
37
Pelvic Viscera
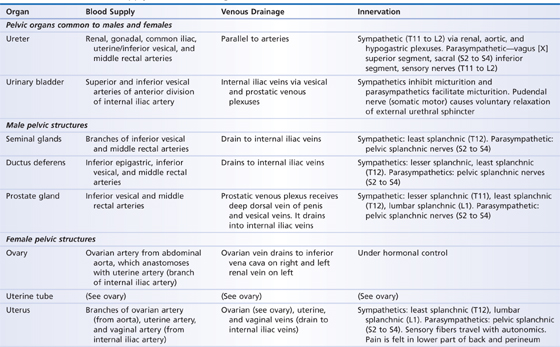
The pelvic viscera include the urinary bladder, distal end of the ureters, rectum, and reproductive organs (Table 37.1, Figs 37.1 to 37.4). Structural support for the pelvic viscera is provided by the bones and ligaments of the pelvis (see Chapter 36).
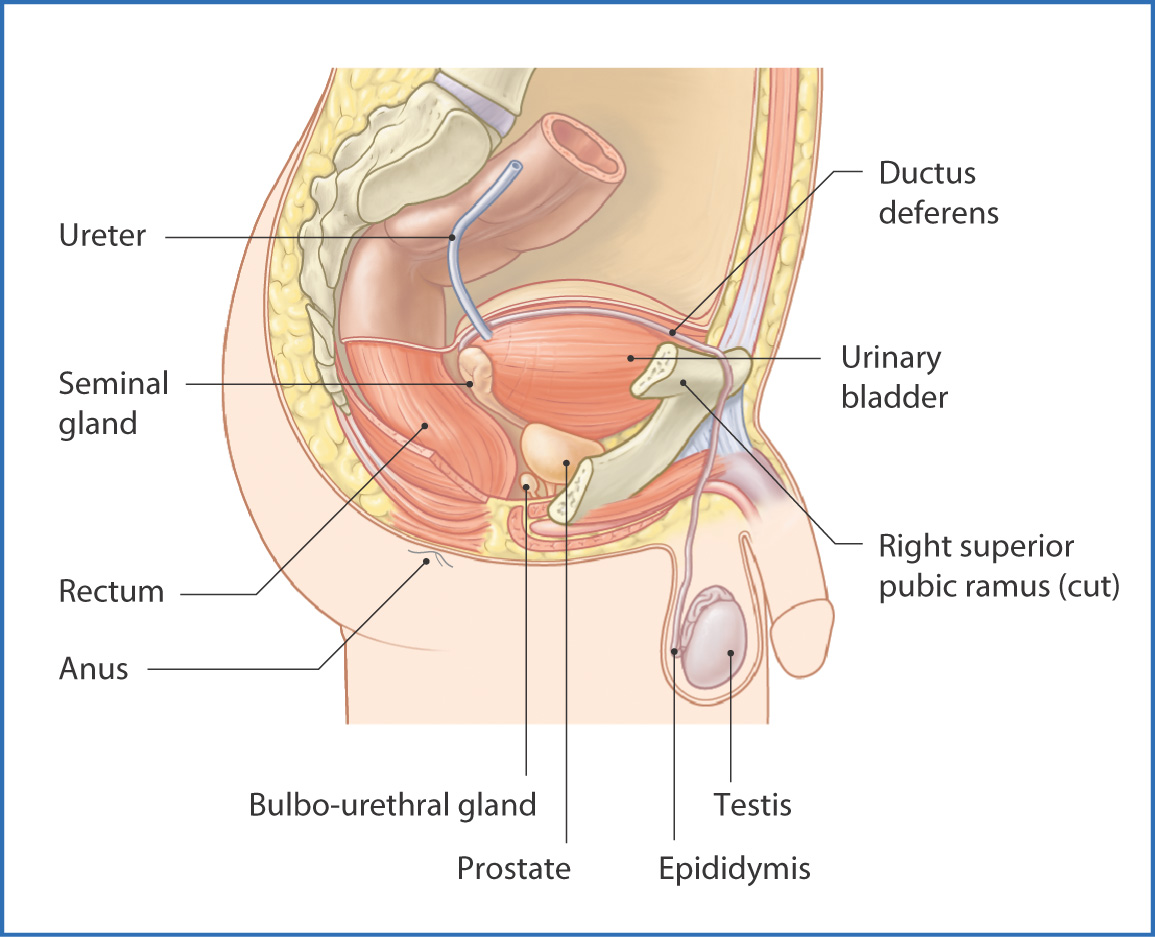
FIGURE 37.1 Male pelvic viscera.
