MICROSCOPIC FEATURES
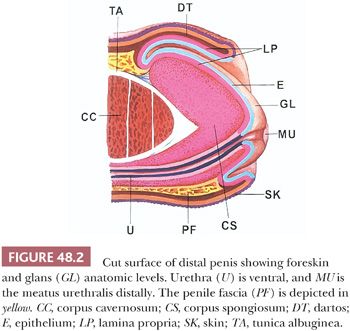
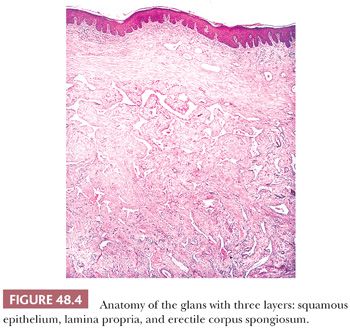
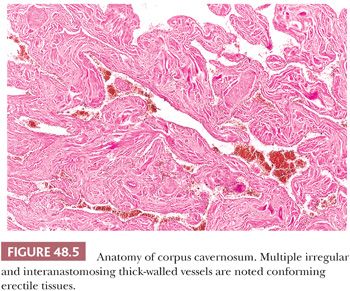
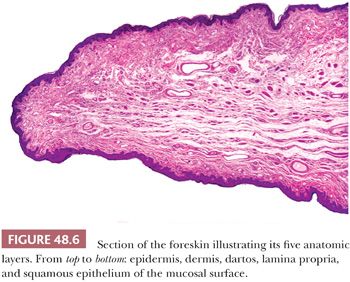
The glans of uncircumcised patients is lined by a 6- to 10-cell layer of nonkeratinizing to slightly keratinized squamous epithelium (Fig. 48.4). Lamina propria is 2 to 3 mm thick and composed of loose connective tissue containing small blood and lymphatic vessels and nerves. Its boundary with corpus spongiosum is not always sharp. The corpus spongiosum consists predominantly of complex and interanastomosed venous sinuses (the erectile tissues) separated by fibrous trabeculae. The thickness of the corpus spongiosum varies from 6 to 13 mm (2,8). The corpora cavernosa, the main component of the shaft, protrudes into the glans in more than two-thirds of the specimens (8). The corpora cavernosa are predominantly composed of thick and interanastomosing erectile vascular structures separated by a complex tridimensional network of trabeculae (Fig. 48.5). The vessel walls are composed of thick bundles of smooth muscle. The vascular structures of the corpora cavernosa are thicker and more complex when compared with those of the corpus spongiosum. The interstitial connective tissue of the trabeculae contains more smooth muscle bundles than in the corpus spongiosum (2). It is important to histologically separate corpus spongiosum from cavernosum because tumor affecting the latter are associated with a higher rate of nodal metastasis. The tunica albuginea is a 1- to 3-mm thick hyaline fibrous sheath surrounding and separating corpus spongiosum and corpora cavernosa. Small nutritional vessels and minute amounts of adipose tissue traverse the tunica from the penile fascia to the erectile tissues, explaining occasional pathways of tumor invasion from the Buck fascia to the corpus cavernosum. The Buck fascia that is present beneath the corporal dartos entirely encases the shaft and extends to the coronal sulcus, where it blends with the connective tissue of the dartos or with the lamina propria. The penile fascia is important because it is highly vascular and composed of loose connective tissue and is a frequent site of tumor extension from the glans and coronal sulcus to the shaft and to the resection margin (see Fig. 48.80) (5). The foreskin shows five histologic layers, which, from the inner to the outer surface, are the mucosal squamous epithelium, lamina propria, dartos, dermis, and epidermis (Fig. 48.6). The skin has a wrinkled and usually pigmented epidermis, underneath which there is the dermis. The dartos is wider and is made of loose connective tissue associated with numerous irregularly arranged bundles of smooth muscle, vascular structures, nerves, and pacinian corpuscles. The mucosal epithelium is nonkeratinizing to slightly keratinized squamous, similar to that of the glans. In adults and especially in the setting of inflammation, the epithelium is often keratinized. Skin adnexa are absent; however, scarce, small sebaceous glands not associated with hair follicles may be rarely identified (2). Mucinous metaplastic cells have been reported in association with chronic inflammation (9). The preputial lamina propria is thin and composed of loose fibrous tissue containing small vessels and nerves. Numerous genital nerve corpuscles (of Meissner) are present in the superficial lamina propria just underneath the epithelium. The anatomic levels in the coronal sulcus vary from three or four (10). From surface to deeper areas, there is a squamous epithelium, lamina propria, dartos, and Buck fascia. The dartos is not present at this site in approximately half of the specimens. When present, it is continuous with the corporal and preputial dartos. The squamous epithelium is often keratinized but not associated with adnexal structures. The lamina propria is identical to that seen in the glans.
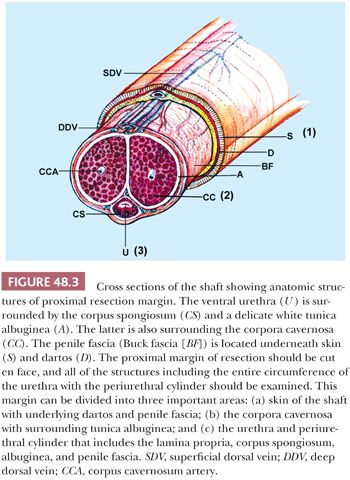
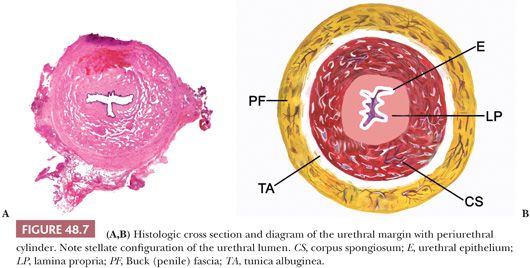
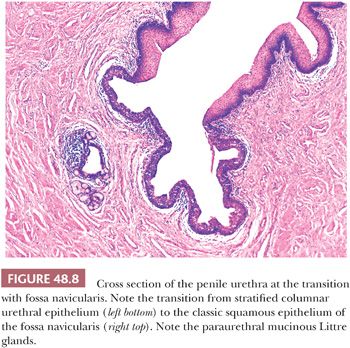
The penile urethra surrounded by periurethral cylinder consists of urethral epithelium, lamina propria, corpus spongiosum, albuginea, and Buck fascia (Figs. 48.3 and 48.7A,B). The penile urethral epithelium is stratified, with a columnar cell layer at the surface (Fig. 48.8). This epithelium is not identical to classic urothelium; umbrella cells are not present (4,11). The distal 5 to 6 mm of penile urethra, which includes the fossa navicularis, shows a nonkeratinizing squamous epithelium continuous to the glans squamous epithelium (Fig. 48.8). Periurethral mucinous Littre glands as well as prostate-specific antigen (PSA)–positive prostatic-like glands and ducts have been described in and around the urethra (12). In the urethra, the presence of squamous epithelium other than in its distal portion should be considered as metaplastic (4).
REGIONAL LYMPH NODES
The inguinal lymph nodes may be classified as superficial and deep. A horizontal line passing through the point where the saphenous vein enters the femoral vein separates these two anatomic compartments. The superficial nodes (~10 to 13) are located above the cribriform fascia (1,11,13). The sentinel nodes are usually part of the group of nodes located at the superior inner quadrant but rarely in other and even deeper sites (13). Deep nodes are scanty, and their lymphatic vessels drain into the pelvic (iliac) lymph nodes, located externally or medially along the major iliac vessels (13,14).
ANOMALIES
Congenital anomalies of the penis are rare, and a wide variety has been described (15). They range from the absolute lack of the organ to segmentary structural anomalies. Penile agenesis or aphallia is a rare condition in which the genital tubercle fails to develop. It tends to be associated with other malformations of the genitourinary tract. Immediate assessment is required to successfully reassign gender (16,17). Conditions in which the penis appears to be absent are concealed penis and webbed penis. In the first, the penis is normally developed but is usually camouflaged under fat in the suprapubic area, scrotum, perineum, or thigh (17,18). In webbed penis, the scrotal skin extends to the ventrum of the penis and hides it.
Hypoplasia and hyperplasia of the penis usually are associated with endocrine abnormalities. Hypoplasias are more common than hyperplasias. In cases of micropenis, the ratio of the length of the penile shaft to its circumference is normal (17). Duplication of the penis or diphallia usually is associated with other genitourinary anomalies such as hypospadias, bifid scrotum, duplication of the bladder, and renal agenesis. The spectrum ranges from a small accessory penis to complete duplication (17). Lateral curvature of the penis is caused by overgrowth or hypoplasia of one corporeal body. In penile torsion, a rotational defect of the penile shaft is present, caused by fibrous tissue surrounding the corpus spongiosum or a short urethra. Chordae usually are associated with hypospadias or epispadias.
Epispadias occurs when the urethra opens on the dorsum of the penis. If the opening of the urethra is in the dorsal aspect of the glans, it is called glandular epispadias; if it is between the pubic symphysis and the coronal sulcus, it is a penile epispadias; if it is in the penopubic junction, it is a penopubic hypospadias. This last type is the most common and is associated with urinary incontinence. Hypospadias occurs when the urethra opens into the ventral aspect of the penis, anywhere from the glans to the perineum. The classification depends on the anatomic location of the defect. It can be glandular, coronal, penile, penoscrotal, or perineal, the most frequent being glandular and coronal. Hypospadias is the most common type of penile congenital defect. The incidence is calculated as 3.2 per 1000 live male births. Associated anomalies include absence of the foreskin, chordee, undescended testis, and inguinal hernias (17,18).
