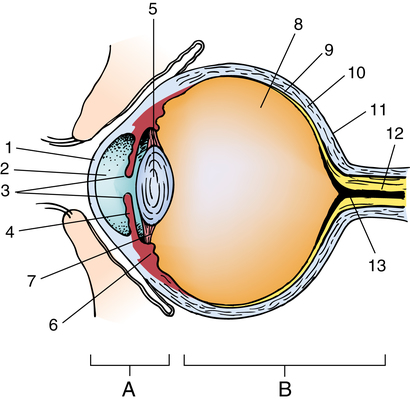
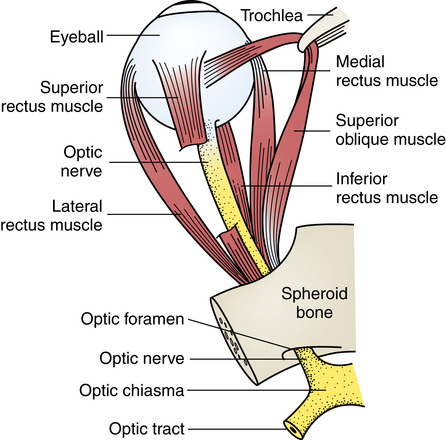
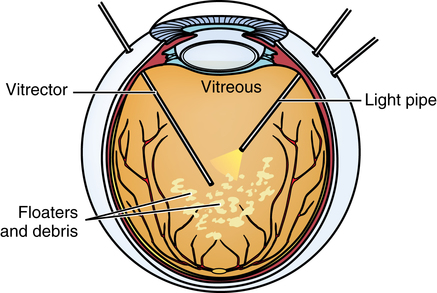
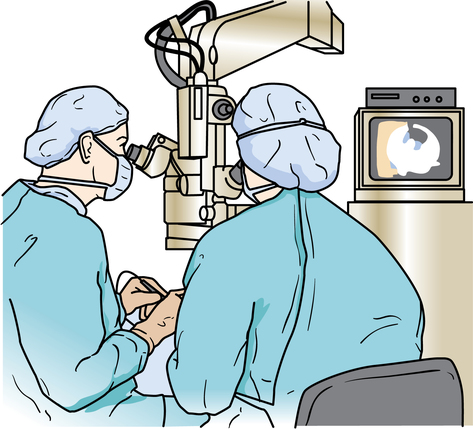
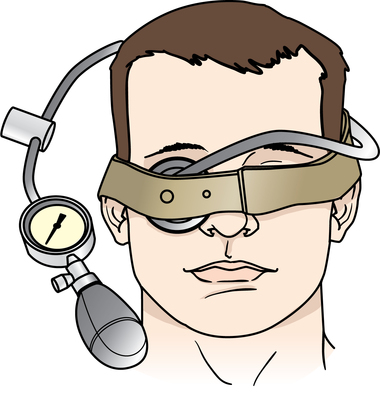
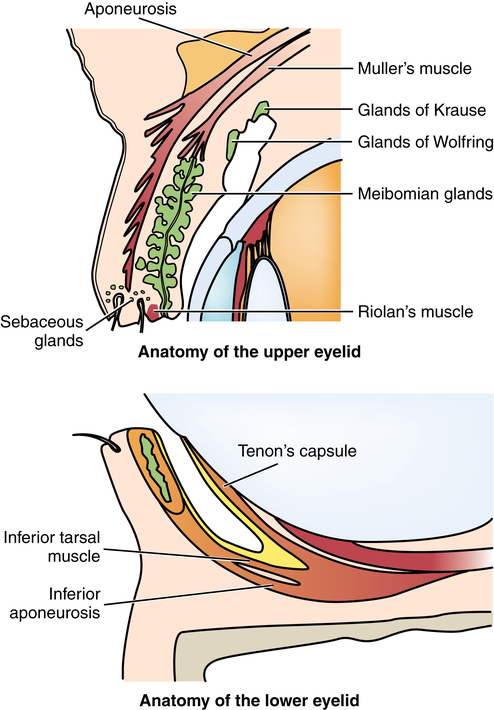
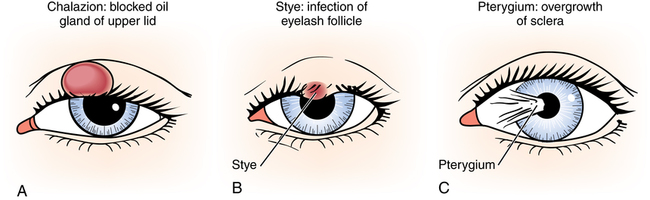
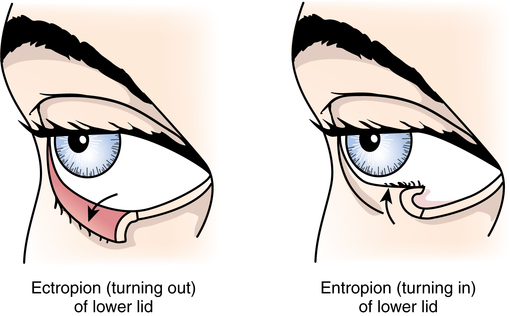
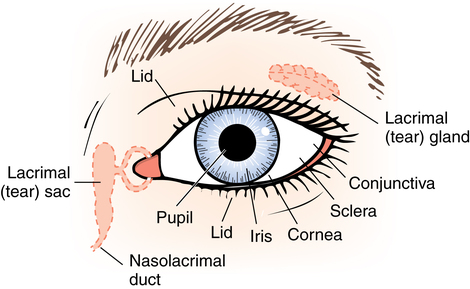
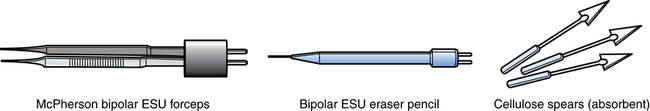
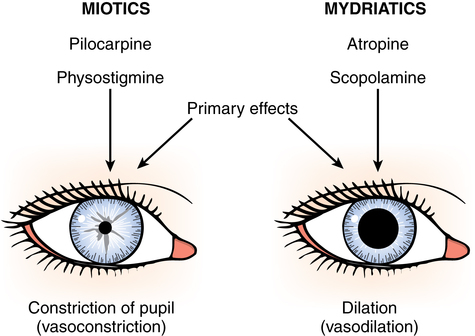
Chapter 39 After studying this chapter, the learner will be able to: • Identify the pertinent anatomy of the eye and surrounding structures. • Describe the procedures performed on the eye for glaucoma. • Discuss the advantages and disadvantages of intraocular lens implantation. A thorough understanding of the anatomic structure and physiology of the eye is fundamental to a comprehension of the surgical procedures. The globe, or eyeball, is situated within the bony orbit and is surrounded by a padding of fatty tissue. Its position is maintained by extraocular muscles and fascial attachments. The sclera, the white outer tissue layer of the globe, is contiguous with the transparent avascular cornea anteriorly. The conjunctiva is the mucous membrane that lines the inner side of the upper and lower eyelids and the exposed portion of the sclera, except for the cornea (Fig. 39-1). The eyeball is divided into two segments: anterior and posterior. The anterior segment of the eye includes the cornea, the anterior chamber filled with aqueous fluid (humor), the circular pigmented iris, and the lens. The lens consists of a clear, transparent, gelatinous protein encased in a capsule. It is supported by a series of suspensory ligaments called zonules. The posterior segment, the portion of the eye behind the lens, contains the vitreous fluid (which must be clear for vision), the retina, and the choroid linings, which are the vascular nourishing layers (Fig. 39-2). Innervation of vision and sensory transmission is derived from the second cranial nerve (optic nerve) (Fig. 39-3). Motor innervation extends from the third cranial nerve (oculomotor nerve) to the rectus muscles. The superior oblique muscles are innervated by the fourth cranial nerve (trochlear nerve). The lateral rectus muscle is innervated by the sixth cranial nerve (abducens nerve). The physiology of vision requires the following: 1. Urinary urgency can be a problem in geriatric patients or in patients receiving diuretic medication. Although the patient should void before coming to the OR, offer the patient the use of a bedpan or urinal before he or she transfers to the operating bed. Severe urinary urgency can cause increased intraocular pressure (IOP) during the procedure. Strain and gross movement are dangerous and are to be avoided. 