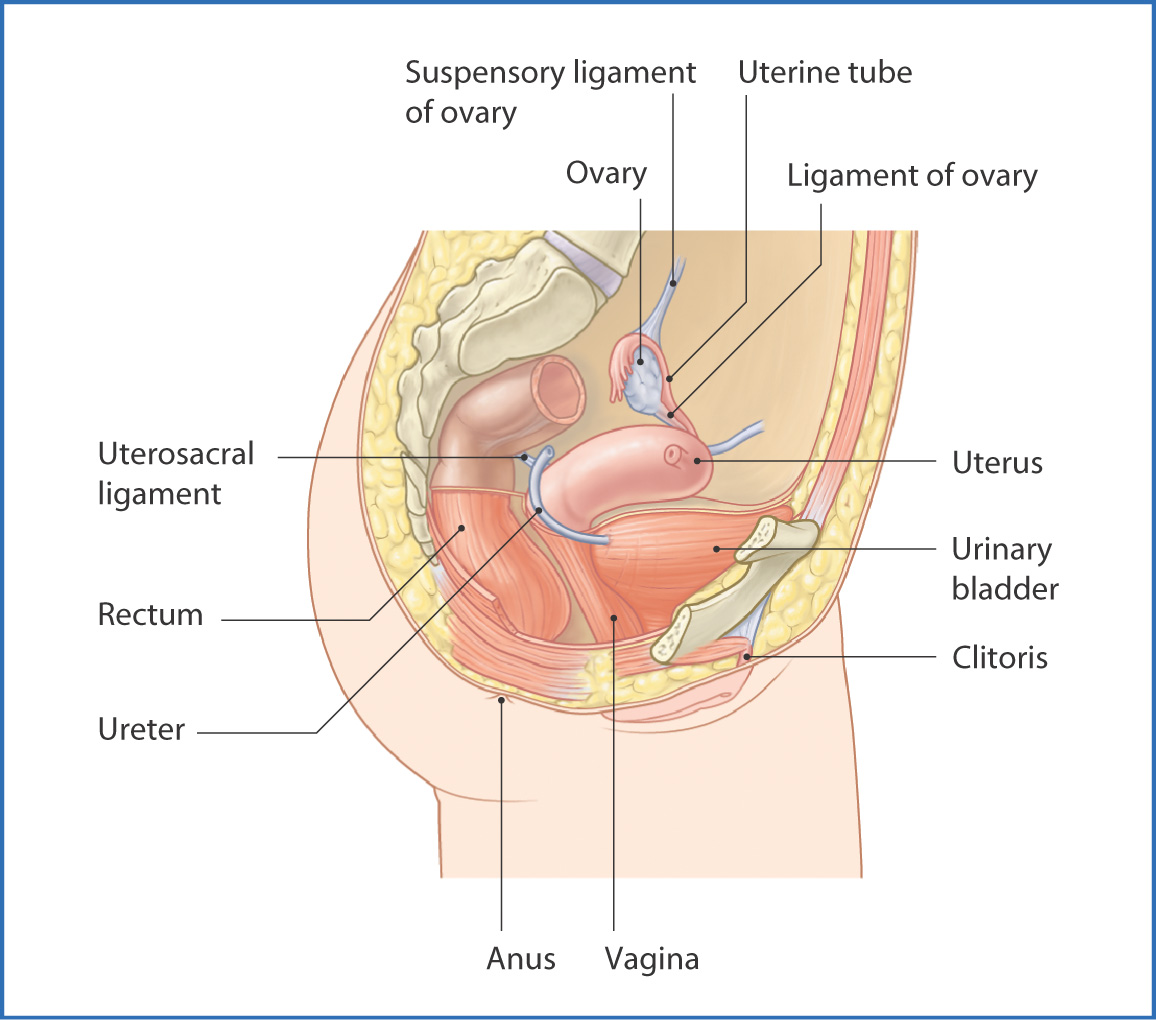
FIGURE 37.2 Female pelvic viscera.