Cysts of the penis are rare. Median raphe cysts result from anomalies in the development of the urethral groove (18,19). They occur in the midline and appear as asymptomatic, translucent subcutaneous masses in the ventral aspect of the shaft. Histologically, they are lined by different types of epithelia according to their embryologic origin: nonkeratinized squamous, pseudostratified columnar, urothelial-type, mucus-producing, ciliated, and apocrine-like epithelium (19,20).
Os penis is the presence of heterotopic bone in the penis; it is usually found in the elderly and is associated with Peyronie disease, but it can also be seen in children (21). In the evolutionary scale, the human species is one of the few mammals whose male genital organ does not normally have an intrapenile bone or bacula.
INFECTIONS
Multiple pathogenic organisms can affect the penis. These organisms can be transmitted sexually or by other means.
BACTERIAL INFECTIONS
Bacterial infections of the genitourinary tract are more frequent in females, except in male newborns, especially if uncircumcised (22). Pathogenic bacteria have a greater propensity to adhere and colonize the mucosal surface of the prepuce; therefore, balanoposthitis is more common in uncircumcised men. Histologically, a nonspecific inflammatory infiltrate is found. Uncommon causes of balanoposthitis caused by Gardnerella vaginalis (23) and Trichomonas (24) have been reported. These infections are sexually transmitted. Gonococcal infections are typically sexually transmitted, but they more frequently produce urethritis. Gonococcal and trichomonal infections have been reported to infect the penile median raphe as well (25,26).
Localized infections of the penis, if not properly controlled, can spread and produce cellulitis. This situation is more common in newborns and immunodepressed patients. Cellulitis usually involves the scrotum and is caused by group A Streptococcus, although group B Streptococcus also has been reported as a causative organism (27). Deep infections of the penis are rare and usually caused by Neisseria gonorrhoeae (28).
Fournier gangrene, a necrotizing fasciitis of the genitalia, perianal, and perineal regions, is a serious and life-threatening condition (Fig. 48.9) (29). The dartos and penile fascia are the preferred sites of penile involvement. Thrombosis of the small vessels, known as obliterative endarteritis, is thought to be a key pathophysiologic event (29). Fournier gangrene is usually a polymicrobial infection. Streptococci and staphylococci are the most common causative agents in children, whereas Gram-negative bacilli and anaerobic bacteria are the most common causative agents in adults (30). The source of the infection may be colorectal, urologic, or cutaneous. The most common predisposing factor is diabetes mellitus.

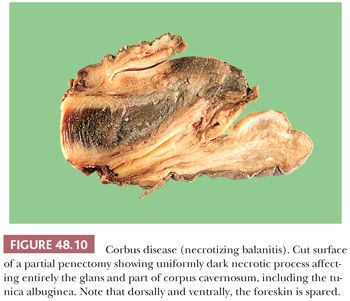
Gangrenous balanitis (Corbus disease), like scrotal Fournier gangrene, is a rapidly progressing necrotizing inflammatory process. It is caused by anaerobic organisms affecting the glans penis. A total necrosis of the glans can be present (31), and unlike Fournier gangrene, which secondarily may affect the penis through corporal fascia or dartos, the foreskin may be spared (Fig. 48.10). Necrotizing gangrene has been described in diabetic patients and associated with penile prosthesis. Mycobacterial infections of the penis are exceptionally rare. Tuberculosis of the penis can present as a primary focus, a direct spread from nearby areas, or hematogenous spread in generalized tuberculosis (32,33). In the past, it was associated with circumcision rituals. Histologic features do not differ from tuberculous granulomas of other sites.
FUNGAL INFECTIONS
Mycotic infections of the penis can be superficial or deep (15,18,34). Superficial infections are caused by dermatophytes and Candida albicans. The former usually infect the penis through local spread from more commonly affected areas such as the groin. C. albicans is usually sexually transmitted and may be carried asymptomatically by 15% to 20% of men. It is believed that this is a factor in recurrent candidal vaginosis. Superficial fungal infections should be especially suspected when neutrophils are present in the squamous epithelium and keratin (often parakeratotic) layer. Deep mycotic infections of the penis, such as cryptococcosis and histoplasmosis have been described, but they are extremely rare. They usually represent hematogenous spread from other primary sites (35,36).
PARASITIC INFECTIONS
Scabies is the most common parasitic infection. It is usually part of a generalized infection. It is caused by the mite Sarcoptes scabiei, hominis variety, an obligate human parasite (34).
SEXUALLY TRANSMITTED INFECTIONS
Syphilis
Syphilis is a sexually transmitted infection caused by the spirochete bacterium Treponema pallidum. The primary route of transmission is through sexual contact but it may also be transmitted from mother to fetus during pregnancy. The disease has four stages, each of which manifest with different signs and symptoms (34,37). The primary stage classically presents with a firm, painless papule that ulcerates, designated as the hard chancre. They are most often solitary. Common sites are the inner prepuce, coronal sulcus, penile shaft, and penile base (34). Secondary syphilis results from hematogenous dissemination of organisms and presents with a diffuse rash, which frequently involves the palms and soles. The anogenital lesion of secondary syphilis is the condyloma lata characterized by soft, flat-topped, moist, red to pale papules; nodules; or plaques, which may become confluent (37). Latent syphilis runs with little to no symptoms and tertiary syphilis with gummas, neurologic, or cardiac symptoms. Syphilis is known as the great imitator due to its frequent atypical presentations. The disease is characterized by anogenital lesions during the primary, secondary, tertiary, and congenital stages of the infection (34,37). Histologically, an obliterative endarteritis surrounded by a predominantly plasmacytic infiltrate is characteristic of the disease. In primary syphilis, the endarteritis can be found at the base of the ulcer. In secondary syphilis, the endarteritis can be superficial or deep and usually is associated with psoriasiform epidermal hyperplasia or spongiform pustular lesions (37,38). The infiltrate composed of plasma cells and lymphocytes may obscure the dermal-epidermal junction. When intraepidermal/intracorneal neutrophils are prominent, the spirochetes tend to be easily identified within the epidermis. Spirochetes can be identified in primary and secondary lesions using Warthin-Starry or Steiner stains. An immunohistochemical stain for T. pallidum is currently available, making easier the identification of the microorganism in these lesions. T. pallidum can also be detected by polymerase chain reaction (PCR). Gummas of tertiary syphilis show granulomatous inflammation with epithelioid and multinucleated giant cells, obliterative endarteritis, and areas of necrosis. Treponemas usually are scant in these gummas and difficult to demonstrate. Reactivation of syphilis in patients infected with human immunodeficiency virus (HIV) is becoming more frequent (39,40), and the affected patients with the disease may show an atypical presentation and course.
Granuloma Inguinale
Calymmatobacterium granulomatis, a Gram-negative bacterium, is the causative agent of granuloma inguinale or donovanosis (34,41). The first clinical manifestation is a small, relatively painless nodule, occurring on the prepuce, glans, penile shaft, or scrotum. The nodule later ulcerates, showing exuberant granulation tissue and pseudoepitheliomatous hyperplasia. Because the lesion spreads by peripheral extension, it may attain a large size. Satellite lesions can be found as pseudobuboes. Histologically, the most important features are (a) massive plasma cell infiltrate in the granulation tissue, (b) diffuse infiltration of neutrophils that form local collections, (c) absence or paucity of lymphocytes, and (d) large mononuclear cells with Donovan bodies. These are large intracytoplasmic, encapsulated, bipolar bodies that are better seen in crushed preparations. The organism does not discolor with hematoxylin and eosin (H&E) stain, but it is well delineated by the Starry-Starry method as short bacilli, either singly or in clumps (42). Electron microscopy reveals that the bacteria reside in phagosomes (41).
Lymphogranuloma Venereum
An obligate intracellular parasite, Chlamydia trachomatis, is the agent associated with this sexually transmitted disease. Lymphogranuloma venereum is manifested by an infrequent primary genital lesion; secondary lymphadenitis with bubo formation; and late infrequent sequelae of fibrosis, edema, and fistula formation (34). Clinically, a painless papule or ulcer appears at the site of inoculation and then rapidly disappears. Within 1 to 2 weeks after the appearance of the primary lesion, enlargement of the inguinal lymph nodes begins.
Histologically, the primary penile lesion shows nonspecific changes. There is ulceration and a nonspecific granulation tissue (42). The inflammatory infiltrate consists of plasma cells and lymphocytes. Nonnecrotizing granulomas composed of epithelioid and a few giant cells surrounded by plasma cells can be seen (42,43). The lymph nodes show focal accumulations of neutrophils in necrotic foci in the early stages. Lymphocytic hyperplasia and massive plasma cell infiltration follow. The lymphocytic hyperplasia can be so pronounced that it can alter the architecture of the lymph node diffusely or create follicular center hyperplasia. The small suppurative foci coalesce and form the classic, although not pathognomonic, stellate abscesses with surrounding epithelioid cells and multinucleated giant cells (43). Sinuses and tracts can develop, and ultimately, fibrosis can be the predominant element in the lymph node. Ordinary histologic stains do not demonstrate the infecting organisms in the skin or node. The diagnosis may be confirmed by culture of a skin lesion or lymph node, and serology is useful (34,43).
Chancroid
Chancroid or soft chancre, a disease caused by a Gram-negative organism, Haemophilus ducreyi, can have several clinical presentations (44). A soft-based painful ulcer is the hallmark. If the ulcer is small, it is called dwarf chancroid; if the ulcer extends rapidly and is associated with a ruptured inguinal abscess, it is a giant chancroid; if there is widespread necrosis and destruction of the external genitalia, it is called a phagedenic chancroid and is caused by a superimposed infection of Fusobacterium organisms (44). Histologically, there is a zonation phenomenon at the ulcer base. The uppermost layer shows necrosis, fibrin, and numerous neutrophils. The middle layer shows abundant granulation tissue with prominent blood vessels, some of which have partial thrombosis. The deepest layer shows an intense plasma and lymphoid cell infiltrate (45).
