DRUG CLASSES
Nonsteroidal anti-inflammatory
Selective serotonin agonists
PHARMACOLOGY IN PRACTICE

Mr. Park has osteoarthritis and has been taking buffered aspirin for almost a year. He is confused at times and has difficulty hearing; his hearing loss concerns his daughter, who is visiting from the coast. As you read about pain assessment and the NSAID drugs, consider whether changing to celecoxib for the osteoarthritis pain would be a consideration.
Because of the mode of action of nonsteroidal anti-inflammatory drugs (NSAIDs), some texts include the salicylates in the NSAID group. Although the chemical and physiologic effects are similar, this text discusses the salicylates in a separate chapter (see Chapter 13). Since NSAIDs are nonopioid analgesics like the salicylates, the NSAIDs have anti-inflammatory, antipyretic, and analgesic effects. The NSAIDs have emerged as important drugs in the treatment of the chronic pain and inflammation associated with disorders such as rheumatoid arthritis and osteoarthritis. Patients experiencing either acute or chronic pain are often undertreated because of an inadequate assessment. In this chapter pain assessment as well as general information on the NSAIDs is covered. NSAIDs are used for mild to moderate pain and are primarily taken on an outpatient basis; these drugs are listed in the Summary Drug Table: Nonsteroidal Anti-Inflammatory Drugs and Migraine Medications.
Pain Assessment
A key nursing role in administering pain relievers is a careful assessment of pain and the monitoring of the patient’s response to the pain medications. Over time pain assessment has taken a prominent place in any basic patient encounter. It is often considered the “fifth vital sign” in nursing assessment. To perform this component of your vital sign routine, two basic measures are needed in any pain assessment: location and intensity. Assessment of location helps the primary health care provider prescribe drugs that target the pain peripherally or centrally. The strength of the analgesic is determined by the patient’s report of the pain intensity.
The intensity of pain is subjective and individualized. Due to this subjectivity, it is sometimes difficult to measure objectively the signs of pain that match the level of distress reported by the patient. The patient’s description of pain should always be taken seriously. Because failure to assess pain adequately is a major factor in the undertreatment of pain, guidelines to help you form questions to ask the patient about pain are listed in Display 14.1.
Barriers to Assessment and Treatment
Pain management in acute and chronic illness is an important responsibility in nursing. As pain managers, you need to be aware of and overcome the three main barriers to proper pain management having to do with assessment, intervention, and evaluation:
• Primary health care providers do not prescribe proper pain medicine doses.
• Nurses do not administer adequate medication for relief of pain.
• Patients do not report accurate levels of pain.
You can lessen these barriers to good pain management by showing sensitivity to patient needs and learning techniques to conduct a good assessment.
Assessment Technique
As noted earlier, to prescribe effective analgesics for pain, the primary health care provider needs two key assessments about pain: location and intensity. To assess location, ask the patient to describe or point to where the pain is at; be cautious of labeling the pain, since pain on the jaw could be from either a tooth ache or referred pain. Help teach your patients to describe their pain (see Patient Teaching for Improved Patient Outcomes: Talking to Providers About Pain at the end of the chapter).
Display 14.1 Guidelines and Questions for a Pain Assessment
Known as the fifth vital sign, the assessment of pain is just as important as the assessment of temperature, pulse, respirations, and blood pressure. The following points help to guide your ability to assess pain.
Assessment Guidelines
• Patient’s subjective description of the pain (What does the pain feel like?)
• Location(s) of the pain
• Intensity, severity, and duration
• Any factors that influence the pain
• Quality of the pain
• Patterns of coping
• Effects of previous therapy (if applicable)
• Nurses’ observations of patient’s behavior
Sample Assessment Questions
Questions to include in the assessment of pain may include the following:
• Does the pain keep you awake at night? Prevent you from falling asleep or staying asleep?
• What makes your pain worse? What makes it better?
• Can you describe what your pain feels like? Sharp, stabbing, burning, or throbbing?
• Does the pain affect your mood? Are you depressed? Irritable? Anxious?
• What over-the-counter or herbal remedies have you used for the pain?