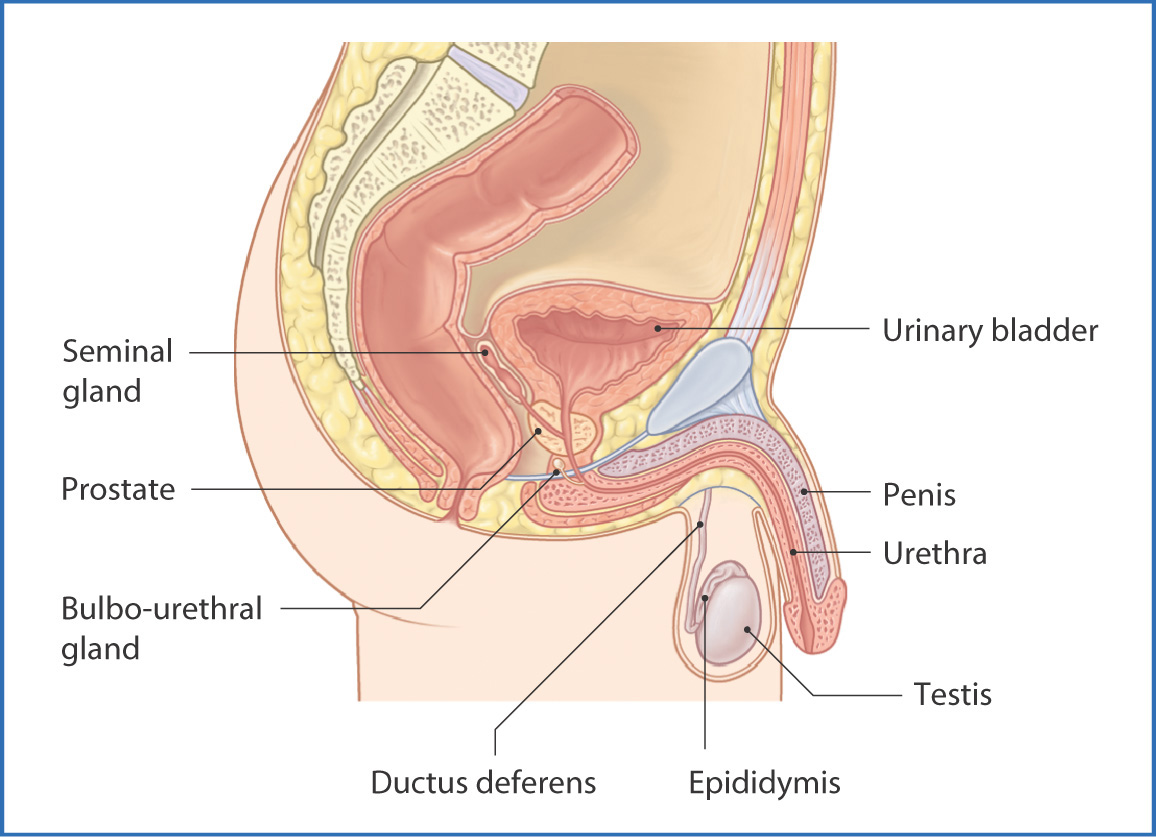
FIGURE 37.3 Male pelvic viscera—median sagittal section.
