National Institute of Health Criteria for Obesity Surgery
•BMI > 40
•BMI > 35 with one or more obesity-related comorbidities
•Comorbidities include a history of diabetes, hypertension, or degenerative joint disease
•Failed previous attempts at non-surgical weight reduction
•No active alcohol or substance abuse
•Realistic expectations of outcomes
•Commitment to long-term vitamin supplementation and follow-up
•Acceptable risk for surgery
A 37-year-old woman comes to your office requesting a gastric bypass operation. She has a BMI of 36. Her past medical history consists of diabetes mellitus, hypertension, and depression. She has attempted various diets and exercise programs only to regain her weight and more. Does she qualify for surgery?
The patient qualifies for obesity surgery because her patient’s BMI is >35 and she has multiple comorbidities. However, be mindful of patients with depression or an endocrine etiology for weight gain. Guidelines established by the American Society of Bariatric Surgeons (ASBS) include preoperative psychological evaluation. This helps identify those who have unrealistic expectations or are unable to give informed consent. Weight gain caused by an endocrine disorder, though rare, must be identified and dealt with prior to considering surgical intervention. Examples include patients with a history of MEN I (hyperparathyroidism, insulinoma, or pituitary adenoma). Most bariatric centers emphasize the importance of a multidisciplinary approach to patient screening and education. This includes evaluation by a dietician, psychologist, and internist (for preoperative risk assessment), and a sleep study if sleep apnea is suspected.
A 32-year-old obese but otherwise healthy male (BMI = 42) has undergone comprehensive preoperative testing for obesity surgery. His insurance company has approved the procedure. He comes today to discuss his surgical options. The dietician noted that this patient is a sweet eater and consumes milkshakes as his main source of protein. What are the different surgical options and which would you recommend for this patient?
A variety of surgical procedures have been developed to achieve weight loss, either by mechanical restriction of caloric intake through the creation of a small gastric reservoir, or the induction of malabsorption by bypassing variable lengths of small bowel. Surgical options include laparoscopic adjustable gastric band, vertical sleeve gastrectomy, Roux-en Y gastric bypass, and biliopancreatic diversion/duodenal switch. This patient would benefit most from a gastric bypass. (In fact, 80% of bariatric (obesity) procedures in the United States are Roux-en Y gastric bypass procedures, though the vertical sleeve gastrectomy is becoming more popular.)
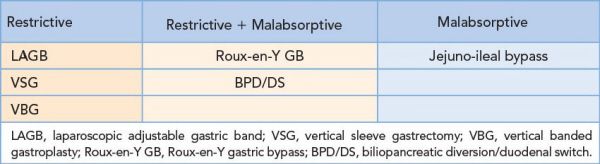
Bariatric surgical procedures can be classified as:
Roux-en-Y Gastric Bypass
•Operation of choice for obesity at most centers
•Produces both restriction and malabsorption (bypasses duodenum and proximal jejunum)
•Creates a small gastric pouch (20 to 30 mL) along the lesser curvature
•Includes a gastrojejunostomy utilizing a Roux-en-Y limb to empty the gastric pouch
•Average weight loss is 60% to 70% of excess body weight
•Maximal weight loss occurs in the first 2 years
•Obesity-related diseases (diabetes, hypertension, and sleep apnea) are dramatically reversed within the first year of surgery
•A laparoscopic approach is associated with a shorter length of stay and fewer complications (wound, infection, hernia, etc.)
•Complications
•Anastomotic leak—most commonly secondary to ischemia
•Small bowel obstruction
•Stenosis—responds to serial dilation
•Internal hernia
•Mesenteric defects should be closed to prevent this
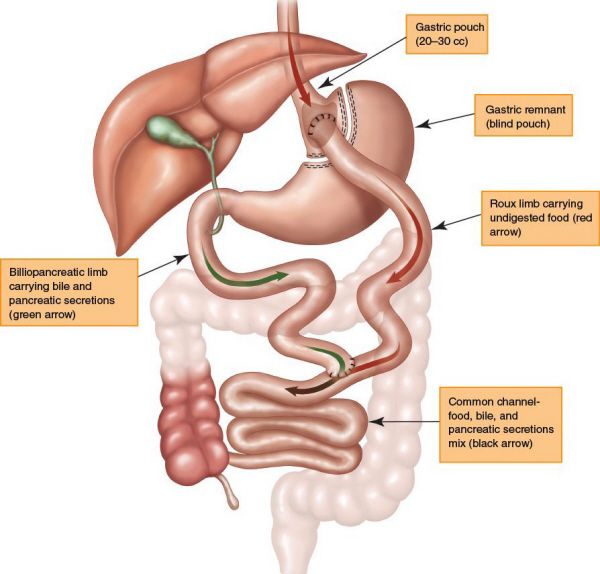
Roux-en-Y gastric bypass. (Reproduced with permission from Ethicon Endosurgery 2011.)
