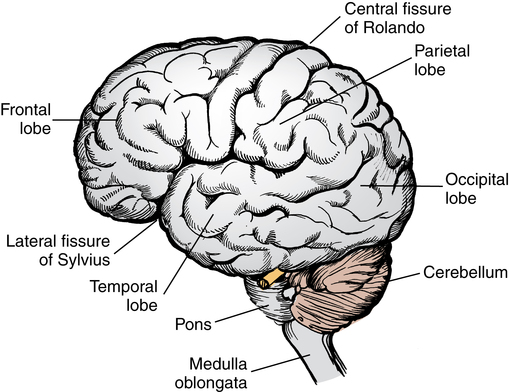
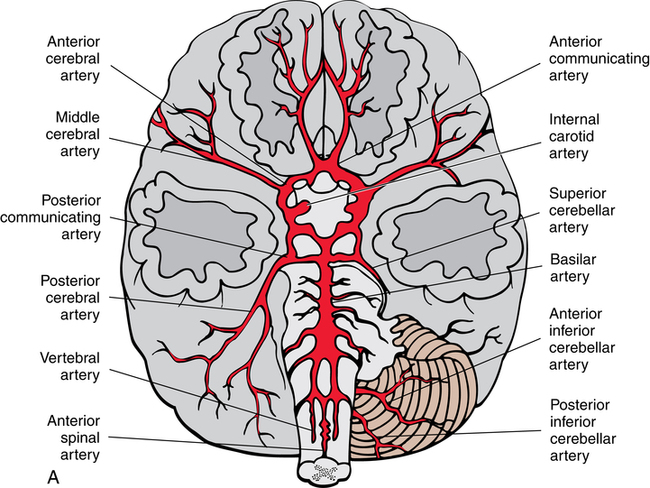
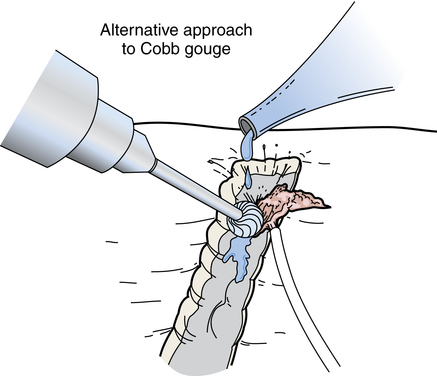
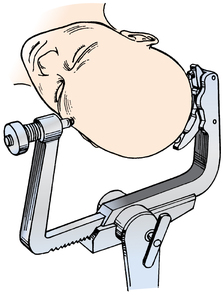
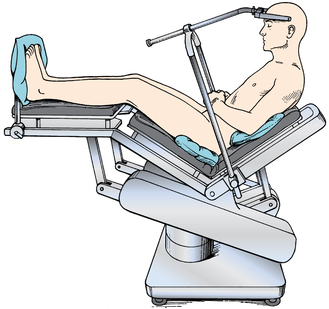
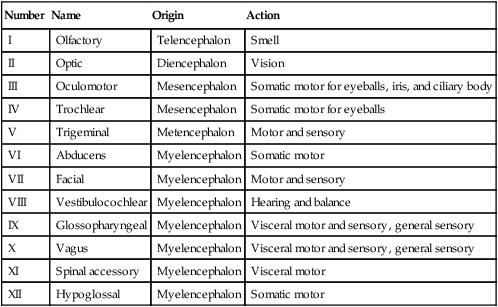
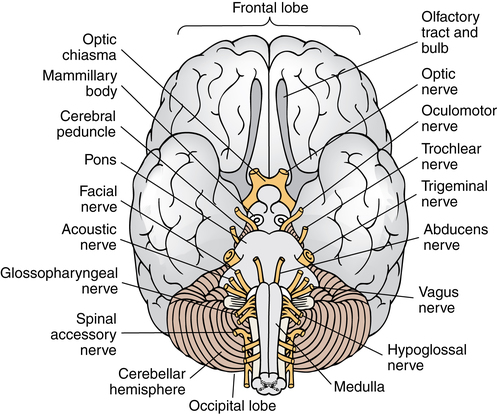
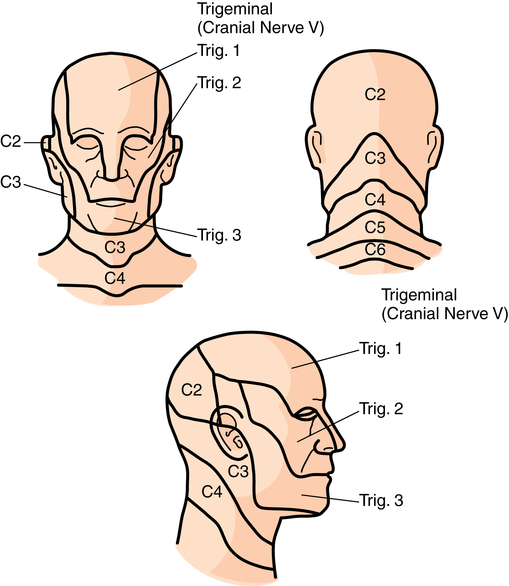
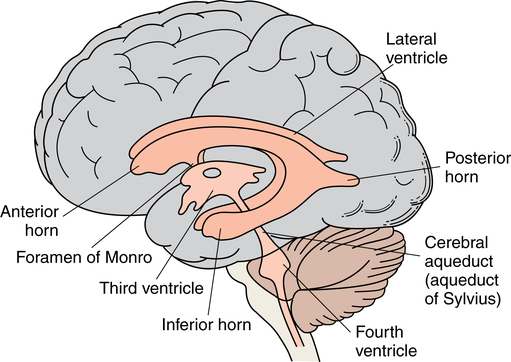
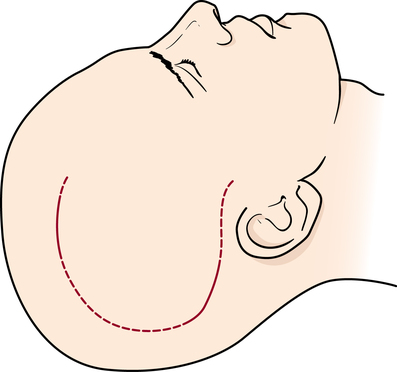
Chapter 37 After studying this chapter, the learner will be able to: • Identify the pertinent anatomy of the brain and spinal cord. • Describe the significance of neurologic monitoring. An understanding of basic anatomy and physiology is essential for preparing for the approach used to reach intracranial and spinal cord structures. The brain is divided into five main subdivisions composed of gray matter (neurons, cell bodies) and white matter (axons, dendrites, nerve fibers). The brain has three distinct anatomic units that consist of several subdivisions, as shown in Figure 37-1. The cranial nerves (Table 37-1) originate from several locations in the brain and its subdivisions (Fig. 37-2). Cranial nerve V (trigeminal) innervates most of the face in correlation with cervical dermatomes (Fig. 37-3). TABLE 37-1 The blood supply to the brain is derived from the carotid and vertebral arteries. The arterial component collectively joins at the circle of Willis (Fig. 37-4). The venous drainage is a series of valveless, bidirectional venous sinuses that communicate directly with the vertebral venous sinuses. The patterns of infectious spread and metastasis can be easily noted via the venous system that ranges from the pelvis to the cranium.7 1. The frontal lobe lies within the anterior fossa. 2. The parietal lobe lies in the superior and anterior portion of the middle fossa. 3. The temporal lobe lies inferior to the frontal and parietal lobes within the middle fossa. 