• Does the pain affect your activity level? Are you able to walk? Perform self-care activities?
Standardized pain measurement tools are used to provide consistency in assessing intensity (see examples in Fig. 14.1). The most common method used is to have a patient rate the pain on a scale of 0 to 10, with 0 being “no pain” and 10 being the “most severe pain imagined” by the patient.
Some population groups are known to have difficulty in assigning a number value to pain. For these patients it is hard to think about their pain experience in a quantitative manner, like assigning a number to it. Display 14.2 gives examples of populations you should note may need alternate pain assessment tools. As with any group or individual suspected of limited health literacy, alternate ways to describe pain intensity are offered. All these tools help to assess the pain of patients no matter whether they are being treated with strong opioids or nonopioid analgesics such as the NSAIDs.
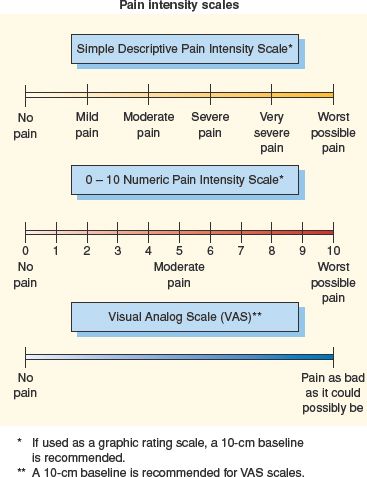
Figure 14.1 Examples of standardized pain assessment tools. (From Smeltzer SC, Bare BG. Brunnar & Suddarth’s textbook of medical-surgical nursing [9th ed.]. Philadelphia: Lippincott Williams & Wilkins, 2000.)
NONSTEROIDAL ANTI-INFLAMMATORY DRUGS
Actions
The NSAIDs are so named because they have anti-inflammatory effects, but they do not belong to the steroidal group of substances and thus do not possess the adverse reactions associated with the steroids (see Chapter 43). In addition, NSAIDs have analgesic and antipyretic properties. Although their exact mechanisms of action are not known, the NSAIDs are thought to inhibit prostaglandin synthesis by blocking the action of the enzyme cyclooxygenase, an enzyme responsible for prostaglandin synthesis. The NSAIDs also inhibit the activity of two related enzymes:
• cyclooxygenase-1 (COX-1), an enzyme that helps to maintain the stomach lining
• cyclooxygenase-2 (COX-2), an enzyme that triggers pain and inflammation
The traditional NSAIDs, such as ibuprofen and naproxen, are thought to regulate pain and inflammation by blocking COX-2. However, these drugs also inhibit COX-1, the enzyme that helps maintain the lining of the stomach. When NSAIDs are taken they block the effects of COX-2, producing pain relief, but they also block the effects of COX-1, which in turn produces adverse reactions. This inhibition of COX-1 causes unwanted gastrointestinal (GI) reactions such as stomach irritation and ulcers. Combination drugs (that include a proton pump inhibitor) are being used to reduce the risk of gastric and duodenal ulcers.
The NSAID celecoxib (Celebrex) appears to work by specifically inhibiting the COX-2 enzyme without inhibiting the COX-1 enzyme. Celecoxib relieves pain and inflammation with less potential for GI adverse reactions.
Display 14.2 Populations at Higher Risk for Poor Pain Assessment
Patients at risk for inadequate pain management are frequently those who are not assessed well. Consider using standardized visual analog tools to assess pain in these high-risk patient populations:
• Infants and children
• Older adults, especially those cognitively impaired
• Developmentally disabled children and adults
• Those with communication problems such as limited English proficiency or limited health literacy
• Those unable to communicate due to the illness or treatment process
 NURSING ALERT
NURSING ALERT
Celecoxib is associated with an increased risk of serious cardiovascular thrombosis, myocardial infarction, and stroke, all of which can be fatal. All NSAIDs may carry a similar risk. Always question the patient regarding a history of risk for actual cardiovascular disease before administering NSAIDs. Because of this risk, celecoxib should not be used to relieve postoperative pain from a coronary artery bypass graft (CABG).
