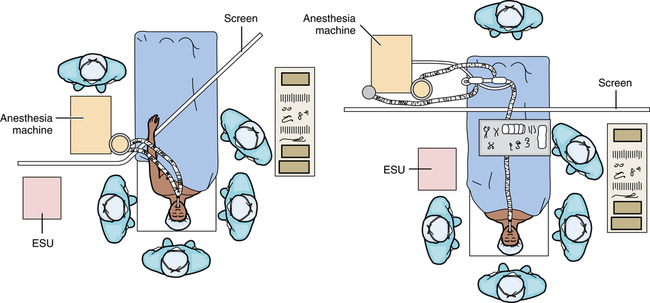
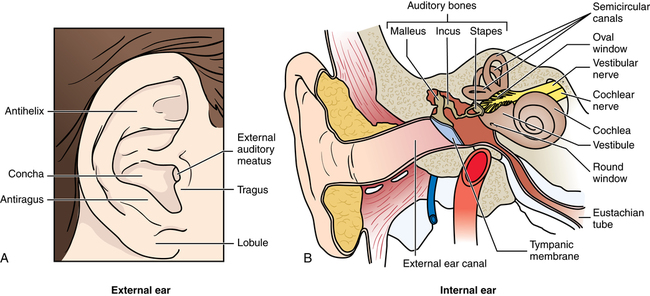
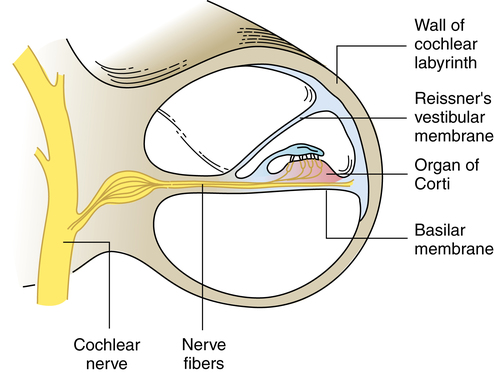
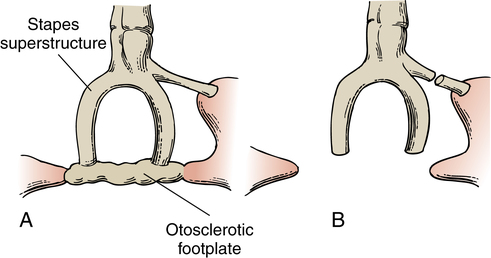
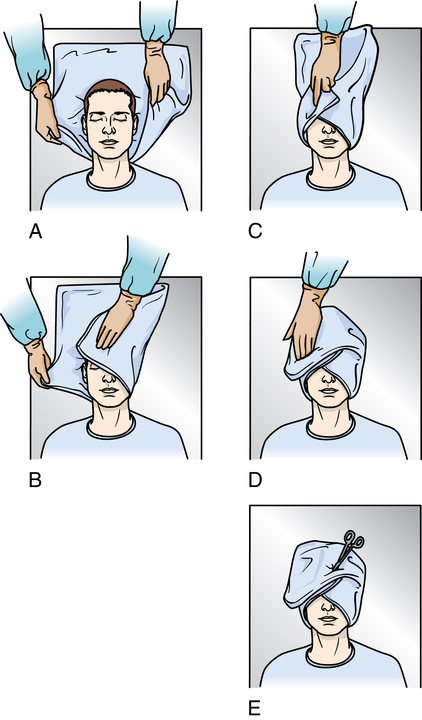
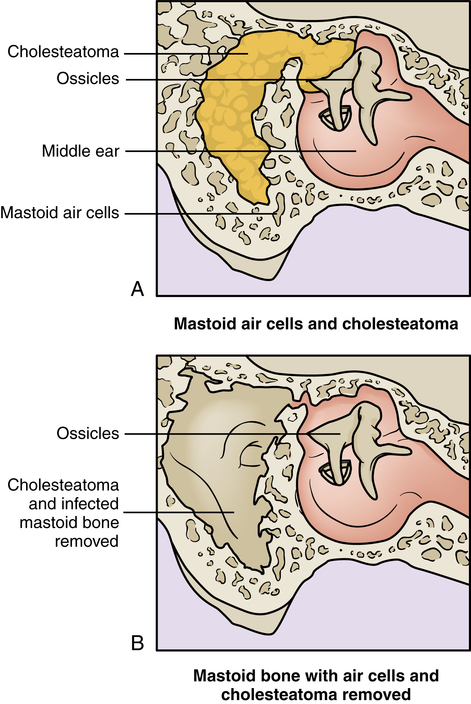
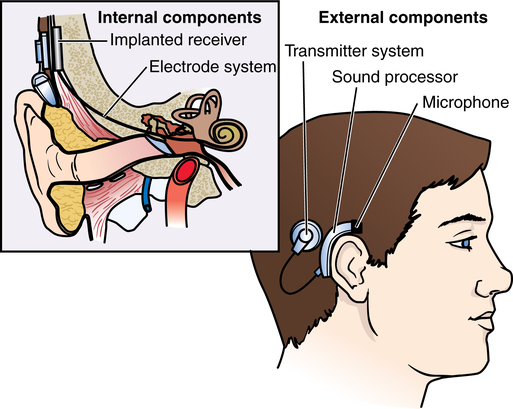
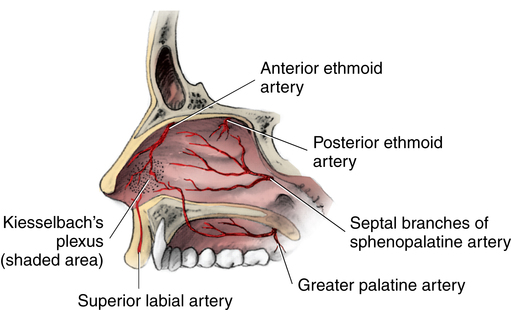
Chapter 41 After studying this chapter, the learner will be able to: • Identify the pertinent anatomy of the ear, nose, and throat. • Describe the care of the patient having an otorhinolaryngologic procedure. • List the main types of hearing loss and the treatments. • Discuss the psychologic effects of head and neck surgery. • List the precautions of caring for the patient with a tracheostomy. Specific considerations include the following: 1. Preoperative explanations and postoperative instructions are vital to the outcome. For example, after ear or nasal procedures the patient must avoid blowing the nose, which would force air up the eustachian tube, potentially causing infection; force air through the incision; or dislodge a graft. To sneeze, both the nose and mouth should be open. 2. Communication is a major problem for patients with loss of hearing or voice. Touch is an effective means of conveying concern and letting the patient know he or she is not abandoned. Pencil and paper or a Magic Slate can be useful for the patient to communicate. The anesthesia provider requires periodic access to the patient’s head and neck, as do the surgeon and sterile team. Positioning of the OR bed must provide space for the anesthesia machine and other equipment, such as the microscope. The anesthesia machine may be positioned near the patient’s side or feet. The endotracheal tube is taped to prevent becoming dislodged during the procedure; all connections must be tight, and tubes must be unkinked. Breathing circuits may need an extension hose if the anesthesia machine is at the foot of the OR bed. The anesthesia provider usually sits alongside the OR bed near the lower half of the patient on the opposite side of the surgeon (Fig. 41-1). Provisions are made for the anesthesia provider to have access to the intravenous (IV) line when the patient’s arms are tucked in at the sides. Extension IV tubing is used. Epinephrine in a local anesthetic, such as lidocaine, is frequently used as a vasoconstrictor in ENT procedures. Cocaine 4% provides local anesthesia and vasoconstriction when used topically on the surgical site. Cocaine can systemically block the effects of epinephrine and should be applied first and allowed to take effect. The epinephrine in the local anesthetic can cause cardiac dysrhythmias, and the anesthesia provider should be alerted when it is injected.7 Nitrous oxide diffuses into the middle ear, causing pressure. During ear procedures, such as tympanoplasty, the nitrous oxide is decreased or discontinued once the tympanic graft is placed to minimize inner ear pressure that could displace the graft.7 Some surgeons prefer a turban-style head drape. Figure 41-2 depicts the method used to