•Marginal ulcer near stomach anastomosis
•B12 deficiency
•Because IF needs an acidic environment to bind B12
•Iron deficiency
•Iron is absorbed in the duodenum, which is bypassed
•Gallstones—secondary to rapid weight loss
Laparoscopic Adjustable Band
•Only a restrictive procedure (not malabsorptive)
•A silastic collar or band is placed around the proximal stomach, creating a 15 mL pouch and a narrow adjustable outlet
•The outlet is adjusted by changing the volume of saline in a surgically placed subcutaneous reservoir to tighten or loosen the band
•Average weight loss approaches 45% to 50% of excess body weight
•Complications include band migration or erosion and malfunction of the subcutaneous port
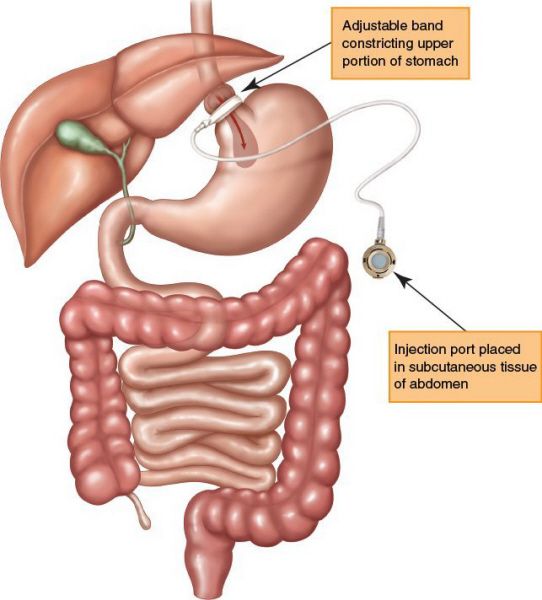
Laparoscopic adjustable gastric band. (Reproduced with permission from Ethicon Endosurgery 2011.)
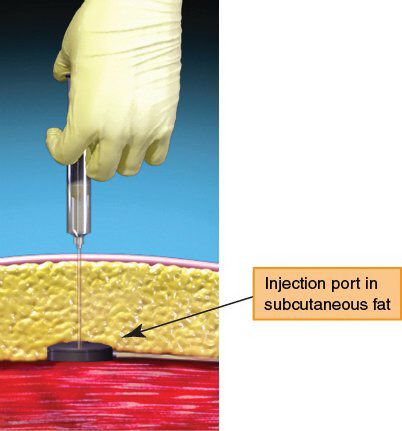
Laparoscopic adjustable gastric band adjustment. Adjustments are done by accessing the port which lies in the subcutaneous fat and is secured to the abdominal wall fascia. A Huber needle attached to a syringe is used to access the port. Sterile saline solution is used to fill the band. Fluid is removed from the band via the same technique. (Reproduced with permission from Ethicon Endosurgery 2011.)
Biliopancreatic Diversion/Duodenal Switch
•Achieves weight loss primarily through malabsorption
•A distal gastrectomy (80%) along the greater curvature is performed to create some restriction
•The distal small bowel is divided 250 cm proximal to the ileocecal valve
•The proximal end is rejoined to the ileum 50 cm proximal to the ileocecal valve
•The distal end is brought up and anastomosed to the duodenum
•Causes weight loss of up to 80% excess body weight
•The duodenal switch operation is a modification of the BPD
•The pylorus is preserved and the anastomosis is made to the duodenum instead of the stomach
•Appropriate candidates include the super-obese (BMI > 60) and those who have failed to lose weight with other obesity procedures
Vertical Banded Gastroplasty
•Entirely restrictive in nature
•Creates a small gastric reservoir or pouch measuring 15 to 20 mL in volume, which then empties into the residual stomach via a banded outlet
•The primary advantages of VBG are the avoidance of a gastrointestinal anastomosis and the preservation of normal gastroduodenal continuity
•Patients lose, on average, 40% to 50% of their excess body weight over 2 years
•Rarely performed in the 21st century
•Complications include pouch expansion, Marlex band migration or obstruction, and breakdown of the staple line that partitions the stomach
A 60-year-old male with DM, HTN, CAD s/p drug eluting stent placement in the LAD, and obstructive sleep apnea, has a BMI of 62. He has been referred to your clinic for evaluation. He is motivated and willing to go through the preoperative process for insurance approval. You find on inspection that most of his weight appears to be concentrated within his abdomen (central obesity). What operation would be the safest and easily performed in this type of patient?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