Uses
The NSAIDs are used for the treatment of the following:
• Pain associated with musculoskeletal disorders such as osteoarthritis and rheumatoid arthritis
• Mild to moderate pain
• Primary dysmenorrhea (menstrual cramps)
• Fever (reduction)
Adverse Reactions
Gastrointestinal System Reactions
• Nausea, vomiting, dyspepsia
• Anorexia, dry mouth
• Diarrhea, constipation
• Epigastric pain, indigestion, abdominal distress or discomfort, bloating
• Intestinal ulceration, stomatitis
• Jaundice
Central Nervous System Reactions
• Dizziness, anxiety, lightheadedness, vertigo
• Headache
• Drowsiness, somnolence (sleepiness), insomnia
• Confusion, depression
• Stroke, psychic disturbances
Cardiovascular System Reactions
• Decrease or increase in blood pressure
• Congestive heart failure, cardiac arrhythmias
• Myocardial infarction
Renal System Reactions
• Polyuria (excessive urination), dysuria (painful urination), oliguria (reduced urine output)
• Hematuria (blood in the urine), cystitis
• Elevated blood urea nitrogen (BUN)
• Acute renal failure in those with impaired renal function
Hematologic System Reactions
• Pancytopenia (reduction in blood cell components), thrombocytopenia (reduced platelet count)
• Neutropenia (abnormally few neutrophils), eosinophilia (low eosinophil count), leukopenia (reduced white blood cell count), agranulocytosis (reduced granulocyte count)
• Aplastic anemia
Integumentary System Reactions
• Rash, erythema (redness), irritation, skin eruptions
• Ecchymosis (subcutaneous hemorrhage), purpura (excessive skin hemorrhage causing red-purple patches under the skin)
• Exfoliative dermatitis, Stevens-Johnson syndrome
Metabolic/Endocrine System Reactions
• Decreased appetite, weight increase or decrease
• Flushing, sweating
• Menstrual disorders, vaginal bleeding
• Hyperglycemia or hypoglycemia (high or low blood sugar)
Sensory and Other Reactions
• Taste change
• Rhinitis (runny nose)
• Tinnitus (ringing in the ears)
• Visual disturbances, blurred or diminished vision, diplopia (double vision), swollen or irritated eyes, photophobia (sensitivity to light), reversible loss of color vision
• Thirst, fever, chills
• Vaginitis
Contraindications
The NSAIDs are contraindicated in patients with known hypersensitivity. There is a cross-sensitivity to other NSAIDs, meaning if a patient is allergic to one NSAID, there is an increased risk of an allergic reaction with any other NSAID. Hypersensitivity to aspirin is a contraindication for all NSAIDs. In general, NSAIDs are contraindicated during the third trimester of pregnancy and during lactation. Some NSAIDs are not used to treat rheumatoid arthritis or osteoarthritis; these include ketorolac, mefenamic, and meloxicam. Celecoxib is contraindicated in patients who are allergic to sulfonamides or have a history of cardiac disease or stroke. Ibuprofen is contraindicated in those who have hypertension, peptic ulceration, or GI bleeding.
Precautions
The NSAIDs should be used cautiously during pregnancy (pregnancy category B), by older adults (increased risk of ulcer formation in patients older than 65 years), and by patients with bleeding disorders, renal disease, cardiovascular disease, or hepatic impairment.
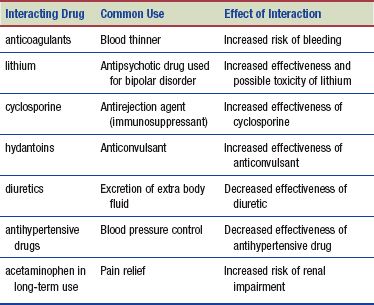
Interactions
The following interactions may occur when an NSAID is administered with another agent:
 HERBAL CONSIDERATIONS
HERBAL CONSIDERATIONS
Capsicum (hot pepper) has been cultivated in almost every society. Peppers are valued as a spice and flavoring for food. Capsaicin is the substance in peppers that, when applied topically, produces sensations varying from warmth to burning. For years, herbalists assumed that capsaicin worked by simply dilating blood vessels and increasing the supply of nutrients to injured joints. That may be a factor, but capsaicin actually works in a very different way.