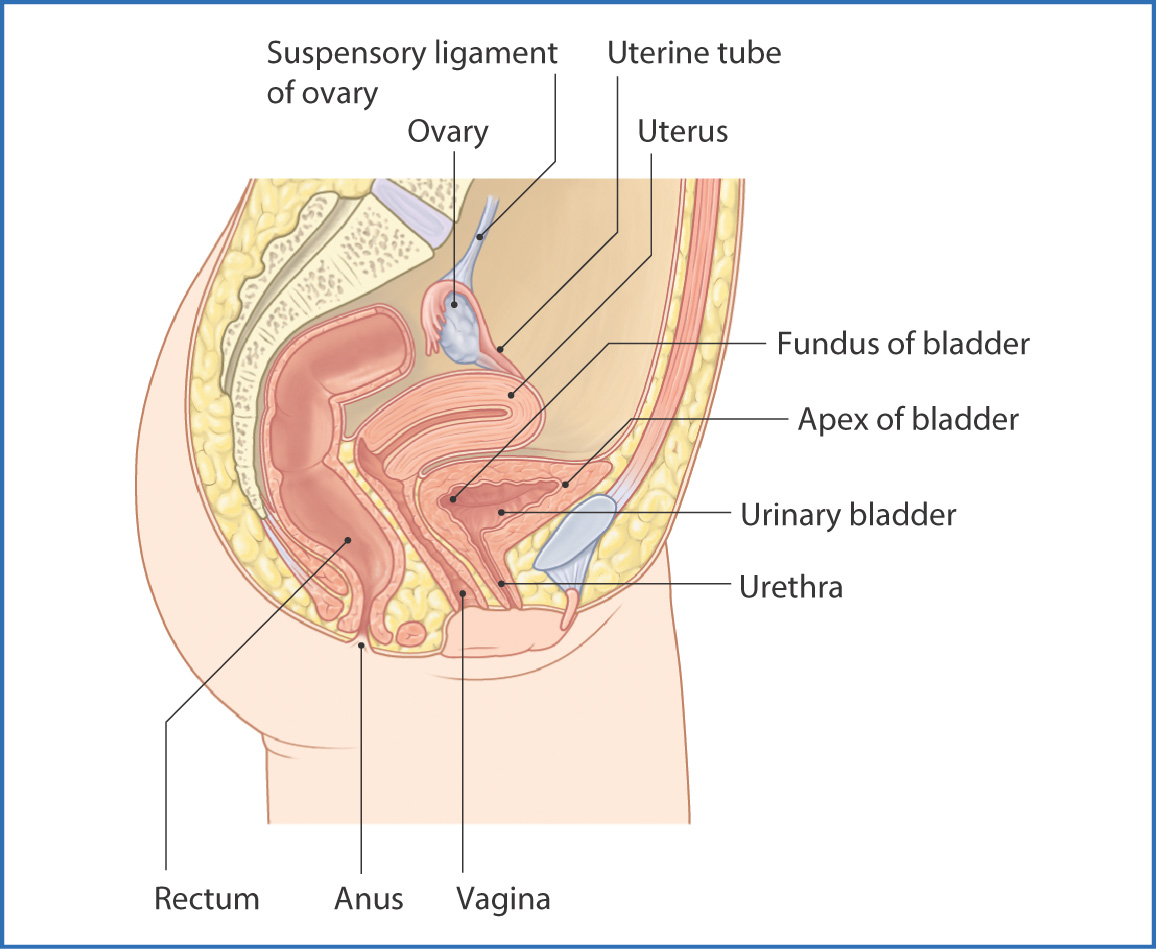
FIGURE 37.4 Female pelvic viscera—median sagittal section.
TABLE 37.1 Neurovascular Supply of the Pelvic Organs
The urinary bladder, the inferior part of the two ureters, and the urethra are contained within the pelvis.
The ureter is a long retroperitoneal muscular tube that transports urine from the renal pelvis of the kidney to the urinary bladder. Descending from the posterior abdominal wall, the ureters become pelvic structures when they cross the bifurcation of the common iliac artery. The ureter is
- anterior to the internal iliac arteries within the pelvis
- in men, posterior to the ductus deferens, which crosses it superiorly near the bladder
- in women, medial and inferior to the uterine artery, which crosses it anteriorly and superiorly in the base of the broad ligament
- in men, posterior to the ductus deferens, which crosses it superiorly near the bladder
The ureters are constricted at the uteropelvic junction, pelvic inlet, and bladder entrance.
