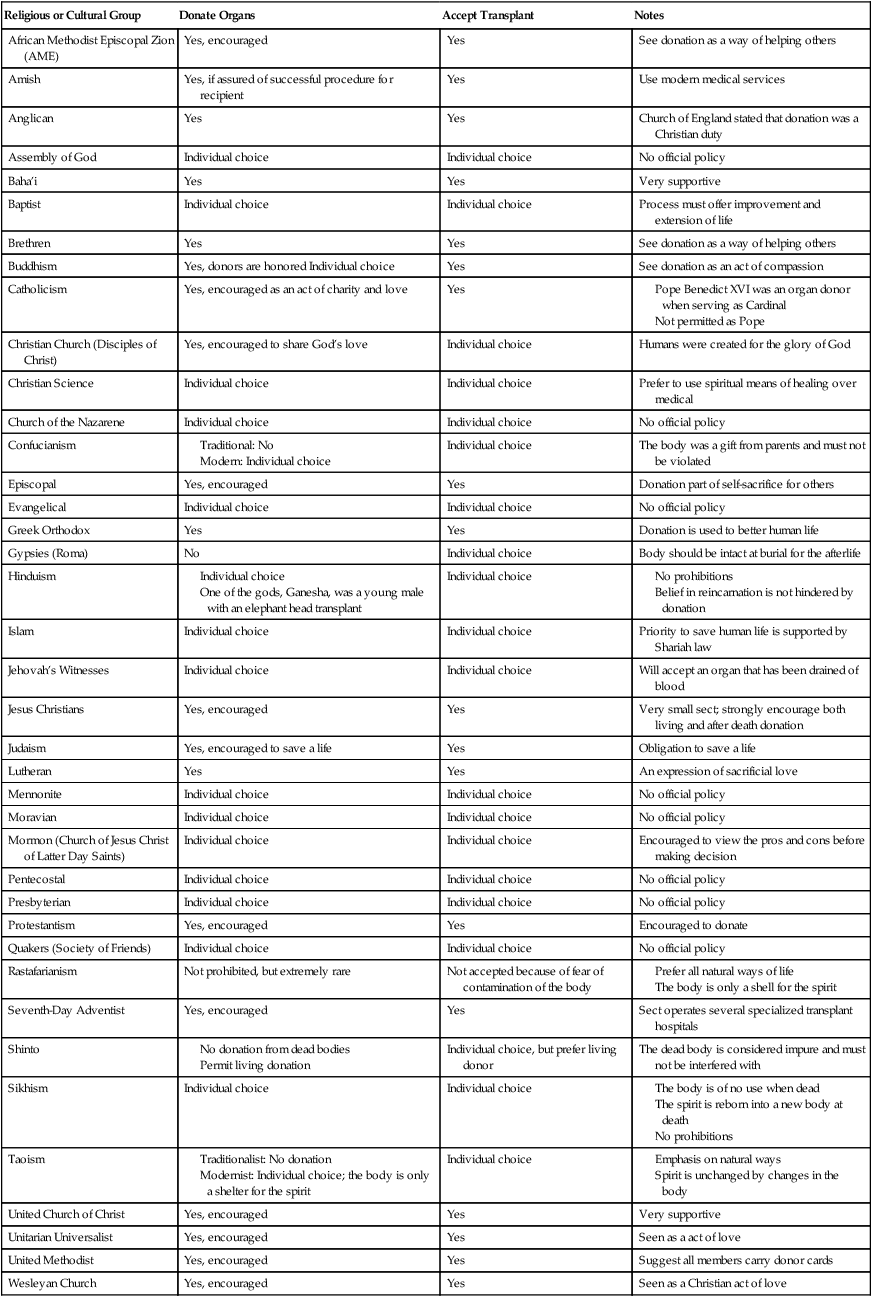
Chapter 45 After studying this chapter, the learner will be able to: • List the criteria for validating brain death. • Describe the testing performed on tissue before it is suitable for transplantation. • Discuss the role of the host procurement facility. • Discuss the psychologic effect of a transplant on the donor and recipient families. Transplantation is the transfer of an organ or tissue from one person to another or from one body part to another. Concentrated efforts continue in search of compensation for or suitable replacements for deficient tissues and organs. The indication for organ transplantation is irreversible functional failure of the organ. The goals of transplantation include changing appearance, restoring function, or improving quality of life. (More information is available at www.unos.org and www.organdonor.gov.) Certain tissues and whole organs can be transplanted and grafted to restore bodily function. The type of transplant selected depends on the purpose of the graft, anatomic function, and availability of the tissue or organ. The types of biologic transplants are listed in Box 45-1. • Skin grafts provide a protective surface covering, initially acquiring and then eventually losing vascular connection with the host. • Corneal grafts replace nonfunctioning corneal tissue. • Bone grafts afford temporary structural supports and a pattern for regrowth of the host’s bone; the grafts are then resorbed. • Ossicles and the tympanic membrane in the ear can be transplanted to restore bone-conduction hearing loss. • Cartilage restores contour in a defect of cartilaginous facial structures. • Blood vessel grafts bypass or replace diseased or obstructed segments of vessels. • Bone marrow restores hematologic and immunologic functions. Tissue transplants can be either autografts or allografts. Xenograft (from another species) transplants are in the research phases. The American Association of Tissue Banks sets standards for retrieving, processing, storing, and labeling tissues and for donor criteria for allografts (Box 45-2). Tissue for transplantation is procured from suitable cadaver (nonliving or brain dead) donors, either heartbeating or nonheartbeating, or from a living donor. Table 45-1 details the procurement parameters for tissue allografts. (Additional information is available from the National Institute of Transplantation at www.transplantation.com or the United Network for Organ Sharing at www.unos.org.) TABLE 45-1 Tissue/Allograft Procurement Parameters Potential donors are screened to avoid the transmission of infection or disease. Cultures are taken at the time of procurement for microbiologic and serologic testing.8 Tissue is not transplanted until negative test results are obtained; tissue is discarded if the test result is positive. Living bone donors are tested for HIV immediately after donation and again after 90 days because seroconversion can be delayed. Recipients also should be tested and should be negative for HIV and hepatitis B virus (HBV). A baseline is