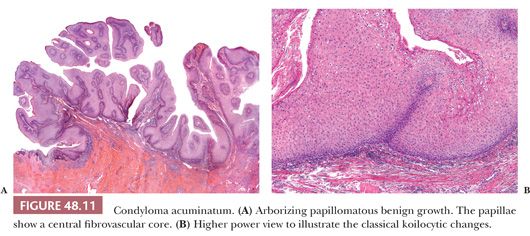
Human Papillomaviruses: Condyloma Acuminatum
Human papillomaviruses (HPVs) are epitheliotropic DNA viruses that infect epithelial cells of the skin and anogenital and oropharyngeal mucosa. More than 100 genotypes have been described, several of which cause specific types of cancers and benign warts (46–49). Genital wart (condyloma acuminatum) is one of the most common sexually transmitted diseases, affecting approximately 20 million people in the United States. Condyloma acuminatum is most often associated with the low-risk types HPV-6 and HPV-11 (50,51). High-risk types of HPV, including 16, 18, 31, 33, 39, 45, 52, 58, and 59, have been linked to cervical, vulvar, penile, and a smaller percentage of oropharyngeal and esophageal carcinomas (see additional discussion in section on penile carcinoma) (46). More than one type of HPV can be associated with a single benign or malignant lesion. Condyloma acuminata tend to affect young adults and are often multiple. They occur on the glans, prepuce, and shaft and may extend into the meatus (11,34) and present as soft, fleshy plaques with cobblestone or filiform appearance. Lesions vary from exophytic cauliflower-like growths to relatively flat and patchy, the latter simulating balanoposthitis (52). They may occur sporadically (usually associated with other genital infections) or in the setting of immunosuppression (53). A high prevalence of papillomavirus-associated penile intraepithelial neoplasia has been found in sexual partners of women with cervical intraepithelial neoplasia, and the female partners of male patients with condyloma acuminata have been shown to have an increased risk of cervical HPV infection and intraepithelial neoplasia (54–56). It is important to recognize that there are clinical and subclinical HPV infections and a significant proportion of them are totally asymptomatic (55,57–61). Clinical methods of viral detection include visual examination, application of acetic acid, peniscopy, and brush cytology (61–62). Pathologic methods of virus identification are immunohistochemistry, in situ hybridization (ISH), and PCR (62–67). Microscopically, condylomata acuminata are exophytic lesions characterized by acanthosis, papillomatosis, and a sharp fairly regular bulbous base (Fig. 48.11A). The surface of the lesion shows hyperkeratosis and parakeratosis. The papillae frequently show an arborescent pattern with prominent central fibrovascular cores; however, a less papillomatous and more rounded growth pattern often showing horn pseudocysts, similar to seborrheic keratosis, is not infrequent. Sessile (flat) and inverted patterns are less frequent. The epithelium shows normal maturation with no atypias. The hallmark of the lesion is the presence of cytopathic viral effect, namely koilocytosis (Fig. 48.11B) (68). These changes tend to be more prominent on the upper levels of the epithelium. Koilocytes have enlarged, wrinkled nuclei surrounded by a perinuclear halo. Binucleated and multinucleated forms and dyskeratotic cells may be seen. It is necessary to distinguish true koilocytes from the vacuolated, glycogenated keratinocytes of mucosal epithelia. Normal vacuolated keratinocytes do not show enlarged nuclei with irregular contours and are not binucleated or multinucleated. The koilocytic changes are more difficult to detect in old lesions that can be confused with seborrheic keratosis. Interestingly, it has been demonstrated that in genital locations, lesions with features of fibroepithelial polyps and seborrheic keratosis without koilocytosis are often associated with HPV (69,70).
Penile condylomas may reach large sizes (>8 cm) and, after many years of neglect, may become locally destructive (giant or atypical condyloma) or may harbor foci of evolving carcinoma (11,71). It is important to keep in mind, however, that condylomata previously treated with podophyllin may display prominent degenerative changes such as vacuolization (pallor of the epithelium), nuclear enlargement, numerous necrotic keratinocytes in the lower half of the epidermis, and increase in the number of mitotic figures (metaphase arrest) (72). Care should be taken not to confuse them with carcinoma. These degenerative changes tend to be focal, and atypical mitoses should not be seen. A high level of suspicion and clinical correlation is necessary to make the correct diagnosis.
Herpes
Herpes is a sexually transmitted disease caused by a DNA virus, the herpes simplex virus (HSV). Most genital infections are caused by HSV-2 (34). It clinically presents with multiple millimeter-sized vesicles that rupture and form painful ulcers. Atypical clinical presentations include fissures, furuncles, linear excoriations, and ulcerations (73). Histologically, there usually are intraepithelial vesicles containing prominent rounded acantholytic keratinocytes. These keratinocytes show the viral cytopathic changes that consist of nuclear ground-glass appearance and molding (68). Multinucleated keratinocytes with the classic nuclear changes are common. Well-defined acidophilic inclusions can also be seen. The diagnosis can be made on Tzanck preparations. Immunohistochemical analysis to identify HSV-1, HSV-2, and herpes zoster viruses is now available.
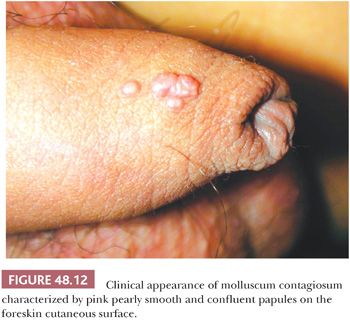
Molluscum Contagiosum
This infection can be sexually transmitted and is caused by a DNA poxvirus. The lesion is a 3- to 6-mm, dome-shaped, pearly papule with central umbilication (Fig. 48.12) (34). Histologically, it shows lobular acanthosis of the epidermis, which causes an inverted pattern of epidermal hyperplasia. Intracytoplasmic eosinophilic inclusions called Henderson-Paterson bodies can be identified in the stratum spinosum and granulosum (68).
Penile Lesion in AIDS
The retrovirus HIV-1 is the agent of AIDS in United States and Europe. The selective replication of HIV within T-helper cells causes their depletion with consequent immunodeficiency. This severe defect in cell-mediated immunity makes the affected individual particularly susceptible to infections. AIDS patients are often concomitantly infected with several different types of microorganisms. Skin diseases (including genital lesions) are common manifestations of HIV infection. Such skin and genital lesions can be classified in noninfective dermatosis, infective disorders, and neoplasms (74–76). Patients with AIDS usually have atypical presentations and more severe dermatosis. Noninfective dermatoses include atopic dermatitis, seborrheic dermatitis–like eruption, psoriasis, genital (aphthous ulcers), and drug reactions. These conditions also tend to be more widespread and severe in patients with AIDS. Histologically, the findings are similar (although frequently more florid) to those seen in patients without AIDS. Plasma cells tend to be numerous in the cutaneous lesions of patients with AIDS.
Infective dermatoses include bacterial, viral, and fungal disorders. HPV-related lesions such as verruca vulgaris and condyloma acuminata are common in such population, and they may be widespread and often associated with preneoplastic and neoplastic HPV-related tumors. AIDS patients are also commonly affected by herpes viral infection (herpes simplex and herpes zoster), molluscum contagiosum, syphilis, Candida, and tinea cruris. Infestations such as scabies can be seen and often presents as the Norwegian variant. Scraping of the lesions will show numerous mites.
AIDS patients also have an increased incidence of neoplastic conditions. The most common tumors in these patients include Kaposi sarcoma and HPV-related squamous cell carcinomas (76,77). Precursor lesions of squamous cell carcinoma (such as bowenoid papulosis and penile intraepithelial neoplasia) are also more frequently found.
MISCELLANEOUS CONDITIONS
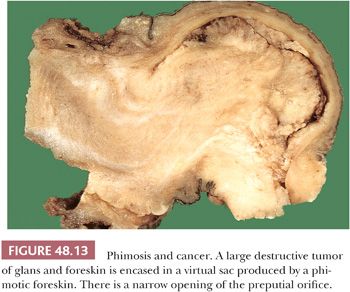
PHIMOSIS
This is a condition in which the prepuce cannot be retracted, usually as a consequence of nonspecific chronic bacterial infections, lichen sclerosus, or congenitally abnormally long foreskin (78). The accumulation of smegma induces a diffuse inflammation of all mucosal epithelial compartments of the glans and foreskin. The treatment of choice is the surgical removal of the foreskin. Histologically, there is fibrosis of the lamina propria associated with a nonspecific lymphoid and plasmacytic infiltrate (79). It is important for the surgical pathologist to liberally sample phimotic foreskin specimens from adults to rule out dysplasia, carcinoma in situ, or occult early invasive carcinoma. Special attention is advised to hyperkeratotic, thick, and slightly elevated or irregular foci. Penile cancer has been reported to occur more frequently in patients with long phimotic foreskins (Fig. 48.13; see Fig. 48.28) (7). In paraphimosis, the prepuce cannot be advanced over the glans and becomes trapped in the space located between the coronal sulcus and the glans corona. Unusual cases of penile infarct secondary to arterial obstruction resulting from edema have been described.
