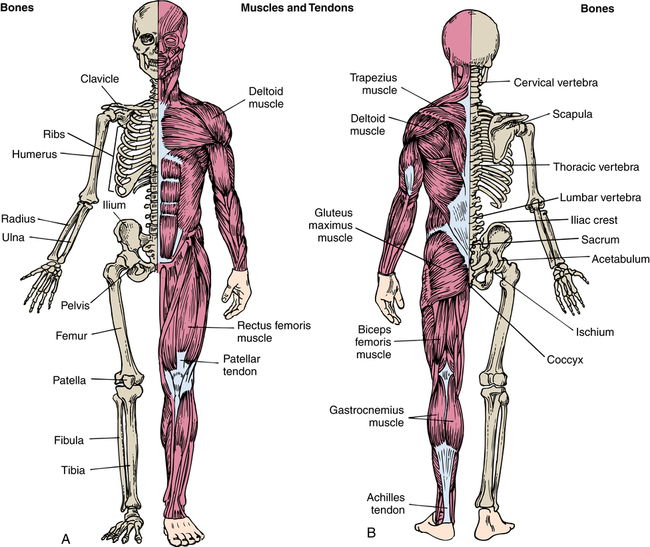
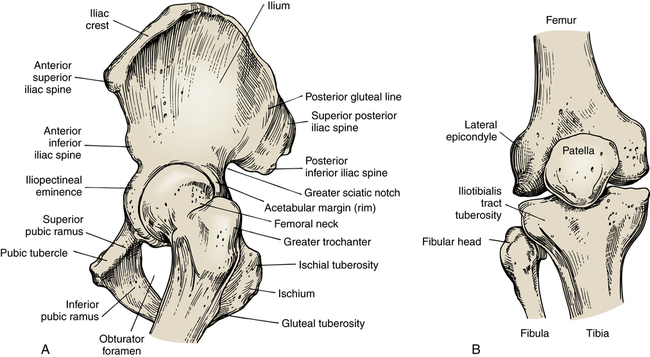
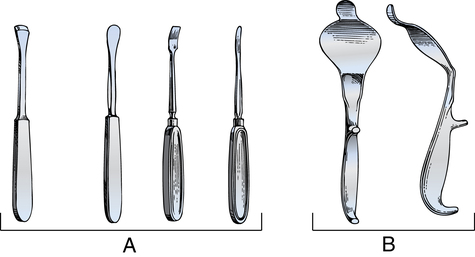
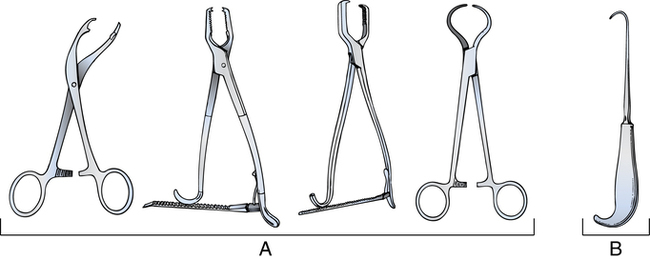
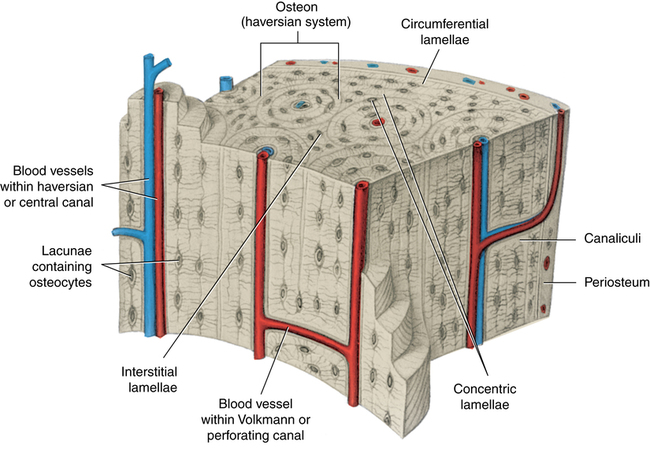
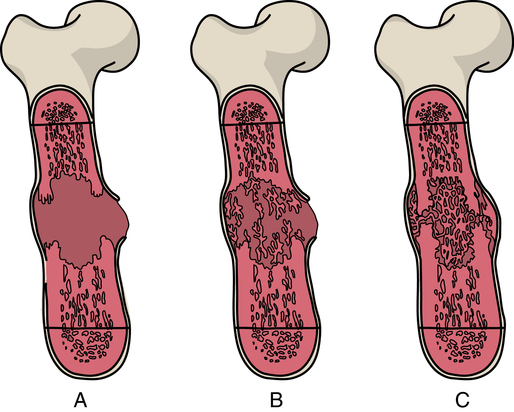
Chapter 36 After studying this chapter, the learner will be able to: • Identify the pertinent anatomy and physiology of the musculoskeletal system. • Discuss several types of fractures and the stabilization of each. • Describe several common specialty orthopedic instruments • Discuss the process for applying a cast. • Describe the care of a patient undergoing orthopedic surgery. Fusion of a joint. Disruption of the blood supply to a bone that causes death and irreversible decay of the osseous tissue. A cast cut into two parts—front and back for removal and reapplication. Bone cement implantation syndrome (BCIS) Adverse physiologic response of the patient to placement of bone cement in the medullary canal. Swelling between layers of fascia that causes damage to tissue. Toxins cause death of tissue. Used to encase and stabilize a structure. Casts are made of plaster or fiberglass. Closed reduction of a fracture without opening the skin. Generating heat. Evacuation of blood from a limb before inflating a tourniquet to create a bloodless field. Emergency procedure to release pressure on region of compartment syndrome. Specialized clean air delivery to the orthopedic operating room. The direction of air flow is carefully calculated to enter and exit the room without generating air-borne particulate. Open reduction and internal fixation of a fracture. Basophilic cells that synthesize collagen and glycoprotein to form bone matrix. Cells in the bone that influence growth and regeneration by breakdown and resorption of existing cellular material. Bone infection. The healing process of bone. Nonunion is the failure of the bone to align and heal. Eligibility includes current licensure in the United States or Canada and a minimum of 2 years’ experience as a registered nurse with a minimum of 1000 hours of nursing practice in orthopedic patient care in the preceding 3 years. The certification period is 5 years and can be renewed through 100 contact hours of continuing education or by successful passage of the certification examination. (More information about certification and the National Association of Orthopaedic Nurses [NAON] is available at http://www.orthonurse.org/.) The human skeleton (Fig. 36-1) has 206 separate bones. The bony framework of the human body is divided into the axial skeleton, which consists of 80 bones that make up the skull, vertebrae, and ribcage, and the appendicular skeleton, which consists of 126 bones that make up the limbs. Each upper extremity is composed of 32 bones, and each lower extremity is composed of 31 bones. Bones are classified according to shape as long, short, flat, and irregular. The humerus in the upper arm, radius and ulna in the forearm, femur in the thigh, and tibia and fibula in the lower leg are long bones. The end of a long bone is referred to as the epiphysis, and the shaft is referred to as the diaphysis. Thin plates of cartilage are found in the ends of long bones. In immature bone this is the area of growth and elongation. In mature bone these plates are ossified and do not grow (Fig. 36-2). The bones in the hand and foot are short bones. The scapula and patella are examples of flat bones. The vertebrae are irregular bones. The cortex (outer layer) of bone is compact, hard connective tissue. This cortical osseous tissue surrounds porous, spongy, cancellous tissue. The innermost