2. The surgeon and circulating nurse verify the intended surgical site with the patient and with the office records. After confirmation and to avoid error, some surgeons place an indelible mark on the side of the patient’s neck that corresponds to the affected eye. 3. The patient is placed in the supine position on the operating bed so the head and body are aligned. Most ORs use a dedicated ophthalmic operating bed that can be used during the procedure and to transport the patient to the postprocedural recovery area (Fig. 39-4). The top of the head is in line with the edge of the operating bed for accessibility. The head should not be turned greatly in either direction; the head is stabilized in a ring-shaped pillow (donut). The patient’s gown is untied at the neck to prevent pressure. Any obstruction to venous circulation can cause undue increased IOP, which can produce a loss of vitreous humor when the eye is opened. To assist venous return from the head, the operating bed is tilted so the patient’s head is elevated by 5 to 10 degrees. For long procedures, an egg crate–type or gel pad mattress may be placed on the bed. Additional padding may be needed to position kyphotic or lordotic patients. 4. Skin preparation and draping procedures are performed according to routine. Sterile plastic drapes are often placed over woven textile drapes to contain lint, especially before lens implantation. A patient with a drape over the face is often apprehensive and afraid of suffocating. To help eliminate the feeling of claustrophobia, the drape can be placed over a Mayo stand or clipped to an intravenous pole to create a tentlike space above the patient’s nose and mouth (Fig. 39-5). Oxygen is delivered via nasal prongs or insufflated to the facial area beneath the drape at 6 to 8 L/min. An electrosurgical unit (ESU) is not to be used in an oxygen-rich environment because of the increased risk for ignition. 5. A quiet, stimulant-free environment is provided for the awake patient who is receiving a local anesthetic. 6. Because the patient has no defensive blink reflex to protect the retina from light exposure, some surgeons use a sterile, opaque pupillary shield to protect the patient’s retina from phototoxic damage caused by prolonged exposure to illumination of the microscope. Some scopes have a sensor near the eyepiece that dims the light source when the surgeon is not looking directly into the scope. The light reverts back to the desired intensity when the surgeon is positioned at the eyepiece. 7. The team should prepare for emergencies by anticipating problems. Fast action can make the difference between a seeing eye and a nonseeing eye postoperatively. The following are potential complications: a. A systemic reaction to medications or local anesthetic drugs and cardiac arrest. b. A loss of vitreous, which requires the removal of vitreous from the anterior chamber with a vitreotome to prevent prolapse of the wound, severe inflammation, or an updrawn pupil. c. An expulsive hemorrhage or an expulsion of ocular contents, which requires a sharp knife (e.g., Beaver blade, Wheeler knife) for fast cutdown into the pars plana area and an 18-gauge needle or cannula attached to a syringe to aspirate blood and reduce pressure in the vitreal compartment in an effort to save the eye and vision (Fig. 39-6). d. Instrument failure. Hand aspiration devices should be available for immediate use. 8. A wide variety of fine-size absorbable and nonabsorbable sutures is used. The scrub person follows the manufacturer’s recommendations for handling these delicate materials and needles with the appropriate needle holders. Special techniques are used in microsurgery. 