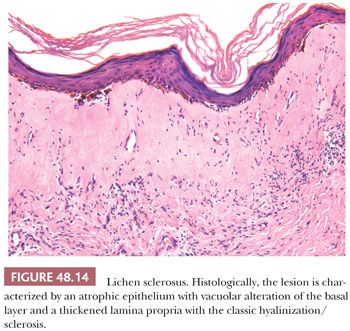
LICHEN SCLEROSUS (BALANITIS XEROTICA OBLITERANS)
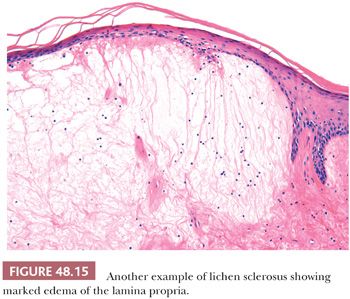
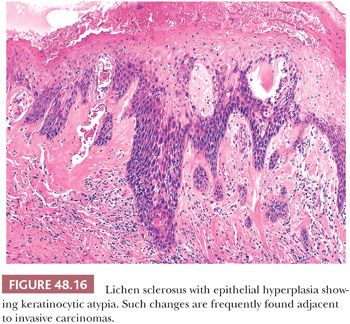
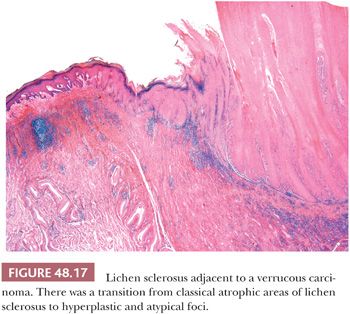
Lichen sclerosus is a chronic and atrophic mucocutaneous condition preferentially affecting anogenital areas of men and women. Extragenital location is less common. This condition was described in the penis as balanitis xerotica obliterans by Stühmer (80) in 1928; however, because some authors prefer to use the term balanitis xerotica obliterans for the end-stage condition and to unify gynecologic and urologic terminology, the use of lichen sclerosus is recommended (81). Penile lichen sclerosus tends to affect middle-aged adults. Grossly, the lesions appear as white-gray, irregular geographic and atrophic areas most commonly compromising the inner aspect of the foreskin, glans, and perimeatal region. Erosion, ulceration, and elevated hyperkeratotic foci may also be seen. In advanced cases, the preputial mucosa folds may disappear, resulting in acquired phimosis or paraphimosis (34). Histologically, the lesions are characterized by an atrophic epithelium frequently intermixed with hyperplastic areas, vacuolar alteration of the basal layer, and a thickened lamina propria with the classic hyalinization/sclerosis (Fig. 48.14). A variable amount of bandlike lymphoid infiltrate is usually seen underneath the area of hyalinization. Because of marked basal cell vacuolar alteration, some cases may show dermal-epidermal cleftings. Marked edema of the lamina propria may precede or coexist with the classical sclerotic changes (Fig. 48.15) (82). Lichen sclerosus is a superficial mucosal disorder preferentially affecting the epithelium and lamina propria and typically sparing the preputial dartos and corpus spongiosum of the glans. The lesions, however, tend to be broad and multifocal, may affect more than one epithelial compartment, and may even extend to the epithelium and lamina propria of the distal urethra (81). Although extragenital lichen sclerosus appears to carry no risk for malignant transformation, the relationship of anogenital lichen sclerosus and squamous cell carcinoma (SCC) is well documented (82–87). In a prospective study, the incidence of SCC arising in the setting of long-standing lichen sclerosus of the penis was 9.3% (85,86). In a retrospective review of 200 penectomy specimens with penile invasive carcinoma, 33% of the cases were associated with lichen sclerosus (81), and this figure was much higher (69%) when considering carcinomas affecting exclusively the foreskin. When present adjacent to invasive carcinomas, lichen sclerosus is almost always associated with areas of epithelial hyperplasia and frequently shows squamous cell atypias (Fig. 48.16) (79). A significant association of lichen sclerosus with special (usually HPV-unrelated) variants of SCC such as usual, pseudohyperplastic, verrucous, and papillary SCCs has been demonstrated (Fig. 48.17). In a recent study, a distinct association of lichen sclerosus with differentiated (simplex) penile intraepithelial neoplasia was found (Fig. 48.16) (87) The frequent coexistence of lichen sclerosus, squamous hyperplasia, differentiated PeIN, and low-grade SCC suggests a common non-HPV–related pathogenic pathway especially for preputial lesions and highlights the importance of circumcision in symptomatic patients for the prevention of penile cancer (87). An analogous lesion, lichen planus, has also been reported in association with SCC, but this relationship appears more controversial (88).
BALANITIS CIRCUMSCRIPTA PLASMACELLULARIS (ZOON BALANITIS)
This is an inflammatory condition of unknown etiology preferentially occurring in uncircumcised men (89,90). Grossly, they are solitary or multiple, well-defined, brown to reddish plaques. The clinical appearance can simulate PeIN. Histologically, there is edema and a dense plasma cell infiltrate associated with lymphocytes and usually siderophages. The epithelium may show mild reactive atypia that needs to be distinguished from PeIN. The diagnosis of Zoon balanitis is largely one of exclusion. One must consider other specific entities such as lichen planus, syphilis, and pemphigoid before making this diagnosis.
PEYRONIE DISEASE
This unusual condition of unknown etiology is characterized by dense fibrosis with formation of a plaque-like lesion affecting the tunica albuginea, penile fascia, and dermis. The fibrosis produces an abnormal curvature of the penis, which is painful during erection. In some cases, there are several firm nodules over the mid dorsal line. Calcification and ossification can be present (91). The condition is more common than originally thought and it may affect up to 9% of the population.
Histologically, its appearance varies with the duration of the disease. Early lesions show a loose proliferation of plum fibroblasts/myofibroblasts admixed with some inflammatory cells (comparable to an early scar). In time, the lesions become more fibrotic and less cellular. Well-established lesions are characterized by hypocellular and hyalinized nodules. The changes in Peyronie disease recapitulate the sequence of events that characterize the development of tissue-scarring fibrosis. These are essentially an initial tissue insult (trauma, microtrauma, or local toxicity), followed by acute and then chronic inflammation that leads to deposition of excessive collagen and other extracellular matrix, fragmentation of elastin, and persistence of myofibroblasts (92,93). Recent experimental findings suggest that increased levels of the profibrotic factor transforming growth factor-β1 (TGF-β1) may play an important role in the pathogenesis of the disease. Injury to the erect penis is thought to trigger the condition by inducing extravasation of fibrin and subsequent synthesis of TGF-β1. Treatment is mainly surgical. Some cases show spontaneous regression. There are currently several promising molecular targets for antifibrotic treatments (92).
TANCHO NODULES AND PARAFFINOMAS
Tancho nodules refer to an unusual custom among some Asian populations to implant foreign material under the skin of the penis to improve sexual pleasure (94). Paraffinomas result from the injection of mineral oil in the penis usually done with the purpose of penile enlargement. Histologically, these materials may cause foreign body reaction that may need surgical resection. Such foreign substances that are injected or inserted into the penis include paraffin, silicone, or wax. A characteristic foreign body reaction called paraffinoma is produced (95). This reaction may occur many years after the injection (96).
PAPILLOMATOSIS OF GLANS CORONA (HIRSUTOID PAPILLOMAS)
This is an asymptomatic benign condition occurring in 20% to 30% of normal men characterized by multiple pearly gray-white fibroepithelial papules located in the dorsal aspect of the glans corona (97,98). These minute papillomas are characteristically arranged in two or three rows. The condition can be confused with condyloma acuminatum, although the diagnosis can be made easily because of the specific location of the lesions as well as the uniformity of the small papules. It was suggested that they may be related to excessive sexual activity. It has been noted that they are more frequently seen in male sexual partners of women carrying an HPV cervical lesion. It is likely that papillomas are not related to HPV infections but, because of the fact that more penises are scrutinized under peniscopy, more diagnoses are being made.
PENILE MELANOSIS
Also called melanotic macules or genital lentiginosis, this condition is clinically characterized by pigmented macules of variable size that may be multifocal and show irregular borders. They may affect the glans and foreskin (34,99,100). Histologically, there is mild acanthosis with hyperpigmentation of the basal layer usually associated with mild lentiginous junctional melanocytic hyperplasia without atypia. Scattered melanophages are often present in the superficial dermis or lamina propria (99). It is considered a benign condition; however, the available information is insufficient to predict the natural history of genital lentiginosis or its relation to mucocutaneous melanoma (100). When associated with lichen sclerosus, there may be superficial fibrosis and pigment incontinence mimicking regression and these findings may be confused with melanoma in situ with regression (101).
SCLEROSING LYMPHANGITIS OF THE PENIS
This unusual and usually self-limited condition preferentially affecting young adults is characterized by firm, subcutaneous, cordlike structure(s) located along the dorsal shaft of the penis or around the coronal sulcus (102,103). The etiopathogenesis is poorly understood, but it has been suggested that it may be associated with trauma and vigorous sexual activity. Concurrent infections including herpes simplex infection have been described, but most likely, they are not the cause of the disease. Because of the difficulty in distinguishing between large lymphatic vessels and veins in this location, there is controversy about whether this condition preferentially affects large lymphatic vessels or veins, and perhaps either could be affected in different patients. This condition may show overlapping features with Mondor phlebitis. Histologically, one or more vessels of the superficial plexus show thickening of the wall, sometimes associated with thrombosis and various stages of recanalization. Inflammation is not prominent.
OTHER RARE CONDITIONS
There are other rare diseases that may present grossly as tumorlike conditions in the penis. Verruciform xanthoma shows a warty-like lesion characterized by acanthosis and hyperkeratosis and parakeratosis. A distinctive feature is the presence of foamy histiocytes between the elongated rete ridges (104). Rare cases of Wegener granulomatosis involving the penis have been reported (105,106). Other rare conditions affecting the penis are inflammatory pseudotumor secondary to chronic catheterization (107) and hyperplastic ectopic sebaceous glands in the foreskin mimicking molluscum contagiosum (108). Cutaneous horn is a clinical term that may be associated with different pathologic entities including warts and SCC. Histologic examination is necessary to achieve a conclusive diagnosis (109,110).