substance is bone marrow and is classified as either red or yellow according to its location and function (see Fig. 36-2). Periosteum, a strong fibrous membrane, covers bone, except at joints. The blood supply and innervation penetrate periosteum and enter the bone through structures known as Volkmann canals. Lengthwise, lamellar structures, referred to as haversian canals, provide weight-bearing strength and passage for additional blood supply (Fig. 36-3). The inner aspect of bone is lined with endosteum, which is tissue similar to periosteum. In small children this layer contains osteoclasts that destroy bone to enlarge the marrow cavity for circumferential growth. Broken bones heal by a process referred to as union. Union of bones takes place in a series of steps (Fig. 36-4): 1. Hematoma formation. Blood accumulates in the area of break or injury. The inflammatory process ensues, and extravascular blood converts from liquid to a semisolid clot. Active phagocytosis removes necrotic tissue and debris. 2. Callus formation. Fibrin cells form a network around the injured area. The damaged periosteum is stimulated to generate osteoblasts, forming new bony substance referred to as osteoid. Minerals begin to accumulate in the network, forming a collagen callus. A callus is visible on radiograph within 1 to 2 weeks of injury. 3. Calcification process. Calcification begins and establishes support of the injury. Connective tissue proliferates across the site and is usually completely calcified within 6 weeks. 4. Remodeling phase. Excess cellular material is resorbed, and the bone resumes its preinjury strength and configuration. This remodeling phase is enhanced by stress and exercise. Depending on the site and severity of the injury, complete remodeling can take 6 months to 1 year to complete. Joints are classified by variations in structure that permit movement (Fig. 36-5). The hip and shoulder are ball-and-socket joints; the knee, ankle, elbow, and phalangeal joints of the fingers are hinged; the wrist is a condyloid joint; and the thumb is a saddle joint. The proximal and distal bone ends are held securely in place by the joint capsule attached to both bone shafts and by ligaments. In addition to conventional x-rays, computed tomography (CT), magnetic resonance imaging (MRI), and bone densitometers allow evaluation of conditions amenable to surgical correction. Arthroscopy enhances diagnosis and treatment of joint disorders, especially those caused by sports injuries.8 Highly sophisticated implants and instrumentation make many orthopedic procedures possible. A large percentage of orthopedic surgical procedures involve contaminated traumatic wounds or tissues highly susceptible to infection. a. Wear knee-high, waterproof shoe covers or boots. Blood and body fluids frequently splash to the floor and lower legs. Shoe covers should be removed and changed if they become contaminated. b. Wear a fluid-impervious gown and/or a waterproof apron under the gown. Copious irrigation frequently is used. c. Double-glove at all times, and/or have additional protection for fingers. Cloth gloves or glove liners of woven Kevlar may be worn between latex gloves in cases of trauma and major reconstructive procedures when sharp instruments and mechanical devices are used. d. Wear protective eyewear at all times. A full-face shield should be considered when splatter is anticipated. Powered bone instruments can produce a fine mist. A space suit–type helmet should be considered when powered bone instruments are used. See Figure 16-5 for orthopedic helmeted attire. 