9. Hemostasis is attained with bipolar cautery and a bipolar eraser pencil. Sponges are spear shaped and consist of precut compressed cellulose on sticks (Fig. 39-7). 10. No foreign material should be introduced into the surgical wound. In intraocular procedures, no portion of any instrument or item intended to enter the eye should be touched by a gloved hand. To remove any debris or impurity, intraocular lenses (IOLs) are soaked and rinsed in balanced salt solution (BSS) and sometimes lubricated with sodium hyaluronate (Healon) before insertion. 11. Inflammation should be kept as minimal as possible because even slight inflammation may result in total functional loss. Steroids are often administered locally, subconjunctivally, and, sometimes, systemically. The eye may respond violently to the slightest amount of trauma. 12. Antibiotic drops are often instilled topically for 24 hours preoperatively and postoperatively. 13. A sterile eye pad is commonly applied at the conclusion of the surgical procedure. A protective plastic or metal shield may be secured over the eye pad to guard against mechanical injury. Absorbable corneal shields may be used. 14. The patient should not be permitted to participate in the move from the operating bed after intraocular procedures; this prevents a sudden rise in IOP and/or dislocation of the IOL implant. 15. Arm restraints are essential for infants and young children. Restraints are applied to adults only under extreme circumstances, such as disorientation. The use of side rails is standard procedure for all patients undergoing ophthalmic surgery. The assistant observes the surgical procedure through an assistant’s ocular and irrigates the cornea with BSS to prevent drying (Fig. 39-13). The assistant should bring to the surgeon’s attention any potentially unsatisfactory situation that the surgeon cannot observe from his or her position. Some scrub persons are trained to first-assist. The surgeon and the assistants should limit their caffeine intake before the procedure to promote steady hands when using microinstrumentation under the microscope. 2. Identify the correct medication, eye, and patient. 3. Check for allergy or sensitivity. 4. Explain the procedure to the patient. 5. Tilt back the patient’s head, and tell the patient to look up. While gently pulling down on the lower lid, instill the medication in the middle third of the inner aspect of the lower lid. Release the lid while the patient slowly closes the eye to retain the drop; let the patient close the eye between repeated drops. In a struggling child, have a parent tilt the child’s head back and close both eyes. Instill the medication at the inner canthus. The drop will roll into the eye as the child opens it. Some medications, such as atropine, may have a systemic effect. To prevent drainage into the tear duct, nose, and stomach, gently blot excess fluid. In small infants or young children, systemic absorption is avoided by applying finger pressure over the lacrimal sac region (inner canthus) of both eyes simultaneously for 1 minute. 