DERMATOLOGIC CONDITIONS THAT INCIDENTALLY AFFECT THE PENIS
A variety of dermatoses can incidentally involve the penis (34). Usually, they are diagnosed and biopsied by dermatologists, not by urologists. Hence, the specimens are submitted to dermatopathologists for histologic evaluation and are rarely seen by the surgical pathologist. Some of these lesions include psoriasis vulgaris, lichen planus, lichen nitidus, fixed drug reactions, allergic contact dermatitis, atopic dermatitis, and lichen simplex chronicus. As part of the Reiter syndrome (urethritis, conjunctivitis, arthritis, and keratodermia blennorrhagica), a balanitis circinata can be noted. These are irregular plaques located in the corona of the penis. For a more detailed description of these entities, see Chapter 1.
NEOPLASMS AND PRECURSOR LESIONS
SQUAMOUS HYPERPLASIA
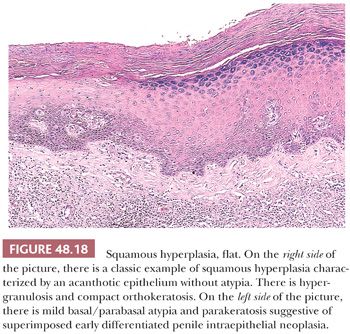
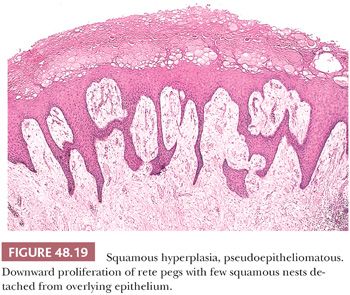
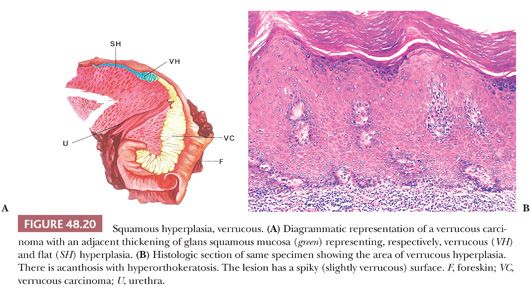
Squamous hyperplasia is characterized by an acanthosis of the squamous epithelium without atypia (Fig. 48.18) (11,111,112). It may be seen as a reactive condition in the context of an inflammatory dermatitis or adjacent to SCCs, particularly usual (keratinizing), verrucous, and low-grade papillary variants. Squamous hyperplasia may involve the glans, sulcus, and foreskin. Grossly, the mucosa is flat, smooth, and pearly white with occasional slightly elevated to papillary configuration, the latter especially seen in areas merging with the adjacent low-grade carcinoma. Microscopically, squamous hyperplasia usually has a flat surface; however, verrucous, papillary, and pseudoepitheliomatous lesions may also be observed. Squamous hyperplasia shows acanthosis, hyper-/orthokeratosis, and normal maturation of squamous cells. Parakeratosis, koilocytosis, deep keratin whorls, and cytologic atypia are not present. Some cases may be associated with lichen sclerosus. Pseudoepitheliomatous hyperplasia may be confused with SCC because the florid complex downward proliferation of squamous rete ridges may appear as detached from the epithelium in cut sections (Fig. 48.19). Important features that may be helpful to differentiate pseudoepitheliomatous hyperplasia from carcinoma include the superficial nature of the lesion, absence of atypia, absence of deep keratin whorls (keratin pearls), and lack of stromal reaction or desmoplasia. Occasionally, hyperplasia of basal cells may be noted, especially in association with the basaloid variant of SCC. Another pattern is that of verrucous hyperplasia, which is typically found adjacent to verrucous carcinomas (Fig. 48.20). The frequent association of squamous hyperplasia with differentiated PeIN and invasive carcinomas, especially low-grade variants, and the usual continuity with the invasive tumor suggest that many lesions labeled as squamous hyperplasia are in fact hyperplasia-like variants of differentiated PeIN (see Figs. 48.16 and 48.17).
PENILE INTRAEPITHELIAL NEOPLASIA
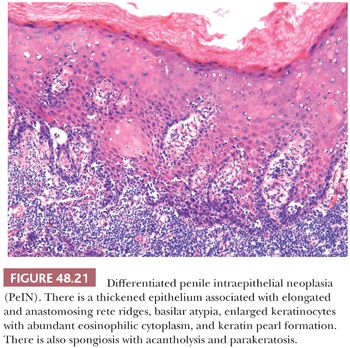
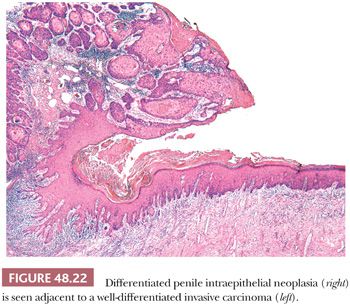
Penile carcinomas mainly show a bimodal pathway of carcinogenesis; therefore, precursor lesions can be broadly classified in two main groups: HPV related and HPV unrelated. Taking into consideration the striking similarities in morphology and pathogenesis between vulvar and penile carcinomas (113–116) and in an attempt to have a simplified and more uniform terminology, we have recently proposed a slightly modified nomenclature for penile preinvasive lesions (116). The term penile intraepithelial neoplasia (PeIN) is preferred over old terms such as squamous intraepithelial lesion (SIL), erythroplasia of Queyrat, and Bowen disease (116–120). These latter two terms are synonymous with carcinoma in situ and have been used for lesions in the glans (erythroplasia of Queyrat) and skin of the shaft (Bowen disease). PeIN can be classified as differentiated/simplex (HPV-unrelated) and undifferentiated (HPV-related) variants. The latter can be subclassified as warty, basaloid, and mixed warty/basaloid. PeINs may be solitary or multifocal and tend to be associated with infiltrating SCCs in approximately two-thirds of cases. In our experience, of these cases, approximately 65% tend to be associated with differentiated PeIN and 35% with warty/basaloid PeIN (116). Differentiated PeIN tends to affect older patients, usually arises in the setting of a chronic scarring inflammatory dermatosis, and is more frequently located in the foreskin when compared with HPV-related variants. The latter tend to affect younger patients and are usually more centrally in the glans and perimeatal region. The gross appearance of PeIN is heterogeneous and does not allow one to distinguish between the two main types. Lesions vary from flat to slightly elevated, pearly white or moist erythematous, dark brown or black macules, papules, or plaques. The contours may be sharp or subtle and irregular. Occasionally, a granular or low papillary appearance may be noted. Microscopically, differentiated (simplex) PeIN is characterized by a thickened epithelium, usually associated with elongated and anastomosing rete ridges, subtle abnormal maturation (enlarged keratinocytes with abundant eosinophilic cytoplasm), whorling and keratin pearl formation (usually in deep rete ridges), prominent intercellular bridges (spongiosis and sometimes acantholysis), and atypical basal cells with hyperchromatic nuclei (116). Parakeratosis is frequent (Fig. 48.21). At low power, the atypia seems to be present only in lower levels of the epidermis; however, at higher power, it is clearer that there is subtle but abnormal maturation in all levels of the epithelium. Despite the subtle changes and in keeping with the gynecopathologic literature, we believe that differentiated PeIN represents a high-grade (although differentiated) lesion that may evolve to frank invasive carcinoma without showing more significant atypias (Fig. 48.22) (116,121). It is not surprising that the precursor lesions of well-differentiated invasive tumors show such a high degree of differentiation. This lesion appears to be the most frequent precursor lesion of penile carcinomas, especially the keratinizing and well-differentiated variants. A preferential association was seen between lichen sclerosus and differentiated PeIN when compared with warty/basaloid variants (see Fig. 48.16). Therefore, it is important to keep a high level of suspicion when dealing with hyperkeratotic/hyperplastic lesions with subtle keratinocytic atypia arising in the setting of long-standing lichen sclerosus.
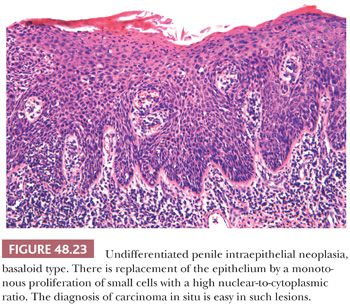
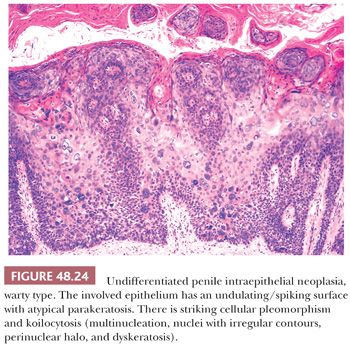
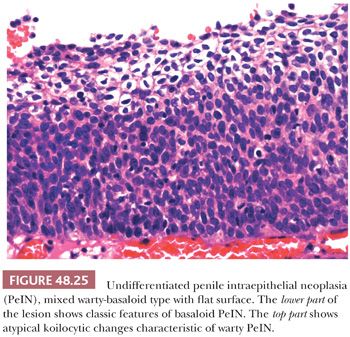
The second major type of PeIN, the undifferentiated, HPV-related type, shows more prominent morphologic changes. It can be subclassified as basaloid, warty, and mixed PeIN. In the basaloid variant, the epithelium is replaced by a monotonous population of small immature cells with a high nuclear-to-cytoplasmic ratio (Fig. 48.23) (111,112,116). Apoptosis and mitotic figures are numerous. Basaloid PeIN should be distinguished from transitional cell urethral carcinoma in situ, which may secondarily involve the penile meatal region (122). In the warty pattern, the involved epithelium has an undulating/spiking surface with atypical parakeratosis. There is striking cellular pleomorphism and koilocytosis (multinucleation, nuclei with irregular contours, perinuclear halo, and dyskeratosis) (Fig. 48.24) (111,112,116). Mitoses tend to be numerous. Frequently, lesions show overlapping features of both, namely warty/basaloid PeIN. These lesions tend to have a spiking surface with koilocytic changes; whereas the lower half of the epithelium is predominantly composed of small basaloid cells (Figs. 48.25 and 48.26). This is not a surprising finding considering that warty and basaloid carcinomas are both HPV-related tumors. Basaloid and warty PeIN can be divided in low-grade and high-grade lesions when the atypical cells occupy less than half or more than half of the epithelial thickness, respectively. Most of the warty and basaloid PeINs will fall within the high-grade category. Full-thickness atypia of the epithelium equals carcinoma in situ. Low-grade lesions are exceptional and should be distinguished from benign condyloma, which is not considered a preneoplastic condition. Occasionally, separate differentiated and undifferentiated PeIN are found in the same specimen.