essential to establish that the patient was not infected by the act of grafting. Patients with HIV or HBV are not barred from receiving an allograft, but baseline data can help rule out causes for rejection or infection. Incidences of graft failure and superinfection are high in patients who are immunocompromised with HIV. Bone marrow transplantation is essentially a tissue transplant. However, because this type of transplantation is fraught with the hazards of rejection, bone marrow is procured and transplanted with a protocol similar to that of solid organ procurement and transplantation. Bone marrow is transplanted only after conventional treatments have failed to replenish depleted bone marrow cells. The marrow given via infusion restores hematologic and immunologic functions. Indications for treatment are acute myelodysplastic syndrome, lymphoblastic leukemia, myelogenous leukemia, aplastic anemia, and certain other blood diseases.3,4 1. Autologous: The donor is the recipient. Stem cells are collected from the patient with leukemia that is in remission, cryopreserved, and stored to be infused during a subsequent relapse. 2. Allogeneic: The donor is HLA-compatible with the recipient. Marrow is harvested for immediate infusion into the recipient. a. A syngeneic donor, an identical twin, is preferred. b. A genotypically compatible sibling or parent has identical tissue type. c. An unrelated allogeneic donor must be HLA-compatible. Graft-versus-host disease (GVHD) is unique to allogeneic bone marrow transplantation. With GVHD, donor T cells immunologically attach to recipient cells and cause tissue damage at the site of antigen localization. 3. T cell–depleted marrow: For prevention of GVHD, mature T lymphocytes are removed from donor marrow before infusion into the recipient. After pretransplant protocols have been completed, the donor is hospitalized before the scheduled transplantation. In the OR, with the patient under general or spinal anesthesia, 500 to 700 mL of bone marrow is aspirated at multiple sites from the iliac crests; the sternum may also be used. The marrow is filtered, heparinized, and placed in sterile containers for infusion. The donor is watched for bleeding and may need blood and fluid replacement.4 If the marrow is not from an identical twin, blood is irradiated before transfusion to destroy the lymphocytes. Mature blood cells and platelets are unaffected by the irradiation process. Daily marrow aspirations and complete blood counts are performed on the host. The success or failure of transplantation is usually decided after 10 to 20 days, when the new marrow begins to function.4 Organ transplantation can be a lifesaving treatment for some end-stage diseases. Although tissue grafts are commonplace, transplantation of functional, whole, vital organs presents physiologic, philosophic, and ethical dilemmas. A biologically related donor (referred to as a living related donor) makes a supreme sacrifice to become an organ donor; therefore, cadavers are the primary source of organs for transplant.7 Organ donation is