create a turban from a drape. Patients undergoing local anesthesia may wear pajama-type bottoms or underpants to the OR in some facilities. Patients having general anesthesia should wear only a gown. The structures of the outer and inner ear (Fig. 41-3, A and B) are concerned with two functions: 1. Hearing (i.e., receiving sound, amplifying it, and transmitting it to the brain for interpretation) Anatomically, the ear is divided into three parts: external, middle, and inner. Hearing affects the quality and quantity of interpersonal interactions. It is a major sense for communicating within one’s environment.5 Loss of hearing therefore affects social relationships. The type of deafness or hearing loss in varying degrees may result from the following: 1. Disease, such as otosclerosis, in which changes in the bony capsule of the labyrinth occur. Otosclerotic bone invades the stapedial footplate, resulting in its fixation and ultimate inability to vibrate in the oval window. Hearing loss is gradual but progressive. This type of deficiency can be surgically corrected when auditory nerve endings are not destroyed. 2. Trauma, such as a perforated eardrum, requiring repair to restore function and aerial ratio. 3. Infection, usually controlled by antibiotics. Although it is more common in children, infection may also occur in adults. It may cause accumulation of fluid in the middle ear. Mastoiditis results from extension of otitis media. a. Serous otitis media may result from obstruction of the pharyngeal orifice of the eustachian tube. If blocked, for example, by hypertrophied adenoid tissue, infection, or allergic swelling, the eustachian tube is unable to equalize pressure because air cannot enter the middle ear from the pharynx. The vacuum or negative pressure thus created causes serum to be drawn into the tympanic cavity from blood vessels in the middle ear mucosa. Recurrent otitis media may require drainage of purulent exudate if conservative treatment fails. b. Acute otitis media may require drainage of purulent exudate if conservative treatment fails. c. Chronic otitis media with or without mastoiditis may follow recurrent otitis media with tympanic membrane perforation. It can produce a chronically draining ear. Measurements that compare bone conduction with air conduction are important in differential diagnosis. Bone conduction refers to hearing as transmitted through the skull; air conduction refers to transmission of sound waves from the tympanic membrane to the inner ear via air. Hearing loss caused by a defect in the external or middle ear, referred to as conductive loss, is a mechanical obstruction of air conduction that usually can be helped by surgical intervention. When the decrement is in the inner ear, referred to as perceptive or sensorineural loss, damage to nerve tissue and/or sensory paths to the brain is not benefited by a surgical procedure. Cochlear nerve endings are the main component of sensorineural hearing (Fig. 41-4). 