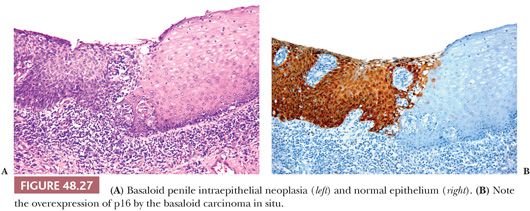
The distinction between differentiated and undifferentiated PeIN is not as challenging as the distinction of differentiated PeIN from other benign/reactive conditions. Because of the subtle histologic changes of differentiated PeIN, there is a great need of molecular and immunohistochemical markers to more easily identify this variant. The use of a triple p16/p53/Ki-67 immunohistochemical panel was found to be helpful in the classification of penile intraepithelial lesions. Squamous hyperplasia tends to be p16 and p53 negative, with variable Ki-67 positivity. Differentiated PeIN are p16 negative and Ki-67 positive, with variable p53 positivity. Basaloid and warty PeINs are p16 and Ki-67 positive (Fig. 48.27A,B), with variable p53 positivity (123–126).
With few exceptions, there is to be a good correlation between the microscopic appearance of the preinvasive process and the associated invasive carcinoma, further supporting the concept of a bimodal pathway of penile tumorigenesis.
BOWENOID PAPULOSIS
Bowenoid papulosis represents a multifocal HPV-related condition affecting the anogenital region of young adults (127). Clinically, penile bowenoid papulosis is characterized by multiple soft papules or macules mostly affecting the skin of the shaft and, less frequently, the epithelium of the glans, sulcus, or foreskin. Despite the clinical benign-looking appearance of these papular lesions, histopathologic findings reveal features of an SCC in situ. There is a proliferation of atypical cells with a high nuclear-to-cytoplasmic ratio that is indistinguishable from carcinoma in situ, especially undifferentiated (warty/basaloid) PeIN. The lesions often show hyperpigmentation of the basal layer. The atypical foci tend to have a patchier and less continuous disposition when compared with carcinoma in situ; however, this is not always the case. Because a definitive histologic distinction between carcinoma in situ and bowenoid papulosis is not possible, clinical correlation is necessary to confirm this diagnosis. Lesions of bowenoid papulosis may regress spontaneously. In some cases (especially in immunocompromised patients), the lesions may be more widespread and may evolve to invasive carcinoma (128). Bowenoid papulosis is most frequently associated with high-risk HPV-16; however, other HPV types and mixed infections have also been reported. (128,129)
SQUAMOUS CELL CARCINOMA
EPIDEMIOLOGY
Penile cancer most frequently affects elderly patients, but age variations are seen with certain histologic subtypes. Basaloid and warty carcinomas appear in slightly younger patients than the other variants. Although rare, penile carcinoma has been reported in young individuals (130–133). Familial cases also have been noted (134). There is no racial preference for penile carcinomas. They have been reported in whites from Europe and North America, Latin Americans, Asians, Africans, Jews, Arabs, native Indians of South America, and African Americans (135–138). Second primary tumors are common in black patients with penile cancer (17.7% of patients) (131). There is a wide geographic distribution, with low frequency in the United States and Europe to higher frequencies in Latin America, Africa, and Asia (except Japan), where up to 20% frequency among male malignant tumors has been reported (138–143). In the United States, elevation rates among white males were seen in midwestern areas, whereas surprisingly low rates were noted in California and southern Florida, which are areas with large Hispanic populations. Although rates were higher among blacks than whites, the data for blacks are too limited for analysis. Reports from Asia and Central and South America are numerous (144–147). Regional differences in prevalence of penile carcinoma are noted in northern and southern Brazil. According to the National Cancer Tumor Registry of Paraguay, penile cancer is the second most common urologic malignancy after prostate cancer. Clinicians in Sweden, Denmark, and Finland have performed extensive epidemiologic studies; no systematic geographic variation has been noted (148). Cancer of the penis is relatively common in Africa, being the most common male cancer in Uganda (138,149). There is wide variation in prevalence in India. The differences in this country do not appear related to circumcision status (Hindus practice circumcision, whereas Muslims do not) (150).
Risk Factors
Uncircumcised men develop penile carcinoma more frequently than those who have had early circumcision (151,152). The risk for penile cancer is 3.2 times greater among men who were never circumcised than in men circumcised at birth (151). Late circumcision does not seem to have the same preventive effect (152). Penile carcinomas arising on circumcision scars in cases of adult circumcision have been described (136). It has been shown that male circumcision is associated with a reduced risk of penile HPV infection and, in the case of men with a history of multiple sexual partners, a reduced risk of cervical cancer in their current female partners (153). Uncircumcised male partners of women with HPV lesions have an increased incidence of HPV infections in the shaft-foreskin (154) and a higher incidence of PeIN compared with uncircumcised men (154). It is clear that when lacking hygienic habits, the foreskin provides a favorable microenvironment for infectious organisms and for the progression of HPV lesions. Penile cancers occur in circumcised males only rarely (127,136,155,156).
A subset of cancer of the penis has been linked to HPVs, with a high preponderance of HPV-16 (46–48,65–67,157–159). In a study of 194 penile lesions from the United States and Paraguay, HPV DNA was detected in 42% of penile carcinomas (67). HPV is more frequently associated with basaloid or warty carcinoma variants (85%). The majority of usual/keratinizing and verrucous carcinomas are HPV unrelated (66,160). There appears to be strong evidence that HPV-16 is involved in penile carcinogenesis; the role of other HPV types remains controversial (46,47,157,158). Molecular studies have shown E6 transcriptional activity and a high viral load in HPV-16 DNA–positive SCCs. Additionally, HPV-16 molecular findings were strongly associated with HPV-16 L1-, E6-, and E7-antibody seropositivity (47).
Numerous reports have linked lichen sclerosus to carcinoma of the penis (83–87,161–165). It is possible that lichen sclerosus represents a precancerous condition for a subset of SCCs, mainly the HPV-unrelated variants (71,84). For a more detailed discussion, please refer to the previous section on lichen sclerosus. The relation between lichen planus and penile cancer remains controversial (88,166).
In a case control study, a significant association was found among smoking, chewing tobacco, and the use of snuff in patients with penile cancer, with a dose–response relationship for the first two. The use of more than one form of tobacco increases the risk (167). Daling et al. (168) found that the adjusted odds ratio for penile cancer associated with current smoking was 2.8 times that of men who never smoked, and it was dose dependent.
Secondary tumors after radiation have been described. They usually are more aggressive than the original tumor (169). Radiation-induced transformation of verrucous to anaplastic carcinoma has been reported (170).
Psoralens and ultraviolet radiation (PUVA) were found to have a strong dose-dependent correlation with penile cancer. When followed for more than 12 years, 14 patients treated with PUVA developed 30 genital neoplasms. The incidence of cancer was 286 times higher than that in the general population and 16.3 times that in patients exposed to low levels. High-dose ultraviolet B radiation increased the risk of genital tumors by 4.6 times compared with controls (171).
A syphilis history is not seen significantly more often in patients with penile cancer than control patients. Syphilis is not related to penile carcinoma (172). Other anecdotal associations reported included Hailey-Hailey disease (173), burn scars (174), asbestos exposure (175), chronic sinus tract (176), hypospadias (177), mineral oil injection (178), and Zoon plasmacellular balanitis (18).
Pathologic Classification
Penile carcinomas can be classified according to patterns of growth and by histologic features. Growth patterns correlate with patients’ outcome. The majority of penile SCCs are histologically similar to squamous cell neoplasms of other organs. Only half of penile SCCs are of the conventional type. The remainders are variants with distinctive clinical, morphologic, and behavioral features. Current subclassification of penile SCCs can be found in the Armed Forces Institute of Pathology fascicle Fourth Series by Epstein et al. (11) on Tumors of the Prostate Gland, Penis, and Scrotum. In this system, penile SCCs are classified in usual; verrucous; basaloid; warty; warty-basaloid; papillary, not otherwise specified (NOS); sarcomatoid; pseudohyperplastic; pseudoglandular (adenoid); adenosquamous; and mixed. In this review, we are adding the newly described papillary variant of basaloid carcinomas (179). Another approach to tumor classification is related to the presence or absence of HPV.