The ureters are innervated by the autonomic nerve plexuses along their path to the bladder: renal, aortic, superior hypogastric, and inferior hypogastric plexuses. The blood supply to the pelvic part of the ureter is from adjacent branches of the common and internal iliac arteries. The main blood supply in females is from the uterine artery, whereas in men blood is supplied by the inferior vesical artery. Venous drainage accompanies the arteries and empties toward the iliac veins. Lymphatic drainage is to the common iliac, external iliac, internal iliac, and lumbar lymph nodes.
The sac-like urinary bladder has strong muscular walls (the detrusor muscles). The apex of the bladder is at the superior edge of the pubic symphysis and is attached to the umbilicus via the medial umbilical ligament. The base (fundus of the bladder), created by the posterior wall of the bladder, is attached to the seminal vesicles and rectum in males and to the uterus and vagina in females. The rest of the bladder between the apex and fundus is the body of the bladder. The superior surface of the bladder is covered with peritoneum. The ureteral openings are located at the posterior superior edge of the fundus of the bladder, and the urethral opening is at the midline inferior anterior part just below the apex of the bladder.
The urinary bladder is a reservoir for urine transported from the kidneys via the ureters. When it is full, parasympathetic nerve fibers cause the detrusor muscle to contract and the urethral sphincter to relax. This can be suppressed voluntarily. Parasympathetic innervation is provided by pelvic splanchnic nerves. Sympathetic fibers are from the sympathetic trunk (levels T11 to L2). These nerves converge on the bladder to form the autonomic vesical plexus.
Blood supply to the bladder is from the superior vesical artery (a branch of the inferior mesenteric artery), and blood drains into the internal iliac veins. In addition, a smaller vesical venous plexus forms a network of small unnamed veins around the bladder. The vesical venous plexus also drains into the internal iliac veins.
Lymphatic drainage of the bladder is toward the superior surface of the bladder. From this point, lymph drains into the external iliac nodes. Lymph from the fundus of the bladder drains into the internal iliac nodes.
The urethra exits the bladder via the internal urethral orifice. From here, urine flows to the external urethral orifice. In men, the urethra is 18 to 20 cm long, whereas in women it is only 4 cm. Innervation in men is provided by the prostatic nerve plexus; in women, it is from the pudendal nerve. Blood supply in men is from prostatic branches, which are branches of the inferior vesical artery (a branch of the internal iliac artery) and middle rectal arteries (branches of the inferior mesenteric artery). In women, blood is supplied by the internal pudendal and vaginal arteries, which are both branches of the internal iliac artery.
The rectum is described as part of the gastrointestinal tract and is discussed in Chapter 33.
Male Pelvic Viscera
The male pelvic viscera (prostate, seminal glands, bladder, and rectum) have a role in sexual activity, reproduction, urination, and defecation (see Figs 37.1 and 37.3).
The prostate is a small, solid, ovoid gland (usually around 3 cm long) through which the first part of the urethra passes. It contains five lobes. Four are glandular and produce secretions that are added to the ejaculate during intercourse and orgasm (posterior, median, and paired lateral lobes). A fifth fibromuscular lobe is anterior to the urethra. Fluid, which is cloudy and milky in color, passes from the prostate to the urethra through several (usually 20 to 30) small prostatic ducts and usually accounts for approximately 20% of the volume of semen. The prostate is surrounded by a thin capsule, a prostatic venous plexus, and pelvic fascia (false capsule). It is supported by the pubococcygeus muscle and the puboprostatic ligaments.
The prostate gland is inferior to the urinary bladder at the base of the penis within the pelvis (intrapelvic) and postero-inferior to the pubic symphysis. Because of its position between the bladder and rectum, the posterior part of the prostate can be partly examined by digital rectal examination to detect abnormalities, such as tumors.
Parasympathetic innervation to the prostate is from pelvic splanchnic nerves (S2 to S4); sympathetic innervation is through nerve fibers that originate in the inferior hypogastric plexus.
Blood supply to the prostate is provided by the prostatic arteries (small branches of the inferior vesical artery), the middle rectal artery, and the internal pudendal arteries (branches of the internal iliac artery). Venous drainage is to the prostatic venous plexus, which drains toward the inferior vesical venous plexus and internal iliac veins. Lymphatic vessels from the prostate gland drain toward the internal iliac and sacral nodes.
The two seminal glands
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