1. Local anesthesia may be used for a minor procedure on the external ear, but general anesthesia generally is used to avoid patient movement while the surgeon is manipulating delicate structures in the middle or inner ear. a. Inhalation anesthesia may be given by facemask for a short procedure, with the anesthesia provider seated at the head of the OR bed. b. The anesthesia provider sits alongside the OR bed with the patient facing him or her when the patient is intubated for a major procedure. c. Hypotensive anesthesia may be employed to create a bloodless field, especially during microsurgery. d. Nitrous oxide is discontinued before placement of a graft in the middle ear to minimize the risk for increased pressure in the inner ear. e. General anesthesia may be supplemented with a local agent in some procedures, often with epinephrine to control bleeding. 2. The patient’s head is turned with the affected side up and stabilized in a donut. The pinna on the unaffected side should be protected from pressure. 3. Lint-free drapes are preferred. It is mandatory that gloves be free of powder and lint. The formation of a powder granuloma in the oval window can cause irreversible sensorineural hearing loss. 4. The operating microscope is used for many otologic procedures. a. The surgeon sits at the head of the OR bed to use the microscope. b. Microinstruments should be carefully handled before, during, and after use. 5. Compressed absorbent patties (cottonoids) moistened with normal saline solution, rather than gauze sponges, are frequently used. They must be counted. 6. Hemostasis may be achieved with epinephrine, absorbable hemostatic sponges or oxidized cellulose, laser, and bone wax. 7. Prosthetic devices should be available in an assortment of types and sizes. Tissue allografts may be used. 8. A nerve stimulator may be used to identify facial, acoustic, cochlear, and/or vestibular nerve branches. Evoked potential audiometry also may be used to monitor the seventh and eighth cranial nerves. 9. Bone instruments, including powered drills, are used for opening the temporal bone. 10. CO2, Nd:YAG, argon, and KTP lasers are used during otologic procedures to control bleeding, divide nerves, and/or vaporize tissues. 11. Pressure dressings are usually applied. Some surgeons place 1 drop of phenylephrine (Neo-Synephrine) in the ear canal postoperatively. Mastoidectomy, the eradication of mastoid air cells, may be indicated to relieve complications of acute or chronic mastoiditis. Mastoidectomy is more commonly performed in conjunction with a reconstructive procedure (see “Tympanomastoid Reconstruction”). A cholesteatoma can form after repeated infections (Fig. 41-5). 1. Type I (myringoplasty) is closure of a perforation in the tympanic membrane caused by infection or trauma. The ossicular chain is normal. Autologous fascia or a vein is used to repair the perforation. A vein graft is taken from the patient’s forearm or hand. Fascia, more commonly used as a patch over a perforation, is obtained from the temporalis muscle. 