Patterns of Growth
The classification of SCC of the penis according to growth patterns is justified because there is a correlation with prognosis (11,180–182). Approximately one-third of penile tumors show a mixed pattern of growth, principally those of clinically advanced stages. There are four main growth patterns (Figs. 48.28 to 48.31).
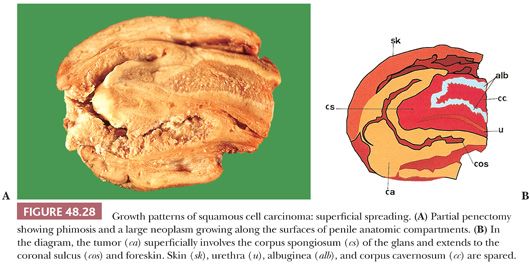
Superficial Spreading. The most common pattern of growth usually corresponds to neoplasms widely involving the superficial anatomic layers of glans, sulcus, or foreskin (Fig. 48.28) (180–182). There are two phases of growth: initially horizontal (mainly involving the epithelium and lamina propria) and in more advanced stages, vertical, with invasion of corpus spongiosum and cavernosum. More than one anatomic compartment is usually affected (i.e., glans, foreskin, and coronal sulcus). Grossly, there is a slightly raised, white-gray, granular firm neoplasm involving epithelial surfaces that on cut surface is mostly limited to superficial layers (Fig. 48.28). Microscopically, the lesion is superficial with an extensive in situ component. Different presentations include (a) predominantly in situ carcinoma, with or without superficial infiltration into lamina propria; (b) predominantly in situ carcinoma, with focal vertical pattern of growth (part of the tumor is nodular and deeply invasive); and (c) carcinoma that is horizontal and bandlike in growth and entirely composed of a mixture of in situ and superficially invasive carcinoma. The histologic variant usually associated with this pattern is SCC of usual type. Because of the centrifugal growth, tumors can extend to urethral or skin surgical margins of resection. Recurrent carcinoma in the glans is not uncommon years after an incomplete removal of a superficially spreading carcinoma of the foreskin.
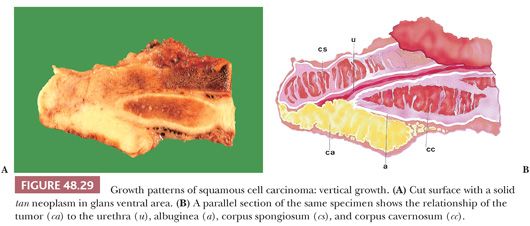
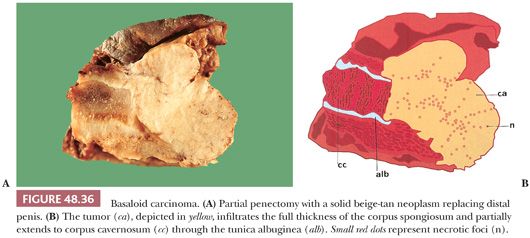
Vertical Growth. The classic presentation is that of a large, ulcerated, and fungating mass that on cut surface shows a solid, deeply invasive nodular appearance (see Figs. 48.29 and 48.36). Microscopically, subtypes associated with this pattern are the basaloid, sarcomatoid/anaplastic, and high-grade usual SCC. There is a high risk of regional metastasis and death (181).
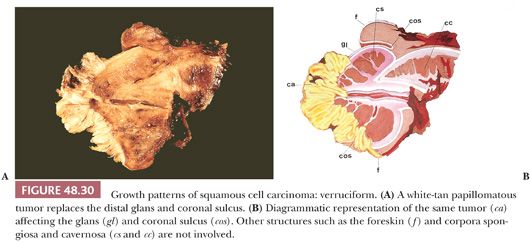
Verruciform. Slowly growing, exophytic, well-differentiated hyperkeratotic tumors with a papillary configuration (Fig. 48.30) (11,180–182). Approximately 25% of penile tumors are verruciform. They are superficial and rarely invade deep structures. This pattern of growth is preferentially associated with verrucous, condylomatous (warty), papillary, and cuniculatum carcinomas. Mixed forms are noted. Benign pseudotumors (verruciform xanthomas) and benign tumors (giant condylomas) may grossly simulate verruciform SCCs.
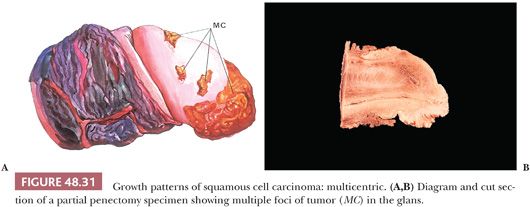
Multicentric. Defined as two or more independent foci of carcinoma separated by benign tissues (Fig. 48.31) (11,181,182). They may be clinically evident or may be a microscopic finding, synchronous or metachronous, and appear in multiple compartments. Histologic subtypes may be similar or dissimilar. Patients are prone to recurrences unless all anatomic compartments are removed at surgery. Any tumor type may present in a multicentric fashion but it is typical of pseudohyperplastic carcinomas.
Mixed. It is not unusual to find a mixture of growths composed of superficially spreading, vertical, and verruciform patterns. Such lesions may also be multicentric. On histologic examination, a combination of low and high histologic grades may be found. A classical example is the hybrid verrucous/SCC of usual type.
Subtypes of Invasive Squamous Cell Carcinomas and Giant Condylomas
Usual. Malignant epithelial tumor composed of squamous cells of variable keratinization and differentiation. Lack of keratinization (pearls or cytoplasmic eosinophilia) is sufficient criterion for exclusion. They harbor no special features. It is the most common type of penile cancer, accounting for 50% to 60% of all cases. The median age is approximately 58 years. Grossly, it appears as an irregular granular mass with a variably flat, exophytic, or even polypoid surface. Large lesions tend to be ulcerated. The cut surface shows a white to tan solid irregular tumor with either superficial or deep penetration into the various penile anatomic layers.
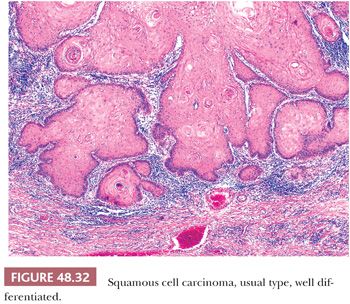
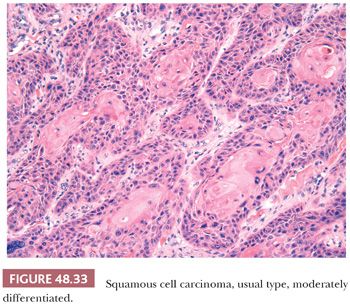
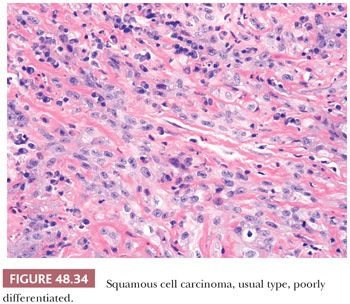
Microscopically, there is an infiltrating keratinizing squamous carcinoma with three differentiation grades (183–185). Well-differentiated (grade 1) tumors are characterized by squamous cells growing in sheets with almost normal to slightly enlarged nuclei and abundant eosinophilic cytoplasm. Intercellular bridges are easily identified, and keratinization is prominent. There is minimal pleomorphism, usually seen near the basal layer (Fig. 48.32). Moderately differentiated (grade 2) carcinomas show a more disorganized growth compared to grade 1 lesions, higher nuclear-to-cytoplasmic ratio, evident mitoses, and although present, less prominent keratinization (Fig. 48.33). Poorly differentiated (grade 3) neoplasms show foci of solid sheets or irregular small aggregates, cords, or nests of cells with little or no keratinization, high nuclear-to-cytoplasmic ratio, thick nuclear membranes, nuclear pleomorphism, clumped chromatin, prominent nucleoli, and numerous mitoses (Fig. 48.34). A tumor should be graded on the least differentiated element, even if this constitutes only a minor component of the neoplasm. Any proportion of grade 3 should be reported (185). When they are the predominant component, it may be difficult to establish the true nature of the neoplasm. In these cases, immunohistochemical studies may be necessary to differentiate these tumors from other less common malignancies such as melanoma and epithelioid angiosarcoma. Transitional cell urethral carcinomas can also be confused with poorly differentiated solid variants of SCC. Urethral neoplasms usually affect the ventral portion of the penis and show no evidence of squamous intraepithelial atypias; the identification of transitional cell carcinoma in situ in urethral epithelium or the history of a previous bladder cancer facilitates the diagnosis.
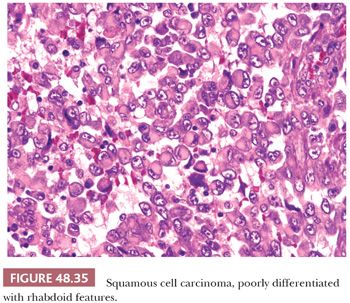
Unusual patterns such as pseudohyperplastic, acantholytic, spindle cell, lymphoepithelioma-like, trabecular, giant cell/pleomorphic, small cell, rhabdoid, and clear cell may be focally seen (Fig. 48.35). The stroma shows a mild to severe inflammatory lymphoplasmacytic infiltrate. Eosinophils are occasionally prominent. Foreign body–type giant cell reaction to the keratin may be noted, especially in highly keratinized tumors. Desmoplasia is unusual. Associated PeIN is present in two-thirds of the cases. Lichen sclerosus can be seen in the adjacent mucosa especially associated with low-grade carcinomas of the foreskin (186).