6. Administer only the specified number of drops. 7. Read the label on the vial before each instillation. 8. Each patient should receive a fresh, single-use, disposable vial of medication that is discarded after use. Medications may be given to alter the size of the pupil (Fig. 39-14), including the following: • Mydriatic drops: 2.5% or 10% phenylephrine (Neo-Synephrine) to dilate the pupil. • Mydriatic-cycloplegic drops: 1% cyclopentolate hydrochloride (Cyclogyl), 1% atropine, and 0.25% scopolamine (Isopto-Hyoscine) to dilate the pupil, paralyze the ciliary body, diminish the reaction to trauma, and prevent anterior synechiae (e.g., adherence of iris to the lens). These drugs are longer acting than phenylephrine. Except in children and select patients, local and topical anesthetics are commonly used for ophthalmic surgical procedures. Most surgical procedures are scheduled as monitored anesthesia care or attended local.4 An anesthesia provider monitors the patient and administers oxygen and/or supplements the local anesthetic if necessary. Intravenous midazolam (Versed) and/or fentanyl (Sublimaze) or propofol (Diprivan) is often given to relax the patient. The sedative effects of these agents increase the patient’s tolerance to procedures. If a general anesthetic is used, the usual general anesthesia routines are followed. Local anesthesia consists of the following: 1. Topical instillation of anesthetic drops. The drug used may be 0.5% proparacaine (Ophthaine), 0.5% tetracaine (Pontocaine), or 2% lidocaine (Xylocaine MPF [methylparaben-free]). Most surgeons prefer to use this method in combination with moderate sedation. 2. Local infiltration by injection of the lids and tissue around the eyes with anesthetic medication. 3. Retrobulbar block. An absolutely quiet eye is necessary, especially at high magnifications of the microscope. When general anesthesia is used, some surgeons administer a retrobulbar block for immobility and to lower IOP.4 A popular solution for this block consists of a mixture of equal parts of 2% or 4% lidocaine and 0.75% bupivacaine, 3.75 units/mL, for penetration. A 25-gauge × 1½-inch (3.8-cm) needle with a sharp, rounded point (e.g., Atkinson needle) and a 5-mL syringe are used. The surgeon inserts the needle behind the eyeball to anesthetize the globe and paralyze the muscles. The patient is asked to look up and away from the injection site and is told that a slight burning sensation may accompany the injection. Up to 5 mL of solution may be slowly and carefully injected. Retrobulbar block may be followed by intermittent massage of the eye to soften it, lower IOP, and facilitate surgical manipulation during cataract extraction, especially when insertion of an IOL is being contemplated. Massage is continued until the IOP is lowered to a satisfactory level (e.g., 10 to 12 scale reading on sterile Schiøtz tonometer). Some surgeons apply the Honan balloon pressure device to soften the eyeball after a retrobulbar block (Fig. 39-15). In using this device, a small inflatable balloon is placed directly over the closed eyelid and is secured with a strap around the head. The balloon is inflated to 30 to 40 mm Hg for 5 to 10 minutes to lower intravitreal pressure. 