2. Type II is closure of a perforated tympanic membrane with erosion of the malleus. The graft is placed against the incus or remains of the malleus. 3. Type III replaces the tympanic membrane to provide protection for the stapes and round window. The tympanic membrane, malleus, and incus have been destroyed by disease. The stapes is intact and mobile. A homograft of tympanic membrane with attached malleus and incus is placed in contact with the normal stapes, permitting transmission of sound. 4. Type IV is similar to type III except that the head, neck, and crura of the stapes are missing. The mobile footplate may be left exposed with the graft placed around it. The air pocket between the graft and the round window provides sound protection for the round window. To conserve the middle ear hearing mechanism, homograft transplantation of tympanic membrane and ossicles may be used to rebuild the chain. 5. Type V is similar to type IV except that the stapedial footplate is fixed because of otosclerosis (osteospongiosis). A fenestra (small opening) is made in the horizontal semicircular canal. The homograft seals off the middle ear to provide sound protection for the round window. A partial stapedectomy removes only the fixed footplate (Fig. 41-6); a total stapedectomy removes the entire stapes, including the footplate. A stapedotomy (small opening into the footplate) may be the preferred procedure. The opening is made with a handheld perforator, microsurgical power drill, or laser. An argon, CO2, or KTP laser may be used for this purpose. A low-wattage lasing beam avoids thermal damage to the perilymph and inner ear structures. After partial or total stapedectomy or stapedotomy, the remaining superstructure is used to reconstruct the sound-conducting mechanism. The implant is an electronic device that converts sound waves into electrical signals to stimulate cochlear nerve fibers in the absence of functioning hair cells. Several devices are available. All of them have external and internal components (Fig. 41-7). The external part, which is attached behind the ear, has a microphone/transmitter and a speech processor/receiver. The internal part has a receiver/stimulator and electrode/channel that is threaded through the cochlea. The internal portion of the nose, the nasal cavity (Fig. 41-8) extends to the nasopharynx, the space behind the choanae (funnel-like posterior nasal orifices). The nose communicates with the ear via the eustachian tube. The hard and soft palates divide the nasal and oral cavities. The ethmoid bone separates the nasal and cranial cavities. • It provides filtered air to the respiratory system. Fine cilia in the mucous membranes propel mucus toward the nasopharynx. Air is warmed and moistened as it passes to the trachea and lower respiratory tract. • It contains the end organs for smell in the olfactory epithelium, which differs from other nasal epithelia. When nasal obstruction blocks off the olfactory epithelium, loss of smell (anosmia) results. The senses of smell and taste are closely related. 