4. The occipital lobe lies posteriorly within the middle fossa. Four spaces within the brain are referred to as ventricles (Fig. 37-5). The lateral ventricles, one in each hemisphere of the cerebrum, drain into the foramen of Monro. The foramen of Monro opens into a central cavity, the third ventricle, which is connected by the aqueduct of Sylvius, with the fourth ventricle lying anterior to the cerebellum and posterior to the brainstem. CSF is a clear substance produced in the choroid plexuses, which are vascular extensions of the pia mater lining the ventricles. CSF is predominantly produced in the lateral ventricles and circulates through the subarachnoid space around the meninges covering the brain and spinal cord. The normal adult volume of circulating CSF is 125 to 150 mL. Obstruction of the CSF flow causes increased ICP. The hemostatic methods commonly used by neurosurgeons for most procedures include the following. A side-viewing fiberoptic endoscope may be used to enhance visibility at obscure angles in otherwise visually inaccessible areas. This endoscope is particularly useful for identification of lesions in the sella turcica, cerebral aneurysms, and intervertebral discs, for example.12 An endoscope may be used for placement of electrodes for stimulators or a catheter for radioisotopes. The argon laser can be used through a ventriculoscope for intraventricular obliteration of the choroid plexuses and for intravascular treatment of lesions and neoplasms. The Nd:YAG laser can be used through a flexible or rigid neuroscope to vaporize a cyst. A straightforward, rigid, zero-degree scope may be used for electrocoagulation or laser obliteration of tissue and to obtain a CT-assisted stereotactic biopsy.8,12 Preparation of the patient in the OR usually begins with clipping of hair with electric clippers. Hair on the head is considered the patient’s personal property. When all of it is removed, it is saved. Hair removal and its disposition are documented on the patient’s chart. Demarcation of the desired outline for the incision may be made on the scalp after the skin preparation and before draping. A sterile disposable skin marker is available (Fig. 37-7). The Mayfield skull clamp provides stability that is necessary for microsurgical procedures and is desirable during lengthy procedures. This eliminates the risk of pressure-related complications around the face or eyes with the patient prone or in a lateral position. Three pins on the skull clamp partially penetrate the outer table of the skull. Pins