the ultimate gift of life and is given by the donor to the recipient. Transplantation can restore the recipient to near-normal physiologic status. Ethical concerns cross religious and cultural boundaries.6,9 Table 45-2 gives examples of religious and cultural groups and their positions about organ donation and transplantation.6,9 Some traditionalist beliefs do not support donation because the body of the dead should not be altered in any way. Modernist beliefs have transcended many old ways by pointing out that the body is not needed for passage into the afterlife.6,9 Information about religious and cultural views about donation can be found at www.organdonor.gov and www.lifebanc.org. TABLE 45-2 Organ Donation and Transplantation Beliefs According to Religious or Cultural Groups Kidney transplantation was initially the most successful and principal clinical application of organ transplantation. If a kidney graft fails, the patient may survive by returning to hemodialysis indefinitely before receiving another transplant.5 This option does not exist for transplants of the heart, liver, pancreas, or lungs. No practical prolonged artificial support exists for these organs in the event of an allograft failure. Transplantation of each organ involves unique technical and physiologic problems, but the major barriers and causes of transplant failure are immunologic rejection and infection.8 Immunodeficiency depends on the amount of immunosuppression the patient receives to prevent rejection. Immunosuppressive agents leave the patient prone to opportunistic infection. Reverse protective isolation may be advisable if the patient has development of leukopenia, a decrease in white blood cells. In other aspects of care, transplant recipients are similar to other critical surgical patients with severe chronic illnesses who need measures that minimize the risk of infection. The American Society of Transplant Surgeons (www .asts.org) and the International Society of Transplantation meet regularly to exchange ideas and information among people of different scientific backgrounds. The aim is to achieve the best possible patient survival rather than merely transplant survival. A national task force has also been established to analyze medical, legal, ethical, economic, and social issues of concern in organ procurement and transplantation.2 Other countries have similar mechanisms. For example, the United Kingdom Transplant Register has membership in the Euro Transplant Register. Organs procured within the United Kingdom can be transported by air to another country in Europe, and vice versa, for a histocompatible recipient. The number of patients awaiting transplants exceeds the supply of available donor organs. As a result, many patients die while waiting for a suitable organ to become available.7 Many people carry a signed Uniform Donor Card or other identification (e.g., the reverse side of a driver’s license) that states that certain or all organs and tissues may be removed for transplantation in the event of death. Such cards, or a living will, constitute