4. Peribulbar anesthesia. This is an alternative to retrobulbar injection. With this method, injections are made in the soft tissue superior and inferior to the globe rather than behind it. A greater amount of the same anesthetic solution used for retrobulbar injection is used for peribulbar anesthesia. With this procedure, adequate anesthesia is obtained without the risk for retrobulbar hemorrhage. For convenience, surgical treatment of the eye can be divided into two main classifications: 1. Extraocular. Conditions affecting the exterior surface of the eye, eyelid, or the orbit. 2. Intraocular. Conditions pertaining to the interior contents of the eye. The anatomy of the upper and lower eyelids is described in Figure 39-16. Tissue may be excised with a knife, an ESU, diathermy, or cryosurgery. An extremely common but benign tumor of the lid is the chalazion—a cystic alteration of one of the oil-secreting meibomian glands in the lid (Fig. 39-17, A). The resulting accumulation of oil forms a hard tumor of the lid and requires excision. The excision is usually an office or ambulatory surgical procedure. Chalazion is differentiated from a stye by the location on the lid. Styes are small infected lash follicles (see Fig. 39-17, B). Conditions such as senile ectropion or entropion most commonly affect the lower lid (Fig. 39-18). Ectropion is a condition in which either the upper or lower lid is everted (turned out) to expose the conjunctival surface. Entropion is the opposite condition, in which the lid margin is inverted (turned in). As a result, the eyelashes often abrade the cornea. Various procedures may be used to correct both conditions. A common result of aging is the stretching of the eyelid skin and the bulging of orbital fat from between the muscle fibers of the lids. Both conditions cause cosmetic disfigurement or baggy lids and, in extreme cases, may obstruct vision. In blepharoplasty, redundant folds of skin and herniated pockets of fat are removed, and defects in the muscle layer are repaired. Transconjunctival blepharoplasty is performed by making a small incision into the conjunctiva of the lower lid and removing fat pads. Small bleeders are cauterized with a disposable electrosurgical pencil. Blepharoplasty is commonly performed by plastic surgeons and is described in Chapter 40.
Ophthalmic surgery
Anatomy and physiology of the eye
Ophthalmic surgical patient care
Special features of ophthalmic surgery
Operating microscope
Ophthalmic drugs
Mydriatic and miotic drugs
Local and topical anesthesia
Ocular surgical procedures
Extraocular procedures
Eyelid
Excision of neoplasm of the eyelid.
Repair of acquired malformation of the eyelid.
Blepharoplasty.
Ophthalmic surgery

 Website
Website