1. CT and rhinoscopy are often performed preoperatively to diagnose the nature and extent of pathologic conditions, especially in the paranasal sinuses. 2. Many nasal procedures are performed with the patient under local anesthesia with or without IV sedation. a. Topical 4% cocaine may be sprayed on the nasal mucosa or applied with soaked, compressed, absorbent patties (cottonoids) or sponges put in the nostrils. Cocaine produces vasoconstriction, as well as anesthesia. The used patties should be accounted for at the end of the procedure. b. A local agent, often lidocaine hydrochloride, 1% or 2%, is injected into the middle meatus. Epinephrine usually is used for vasoconstriction to control bleeding. c. When general anesthesia is indicated, a pack is placed in the pharynx to prevent aspiration of blood after the patient is intubated. 3. Paranasal sinuses and tissues underlying the mucosa are considered sterile. Therefore, instrumentation should be sterile, although the nasal cavity is considered a contaminated area because the instrumentation is entering a vascular bed. Venous drainage could easily carry microorganisms to the cavernous sinus, causing an intracranial infection. 4. CO2, Nd:YAG, and KTP lasers may be used. Endoscopes also are used. All equipment and accessories should be checked for working order. 5. Nasal packing is inserted at the end of most procedures except endoscopic sinus and laser procedures. A mustache dressing may be placed under the nose to act as a drip pad. Postoperatively the patient should be positioned in a head-up position to minimize bleeding. Ice is placed over the nasal bridge for the first 48 hours. The ice should be used in 20-minute intervals only. Most nosebleeds are caused by trauma, usually at Kiesselbach’s plexus of arteries and veins (also known as Little’s area) in the anterior part of the nasal septum (Fig. 41-9). Dehumidified air may cause changes in the mucosa and splitting of tiny vessels. Bleeding may be spontaneous, as in patients with arteriosclerosis, hypertension, or blood dyscrasia. Epistaxis is usually anterior and unilateral. In people with systemic disease, such as leukemia, or with severe fracture, the bleeding is frequently posterior and more severe. Management involves locating the precise bleeding site and promptly instituting appropriate therapy. Severe hemorrhage places the patient in a precarious condition. Hypovolemia should be corrected preoperatively.
Otorhinolaryngologic and head and neck surgery
General considerations in ear, nose, and throat procedures
Anesthesia considerations
Pharmacologic considerations
Positioning, prepping, and draping
Ear
Anatomy of the ear
Pathology of hearing
Differential diagnosis
Surgical procedures of the ear
General considerations
Middle ear procedures
Mastoidectomy.
Tympanoplasty.
Stapedectomy and stapedotomy.
Inner ear procedures
Implantation of a cochlear prosthesis.
Nose
Anatomy of the nose
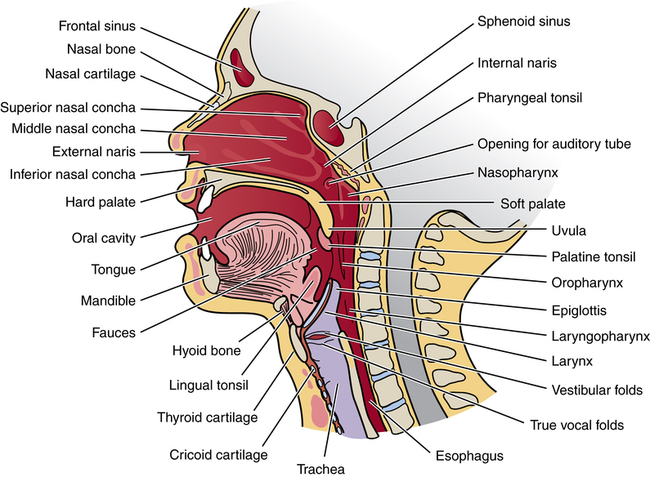
Physiology of the nose
Surgical procedures of the nose
General considerations
Nasal cavity procedures
Epistaxis.

 Website
Website