legal written consent under the Uniform Anatomical Gift Act enacted by all 50 states. Written or telephone consent is still obtained from the family of a potential donor before procurement may commence.7 Immunologic rejection and the shortage of donor organs remain the principal deterrents to transplantation. The goal is selection of a donor-recipient match with adequate histocompatibility to permit an organ to function without complications. Organs and tissues come from two primary sources: cadaver (heartbeating and nonheartbeating) and living related donors (Table 45-3). TABLE 45-3 Nonheartbeating cadaver donor: heart valves only Donor criteria include no cardiac disease and normal cardiac enzymes
Organ procurement and transplantation
Types of transplants
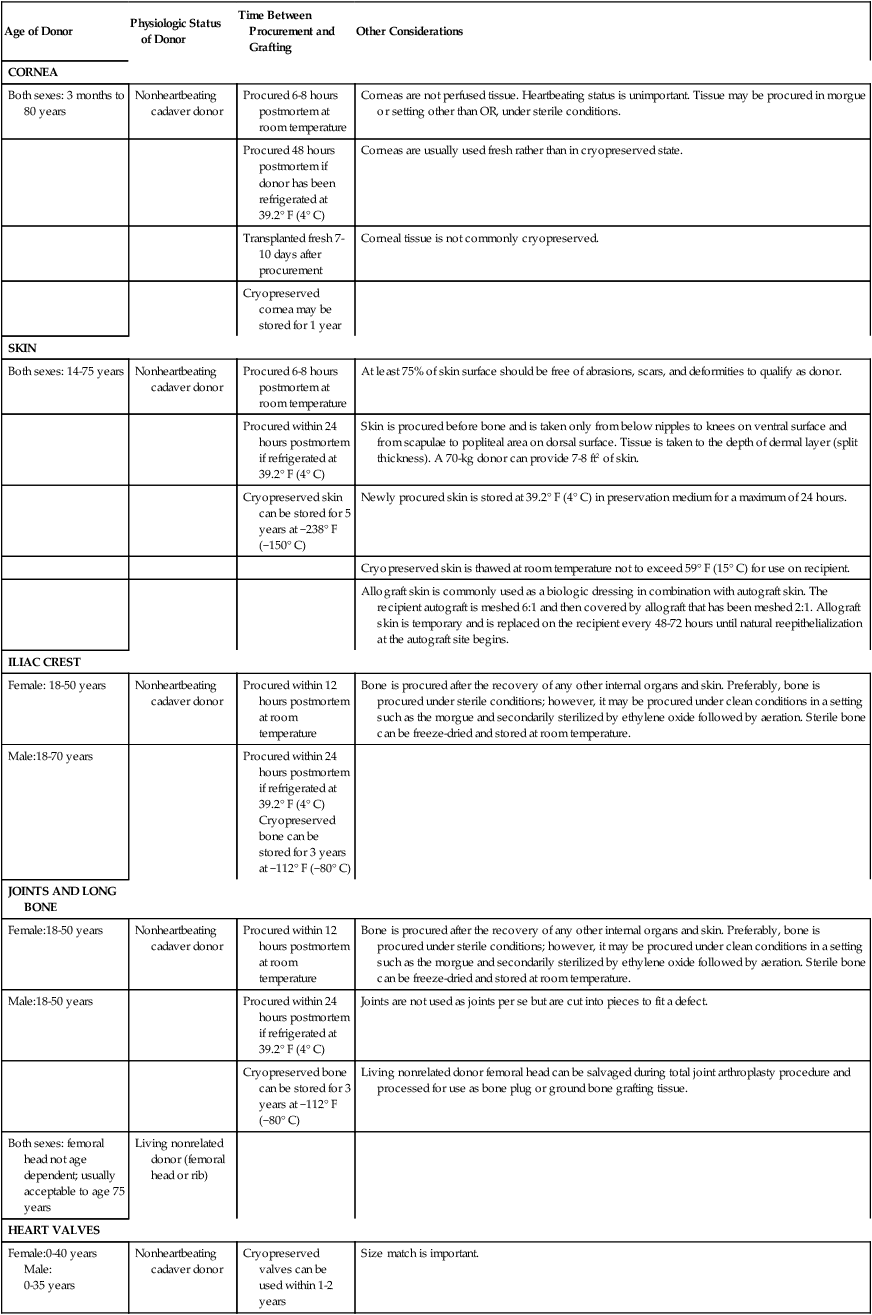
Tissue transplantation
Age of Donor
Physiologic Status of Donor
Time Between Procurement and Grafting
Other Considerations
CORNEA
Both sexes: 3 months to 80 years
Nonheartbeating cadaver donor
Procured 6-8 hours postmortem at room temperature
Corneas are not perfused tissue. Heartbeating status is unimportant. Tissue may be procured in morgue or setting other than OR, under sterile conditions.
Procured 48 hours postmortem if donor has been refrigerated at 39.2° F (4° C)
Corneas are usually used fresh rather than in cryopreserved state.
Transplanted fresh 7-10 days after procurement
Corneal tissue is not commonly cryopreserved.
Cryopreserved cornea may be stored for 1 year
SKIN
Both sexes: 14-75 years
Nonheartbeating cadaver donor
Procured 6-8 hours postmortem at room temperature
At least 75% of skin surface should be free of abrasions, scars, and deformities to qualify as donor.
Procured within 24 hours postmortem if refrigerated at 39.2° F (4° C)
Skin is procured before bone and is taken only from below nipples to knees on ventral surface and from scapulae to popliteal area on dorsal surface. Tissue is taken to the depth of dermal layer (split thickness). A 70-kg donor can provide 7-8 ft2 of skin.
Cryopreserved skin can be stored for 5 years at −238° F (−150° C)
Newly procured skin is stored at 39.2° F (4° C) in preservation medium for a maximum of 24 hours.
Cryopreserved skin is thawed at room temperature not to exceed 59° F (15° C) for use on recipient.
Allograft skin is commonly used as a biologic dressing in combination with autograft skin. The recipient autograft is meshed 6:1 and then covered by allograft that has been meshed 2:1. Allograft skin is temporary and is replaced on the recipient every 48-72 hours until natural reepithelialization at the autograft site begins.
ILIAC CREST
Female: 18-50 years
Nonheartbeating cadaver donor
Procured within 12 hours postmortem at room temperature
Bone is procured after the recovery of any other internal organs and skin. Preferably, bone is procured under sterile conditions; however, it may be procured under clean conditions in a setting such as the morgue and secondarily sterilized by ethylene oxide followed by aeration. Sterile bone can be freeze-dried and stored at room temperature.