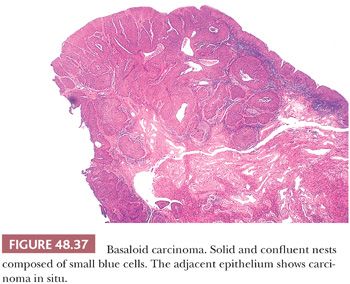
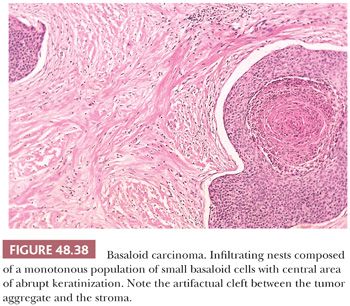
Basaloid. HPV-related, it is composed of small or intermediate basophilic cells with numerous mitoses (187). It accounts for 5% to 10% of all penile cancers; the median age at diagnosis is 52 years. More than half of patients show inguinal metastasis at the time of diagnosis. The glans is the main location but primary preputial tumors also occur. Grossly, there is a rather flat, ulcerated irregular mass. The cut surface shows a solid, tan tissue usually replacing corpus spongiosum, with involvement of albuginea and corpora cavernosa. Necrotic foci within the tumor are noted using a magnifying lens (Fig. 48.36). Microscopically, characteristic solid nests composed of monotonous small tumor cells often with central comedonecrosis are noted (Figs. 48.37 to 48.39). Peripheral palisading may occur surrounded by peripheral clear spaces or clefts; the latter are caused by retraction artifact (similar to what is observed in cutaneous basal cell carcinomas). The cells are small, with a high nuclear-to-cytoplasmic ratio, similar to basal cells, and show inconspicuous nucleoli. Numerous mitoses are characteristic. A starry sky appearance is due to apoptosis (Fig. 48.40). Occasionally, there are pleomorphic cells with larger size. Focal and abrupt keratinization in the central portion of the nest is characteristic. The adjacent epidermis usually shows basaloid PeIN and, less often, warty, warty-basaloid, or differentiated PeIN. The stroma may show chronic inflammatory cells or hyalinization. Perineural, lymphatic, and venous invasion tends to be prominent.
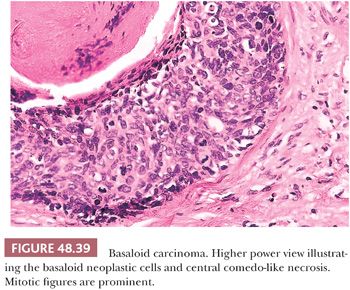
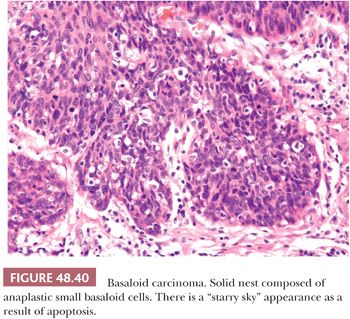
The differential diagnosis is with the usual SCC, distal urethral carcinomas, basal cell carcinomas of the skin, and small cell neuroendocrine carcinomas. Basaloid carcinoma differs from the usual carcinoma by having a distinctive nesting pattern with central comedonecrosis and smaller, more regular cells compared to the larger, more pleomorphic and keratinizing cells of the usual SCC. Keratinization in basaloid carcinomas is abrupt and focal within the center of the nest, whereas it is gradual maturing in the typical squamous carcinoma. Urothelial carcinomas of penile urethra may be composed of small cells and disclose a nesting pattern similar to basaloid carcinoma, but in the former, there is usually more pleomorphism than in the basaloid tumors. The association with a papillary or in situ urothelial neoplasm of the urothelial mucosa, or previous history of blader cancer, may help. Most penile urethral carcinomas probably represent intraluminal implants from a previous urothelial bladder or proximal urethral carcinomas. Immunohistochemical stains with urothelial cell markers (uroplakin III and thrombomodulin) may be used (188). As a consequence of the plastic potential of urothelia, basaloid SCCs may arise primarily in the urethra. They are identical to penile basaloids and distinction is not possible. The distinction of penile basaloid carcinomas from skin basal cell carcinomas may be problematic, but cell from basaloid carcinomas are more atypical in appearance than those of basal cell carcinomas, which characteristically occur in the skin of the shaft in contrast to the mucosal and usually glans location of basaloid carcinoma. An unusual basal cell carcinoma of foreskin inner mucosa has been reported (189). Basaloid carcinomas usually lack the peripheral palisading and myxoid stromal changes characteristic of basal cell carcinomas. Occasionally, in basaloid carcinomas predominates a small cell pattern with trabecular or solid growth in sheets resembling neuroendocrine or Merkel cell carcinomas. The distinction may be difficult and immunohistochemical stains for neuroendocrine differentiation may be necessary.
Basaloid carcinomas are usually diffusely and strongly positive for p16INK4a indicating their relation to HPV. CK 34βE12 (high–molecular weight cytokeratin) is positive in basaloid carcinoma and it is useful for the differential diagnosis with other SCC variants (190). HPV-16 is detected in 71% to 81% of cases by whole tissue section PCR (66,67,191).
Nodal metastases are frequent in patients with basaloid carcinomas. The mortality rate varied from 30% to 60% (187,192).
Warty-Basaloid. They are heterogeneous penile neoplasms with features of basaloid and warty carcinomas in at least 20% of the tumor (Fig. 48.41). Evidence of HPV has been detected in the majority of cases (191). Most tumors are located in the glans but an extension to coronal sulcus or foreskin is present in about two-thirds of cases. Foreskin exclusive location may be noted. Tumors are large and destructive, measuring 2 to 12 cm (mean 5 cm). Grossly, they are exoendophytic. Microscopically, both basaloid and warty components are present (Fig. 48.42A,B), but the basaloid predominates. Two main patterns are recognized: The most common, present in about two-thirds of cases, depicts warty features on the surface and basaloid carcinoma in the invasive portion of the tumor. Both components are separated but mixtures may be present. The second pattern is represented by a nonpapillomatous infiltrative tumor composed of neoplastic nests showing basaloid features at the periphery and warty features at the center. Warty-basaloid carcinomas frequently invade deep erectile tissues. Tumors limited to lamina propria are rare. Vascular and perineural invasion are common (193).

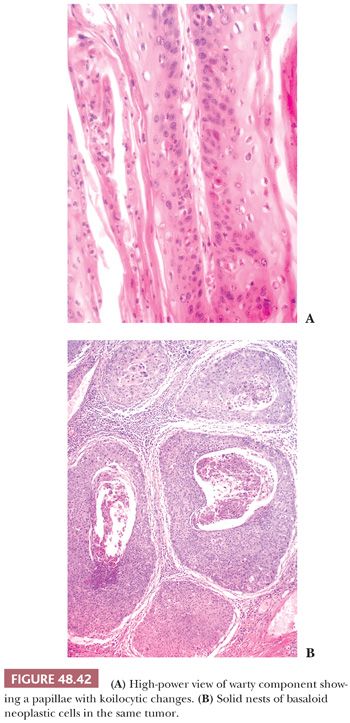
Warty-basaloid carcinomas should be distinguished from the pure forms of warty or basaloid carcinomas. Distinction is based on the relative proportions of the components. Basaloid carcinomas are usually nonpapillomatous and exhibit the typical nesting pattern of growth proper of this tumor. Warty features can be focally observed in basaloid carcinoma but they should not represent more than 10% of the tumor mass (191). A papillary outgrowth is rarely noted on the surface of basaloid carcinomas. The papillae are condylomatous, that is, they have a central fibrovascular core, and lined exclusively by small basaloid cells. This unusual variant should not be confused with a warty-basaloid carcinoma because there is no warty component (193,194). As in the basaloid SCC, in pure warty carcinomas, a basaloid component can be focally present but should not account for more than 10% of the tumor mass. Most warty carcinomas exhibit an exophytic–endophytic pattern of growth, and morphologic features are similar in both components, a helpful feature.
Warty-basaloid carcinomas are more aggressive than pure warty carcinomas but less aggressive than typical basaloid carcinomas. Inguinal nodal metastases are found at presentation in about one-half of all patients. The cancer-specific mortality rate in a study was 33%, and the estimated 5- and 10-year survival rates were about 65%. Clinical behavior is related to the basaloid component, with a high rate of regional metastasis (195).
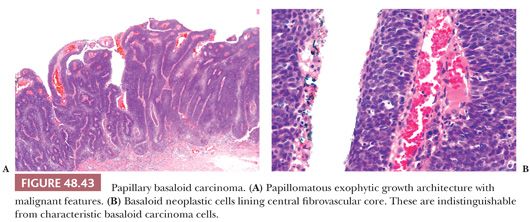
Papillary Basaloid Carcinoma. It is a distinctive HPV-related papillomatous tumor composed of basaloid cells, most likely a variant of basaloid carcinoma. Tumors may be completely papillary noninvasive or harbor an invasive component undistinguishable from classical basaloid carcinomas (179). Patients’ mean age is 66 years; patients with invasive tumors are older than those with in situ lesions. Glans is the most common site but the foreskin may also be exclusively affected. Grossly, tumors are exophytic and papillomatous. Microscopically, papillae are straight, foliaceous, or rounded, distinctively composed of a central fibrovascular core, resembling condylomatous tumors or high-grade papillary urothelial cell neoplasms (Fig. 48.43A,B). Although clear cells, koilocytic-like changes may be observed near the keratinized surface; unlike typical condylomata, these cells show malignant features. The cellular population lining the papillae is uniform, with scant pleomorphism throughout the epithelium, and tumor cells are similar to those observed in basaloid PeIN, high-grade papillary urothelial carcinoma, or invasive basaloid carcinoma. The interface between tumor and stroma is variable from well-defined noninvasive borders to in situ to deeply invasive. HPV is detected in the majority of cases and p16 is usually strongly positive.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