2. Avoiding inadvertent penetration of the skin of personnel during the surgical procedure. a. Use instrument ties and other nontouch suturing and sharp instrument techniques whenever possible. b. Pass sharp instruments on a tray or magnetic mat, not hand to hand. c. Announce when instruments are being passed. d. Cover exposed internal wires and pins that extend through the skin with appropriate tubing, cork stoppers, or plastic caps. 3. Clean gowning and gloving (i.e., the scrub person should change contaminated gloves before gowning and gloving another team member during the surgical procedure). To expose a bone or joint, special retractors and elevators are used (Fig. 36-6). Retractors are contoured to fit around the bone or joint without cutting or tearing muscles. Periosteal elevators are semi-sharp instruments used to strip periosteum from bone without destroying its ability to regenerate new bone. They are used for blunt dissection. Grasping instruments are required to hold, manipulate, or retract bone. Bone-holding forceps should be selected appropriately for the size of the bone in the surgical field. Bone hooks are used for retraction and leverage (Fig. 36-7). Heavy clamps are needed to hold smaller bones or grasp a joint capsule, such as a meniscus clamp for fibrocartilage in the knee. Cutting instruments are used to remove soft tissue around bone; to cut into, cut apart, or cut out portions of bone; and to smooth jagged edges of bone. The surgeon’s armamentarium includes osteotomes, gouges, chisels, curettes, rongeurs, reamers, bone-cutting forceps, meniscotomes, rasps, files, drills, and saws (Fig. 36-8). These have sharp edges. Extra care should be taken not to nick or damage cutting edges; they should always be protected on the instrument table and during cleaning, sterilizing, and storing. Fitted sterilizable cases (Fig. 36-8, E), trays, foam towels, or canvas cases are used to keep sets together by sizes (e.g., osteotomes, gouges, chisels, curettes), as well as to protect cutting edges. Cutting instruments must be sharp. Osteotomes, chisels, gouges, and meniscotomes can be sharpened by operating room (OR) personnel with handheld hones or a honing machine designed for this purpose. Most manufacturers provide a service for sharpening and repairing instruments. Curettes, rongeurs, and reamers should be returned for sharpening. Small drill bits and saw blades usually are disposable (Fig. 36-9). The items discussed in this section are used frequently in many orthopedic procedures. When necessary to provide structural support, a piece of bone from one part of the skeletal system may be obtained from the patient to reinforce another part of the skeletal system. Autologous cancellous and cortical bone is obtained from the crest of the ilium, and cortical bone is obtained from the fibula.10 Bone wax is used for hemostasis on cut bone. The surgeon’s preference card should be checked before the packet is opened to the sterile field. The inner sterile foil packet can be placed in warm saline irrigation to soften the wax for use. Alternative bone edge hemostasis can be attained with Gelfoam slurry or synthetic non–bee’s wax copolymers. Bone wax and other bone edge hemostatics are discussed in Chapter 29. Special care must be used to carry out strict asepsis. Infection is the most serious, dreaded, and costly complication of orthopedic surgery. Some surgeons prefer to operate within an ultraclean air system, especially for total joint replacement procedures. Orthopedic surgeons use laminar airflow more frequently than do other surgical specialists.2,13 A surgical isolation bubble system or patient isolation drape may be used to isolate the sterile field from personnel and equipment. Surgical helmets are available that isolate airborne contaminants shed from each team member. Hoses exhaust exhaled air. Masks are not worn under the helmet. Figure 16-5 depicts the team wearing the helmet system. This system can be used independently or in conjunction with a laminar airflow system. Laminar air flow design is described and illustrated in detail in Chapter 10. 