on one side may be spring-loaded (Fig. 37-8) to join the skull and the clamp into one rigid mechanical unit. When pin fixation is used, antibiotic ointment is applied around each fixation pin to form an airtight seal. This reduces the risk of air embolism and infection.7 The circulating nurse should be familiar with the desired neurosurgical positions and the headrests, skull clamps, and attachments for each. The patient is anesthetized in a supine position on the transport cart and turned prone onto the OR bed. A detailed description of prone positioning is found in Chapter 26 of this text. The eyes are lubricated, and the lids are taped closed for protection. The patient’s transport cart should be immediately available in the event of the need for cardiac resuscitation. The patient needs to be placed supine in a rapid manner, and the nearby cart facilitates this maneuver. For a posterior approach, a head holder supports the forehead. The seated position allows greater torsion and flexion of the neck than either a lateral or the prone position and a more accessible approach to the cerebellopontine angle (Fig. 37-9).
Neurosurgery of the brain and peripheral nerves
Anatomy and physiology of the brain
Brain
Number
Name
Origin
Action
I
Olfactory
Telencephalon
Smell
II
Optic
Diencephalon
Vision
III
Oculomotor
Mesencephalon
Somatic motor for eyeballs, iris, and ciliary body
IV
Trochlear
Mesencephalon
Somatic motor for eyeballs
V
Trigeminal
Metencephalon
Motor and sensory
VI
Abducens
Myelencephalon
Somatic motor
VII
Facial
Myelencephalon
Motor and sensory
VIII
Vestibulocochlear
Myelencephalon
Hearing and balance
IX
Glossopharyngeal
Myelencephalon
Visceral motor and sensory, general sensory
X
Vagus
Myelencephalon
Visceral motor and sensory, general sensory
XI
Spinal accessory
Myelencephalon
Visceral motor
XII
Hypoglossal
Myelencephalon
Somatic motor
Cerebrum
Ventricles
Special considerations in neurosurgery
Methods of hemostasis
Adjuncts to visibility
Endoscope
Patient care considerations for craniotomy
Patient preparation
Patient positioning
Prone position
Seated position
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Neurosurgery of the brain and peripheral nerves

 Website
Website