People suffering from osteoarthritis have elevated levels of decapeptide substance P (DSP) in their blood and in the synovial fluid that bathes their joints. DSP has two undesirable functions. First, it breaks down the cartilage cushions in joints, contributing to osteoarthritis. Second, it serves as a pain neurotransmitter in both osteoarthritis and rheumatoid arthritis.
Researchers have discovered that capsaicin inhibits the activity of DSP. A cream containing capsaicin, when rubbed on the skin, penetrates to arthritic joints, where it stops the destruction of cartilage, relieves pain, and increases flexibility. Side effects include a localized burning sensation during the first few weeks of use, which diminishes with continued application.
People suffering from ulcers are usually warned to avoid spicy foods. But new research suggests that capsaicin produces the opposite effect—that capsaicin might actually protect against peptic ulcers. A number of experiments over the years have found that capsaicin protects the gastric mucosal membrane against damage from alcohol and aspirin (DerMarderosian, 2003).
DRUGS USED IN THE TREATMENT OF MIGRAINE HEADACHES
Pain associated with migraine headaches is believed to be caused by vascular spasms. Drugs used to treat migraine headaches are given (1) prophylactically to prevent the spasms or (2) to treat the acute pain when a migraine occurs. The mechanism of action and classification of the drugs to prevent migraine headaches are different from those used to treat the acute pain of the migraine attack. Prophylactic treatment may include drugs from the following categories: beta (β) blockers (see Chapter 25), calcium channel blockers (see Chapter 35), antidepressant medications (see Chapter 22), or anticonvulsant drugs (see Chapter 29). The selective serotonin (5-HT) agonists used to relieve the acute pain are covered in this chapter and are listed in the Summary Drug Table: Nonsteroidal Anti-Inflammatory Drugs and Migraine Medications.
Actions and Uses
The symptoms of migraine headaches are believed to be caused by local cranial vasodilation and stimulation of trigeminal nerves. Activation of the 5-HT receptors causes vasoconstriction and reduces the neurotransmission, which in turn produces pain relief. Selective serotonin drugs are used for the relief of moderate to severe pain and inflammation related to migraine headaches. Because reduced GI motility can happen during a migraine event, delayed absorption of oral drugs may occur and alternative routes of administration are needed: rectal, internasal, or subcutaneous injection.
Adverse Reactions
These agents are generally well tolerated, with most adverse reactions mild and transient. The most common are dizziness, nausea, fatigue, pain, dry mouth, and flushing.
Cardiovascular System Reactions
• Coronary artery vasospasm
• Cardiac arrhythmias and tachycardia
• Myocardial infarction
Contraindications and Precautions
These drugs are contraindicated in patients with a known hypersensitivity to selective serotonin agonists and should only be used when a clear diagnosis of migraine headache has been established. 5-HT agonists should not be used in patients with ischemic heart disease (such as angina or myocardial infarction), transient ischemic attacks (TIAs), or uncontrolled hypertension or those patients taking monoamine oxidase inhibitor (MAOI) antidepressants. These drugs should be used cautiously in patients with hepatic or renal function impairment, such as the elderly or patients requiring dialysis. Because these are pregnancy category C drugs, they should only be used during pregnancy when the benefit outweighs the risk to the fetus. Caution should be exercised when administering them to lactating mothers.
The ergot derivatives (see Summary Drug Table: Nonsteroidal Anti-Inflammatory Drugs and Migraine Medications) should not be used by HIV patients using protease inhibitors or patients taking macrolide antibiotics due to the risk of peripheral ischemia.
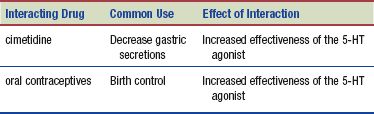
Interactions
The following interactions may occur when a selective serotonin drug is administered with another agent:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