1. Consult the surgeon’s preference card, and manufacturer’s manual for attachments needed for each desired position. The fracture table is used for supine procedures and cannot accommodate lateral positioning. 2. Check the patient’s height and weight in kilograms. Each style of OR bed has specific weight limits. The weight limit is printed on the base of the table. 3. Assemble the necessary attachments. Pad all parts of the OR bed and attachments to prevent pressure on joints, the sacrum, and the perineum. 4. Attach the standard components and accessories to the OR bed frame so that all is in readiness for positioning the patient after the administration of anesthesia. 5. Arrange appropriate staff to move the patient from one surface to another. The patient will be a full lift whether general or regional anesthesia is used. Placement on the fracture table is somewhat precarious because the body section is very narrow. It is easy for the patient to fall if not carefully positioned and secured. Conventional x-ray equipment and fluoroscopy frequently are used during orthopedic procedures. Considerations for patient safety and personnel protection described in Chapter 13 apply to the use of x-ray for all invasive or noninvasive orthopedic procedures performed in the OR suite. Special positioning and draping techniques may be necessary, especially when C-arm fluoroscopy is used. Often both anteroposterior (AP) and lateral views are necessary to assess the alignment of a bone or determine the position of a fixation device or prosthetic implant.12 X-rays or C-arm fluoroscopic images document the work of the surgeon for the permanent record. 1. Unit beds are used to transport patients in traction apparatus. Beds, frames, and transport carts can be decontaminated in the vestibule/exchange area. 2. A cast should be removed preoperatively in the cast room. If the OR suite does not have a cast room, a cast may be bi-valved in the patient’s room and then removed in the OR to minimize the dispersal of particulates in the air. 3. Positioning the patient intraoperatively and postoperatively should be directed by the surgeon. Immobilization and good body alignment contribute to patient comfort and prevention of neurovascular injury. Pillows or other supports should not cause pain, impair function of unaffected muscles and joints, or compromise circulation. 4. Transcutaneous electrical nerve stimulation (TENS) may be used for postoperative analgesia. The electrode pads are affixed to the skin along the sides of the incision when a dressing is applied. Before application, the skin should be cleansed with water. (Saline is a conductor, so it cannot be used for cleansing.) The wires are connected to the stimulator in the postanesthesia care unit (PACU) or after recovery from anesthesia. The patient can be taught preoperatively how to use TENS for relief of pain postoperatively. 5. Electrostimulation promotes cellular responses in bone and ligaments. Mechanically stressed bone generates electrical potentials related to patterns of bone regeneration. If stimulated, healing may accelerate. 