Male:18-70 years
Procured within 24 hours postmortem if refrigerated at 39.2° F (4° C)
Cryopreserved bone can be stored for 3 years at −112° F (−80° C)
JOINTS AND LONG BONE
Female:18-50 years
Nonheartbeating cadaver donor
Procured within 12 hours postmortem at room temperature
Bone is procured after the recovery of any other internal organs and skin. Preferably, bone is procured under sterile conditions; however, it may be procured under clean conditions in a setting such as the morgue and secondarily sterilized by ethylene oxide followed by aeration. Sterile bone can be freeze-dried and stored at room temperature.
Male:18-50 years
Procured within 24 hours postmortem if refrigerated at 39.2° F (4° C)
Joints are not used as joints per se but are cut into pieces to fit a defect.
Cryopreserved bone can be stored for 3 years at −112° F (−80° C)
Living nonrelated donor femoral head can be salvaged during total joint arthroplasty procedure and processed for use as bone plug or ground bone grafting tissue.
Both sexes: femoral head not age dependent; usually acceptable to age 75 years
Living nonrelated donor (femoral head or rib)
HEART VALVES
Female:0-40 years
Male:
0-35 years
Nonheartbeating cadaver donor
Cryopreserved valves can be used within 1-2 years
Size match is important.
Bone marrow transplantation
Organ transplantation
Religious or Cultural Group
Donate Organs
Accept Transplant
Notes
African Methodist Episcopal Zion (AME)
Yes, encouraged
Yes
See donation as a way of helping others
Amish
Yes, if assured of successful procedure for recipient
Yes
Use modern medical services
Anglican
Yes
Yes
Church of England stated that donation was a Christian duty
Assembly of God
Individual choice
Individual choice
No official policy
Baha’i
Yes
Yes
Very supportive
Baptist
Individual choice
Individual choice
Process must offer improvement and extension of life
Brethren
Yes
Yes
See donation as a way of helping others
Buddhism
Yes, donors are honored Individual choice
Yes
See donation as an act of compassion
Catholicism
Yes, encouraged as an act of charity and love
Yes
Christian Church (Disciples of Christ)
Yes, encouraged to share God’s love
Individual choice
Humans were created for the glory of God
Christian Science
Individual choice
Individual choice
Prefer to use spiritual means of healing over medical
Church of the Nazarene
Individual choice
Individual choice
No official policy
Confucianism
Individual choice
The body was a gift from parents and must not be violated
Episcopal
Yes, encouraged
Yes
Donation part of self-sacrifice for others
Evangelical
Individual choice
Individual choice
No official policy
Greek Orthodox
Yes
Yes
Donation is used to better human life
Gypsies (Roma)
No
Individual choice
Body should be intact at burial for the afterlife
Hinduism
Individual choice
Islam
Individual choice
Individual choice
Priority to save human life is supported by Shariah law
Jehovah’s Witnesses
Individual choice
Individual choice
Will accept an organ that has been drained of blood
Jesus Christians
Yes, encouraged
Yes
Very small sect; strongly encourage both living and after death donation
Judaism
Yes, encouraged to save a life
Yes
Obligation to save a life
Lutheran
Yes
Yes
An expression of sacrificial love
Mennonite
Individual choice
Individual choice
No official policy
Moravian
Individual choice
Individual choice
No official policy
Mormon (Church of Jesus Christ of Latter Day Saints)
Individual choice
Individual choice
Encouraged to view the pros and cons before making decision
Pentecostal
Individual choice
Individual choice
No official policy
Presbyterian
Individual choice
Individual choice
No official policy
Protestantism
Yes, encouraged
Yes
Encouraged to donate
Quakers (Society of Friends)
Individual choice
Individual choice
No official policy
Rastafarianism
Not prohibited, but extremely rare
Not accepted because of fear of contamination of the body
Seventh-Day Adventist
Yes, encouraged
Yes
Sect operates several specialized transplant hospitals
Shinto
Individual choice, but prefer living donor
The dead body is considered impure and must not be interfered with
Sikhism
Individual choice
Individual choice
Taoism
Individual choice
United Church of Christ
Yes, encouraged
Yes
Very supportive
Unitarian Universalist
Yes, encouraged
Yes
Seen as a act of love
United Methodist
Yes, encouraged
Yes
Suggest all members carry donor cards
Wesleyan Church
Yes, encouraged
Yes
Seen as a Christian act of love
Organ procurement
Age of Donor
Physiologic Status of Donor
Time Between Procurement and Transplantation
Other Considerations
HEART
Female: 0-40 years
Heartbeating cadaver donor
3-6 hours, fresh tissue
Heartbeating cadaver donor: total heart and segments of great vessels
Male: 0-35 years
Nonheartbeating cadaver donor
Cryopreserved valves can be used within 1-2 years
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

 Website
Website