1. A sterile irrigating pan is placed under an extremity to catch solution if an open wound is to be cleansed, irrigated, and debrided, as for a compound fracture. If an irrigating pan is not used, the runoff is collected by an absorbent pad under the prepped limb. A staff aide wearing gloves can elevate the limb during the prep procedure. 2. A pneumatic tourniquet is commonly used for a surgical procedure on or below the elbow or knee to provide a blood-free field. The tourniquet cuff is applied before the extremity is prepped. Prevent prep solution from running under the tourniquet cuff by covering the cuffed area with a sticky drape or towel. The tourniquet is not inflated until the limb is elevated and exsanguinated with a sterile Esmarch. It is important to exsanguinate the limb to assure a bloodless field and prevent blood clots. Do not discard the Esmarch in case it is needed again. Re-roll it and place on back table. Always check the pressure setting with the surgeon before inflating a tourniquet. Ischemia time is a critical factor in patient safety. Notify the surgeon of the time lapse after the first hour and every 15 minutes thereafter throughout tourniquet inflation. Document the tourniquet location, time, pressure, and unit identifying number. 3. The extremity is elevated for the skin prep. A dry sterile drape is positioned under the limb by the scrub person before it is lowered to the sterile field. 4. A self-adhering incise drape may be used as the first drape applied over the incision site. If the extremity must be manipulated during the surgical procedure, the entire circumference must be draped free with sterile stockinette. 5. Stockinette may be used over a self-adhering plastic drape or to cover skin and wrapped with Coban or ACE bandage to keep the circumferential drape in place. This wrap is cut with bandage scissors over the line of the incision. An extremity sheet or split sheet may be used over the wrapped stockinette as a body drape. A large sterile glove can be placed over the foot to protect the sterile field during lower limb surgery. 6. A fluid-control drape collects blood and irrigating fluids in a pouch to prevent strike-through of and runoff from drapes. Fluids can be drained or suctioned for disposal. Blood may be suctioned directly from the surgical site for autotransfusion if blood loss is more than 400 mL, as in some hip procedures. 7. After a surgical procedure on a knee joint, a pressure dressing is usually applied to prevent serum accumulation. This may be a Robert Jones dressing, which includes a soft cotton batting roll, sheet wadding, and cotton elastic bandage. A cotton roll or other bulky material may be placed on each side of the knee and held in place with sheet wadding. A four-ply, crinkled-gauze bandage or cotton elastic bandage over this provides even, gentle pressure. Depending on the surgical procedure, a plaster splint or some other type of knee immobilizer may be preferred. 8. After a surgical procedure on a shoulder, the arm may be bound against the side of the chest for immobilization. An absorbent pad or a large piece of cotton or sheet wadding is placed under the arm to keep skin surfaces from touching, because they may macerate. The arm is held in a shoulder immobilizer that supports the humerus and wrist, or it may be bound firmly to the side of the chest with a cotton elastic bandage. 9. Postoperatively, the extremity is elevated on a pillow placed lengthwise. This facilitates venous return, decreases swelling, and minimizes pressure on nerves. The hand should be elevated above the level of the heart; the toes must be higher than the nose.
Orthopedic surgery
The art and science of orthopedic surgery
Anatomy and physiology of the musculoskeletal system
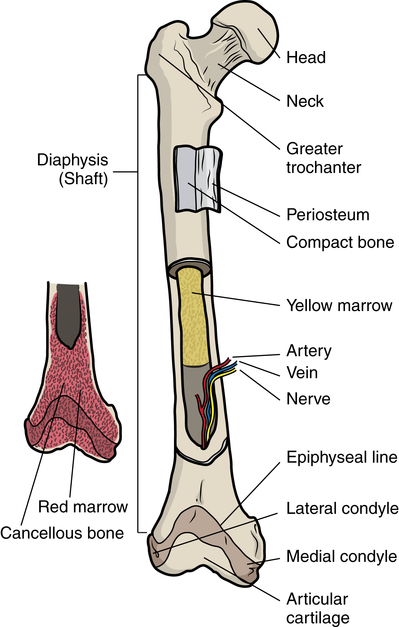
Bones
Bone healing
Joints
Special features of orthopedic surgery
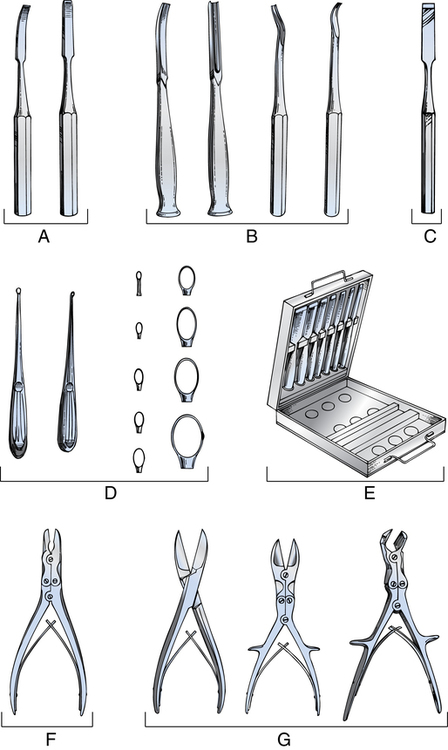
Instrumentation
Exposing instruments
Grasping instruments
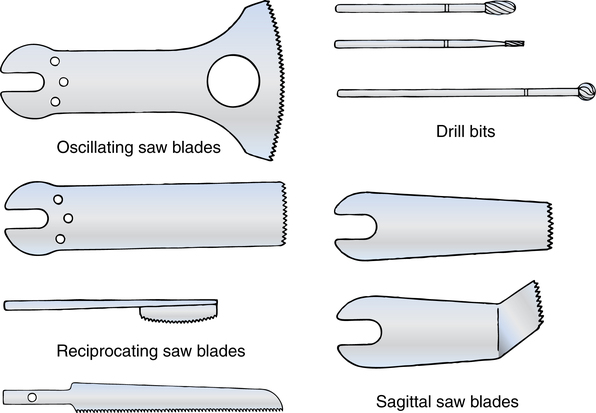
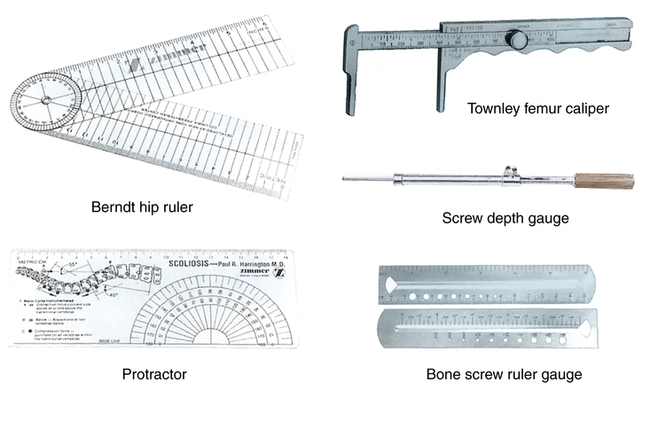
Dissecting and debulking instruments
Materials and equipment used frequently
Bone grafts
Bone wax
Laminar air system
Fracture table
X-ray equipment
Special considerations in orthopedic surgery
Extremity procedures
General considerations
Orthopedic surgery

 Website
Website