Mixed Germ Cell Tumors
Steven S. Shen, MD, PhD
Jae Y. Ro, MD, PhD
Key Facts
Terminology
Germ cell tumor composed of > 1 histologic type of germ cell tumor, including seminoma
Clinical Issues
Accounts for 30-40% of all testicular germ cell tumors
Depends on clinical stage, proportion of embryonal carcinoma component, and lymphovascular invasion
Macroscopic Features
Variegated cystic and solid mass with hemorrhage and necrosis
Microscopic Pathology
Variable combination and percentage of all germ cell tumor components
Embryonal carcinoma (EC) and teratoma (T) are most common (26%)
Other combinations include teratoma and EC, teratoma with EC and yolk sac tumor (YST)
Areas of necrosis and hemorrhage are common
Rare special variants include polyembryoma and diffuse embryoma
Ancillary Tests
Immunoprofile reflects histologic component of different germ cell tumors
1st-line germ cell markers: Oct3/4, CD30(BerH2), PLAP, cytokeratin
Top Differential Diagnoses
Pure germ cell tumor, such as EC, YST, or teratoma, and metastatic carcinoma
TERMINOLOGY
Abbreviations
Mixed germ cell tumor (MGCT), mixed nonseminomatous germ cell tumor (MNSGCT)
Synonyms
Mixed nonseminomatous germ cell tumor
Definitions
Germ cell tumor composed of > 1 histologic type of germ cell tumor, including seminoma
CLINICAL ISSUES
Epidemiology
Incidence
2nd most common germ cell tumor after seminoma
Accounts for 30-40% of all testicular germ cell tumors
Age
Range: 20-40 years (10 years younger than seminoma)
Rarely seen in prepubertal children and older adults (> 50 years)
Presentation
Testicular mass or swelling ± pain
Treatment
Similar to pure nonseminomatous germ cell tumor and depends on clinical stage
Radical inguinal orchiectomy ± retroperitoneal lymph node dissection or adjuvant therapy
Prognosis
Depends on clinical stage, proportion of embryonal carcinoma (unfavorable) and mature teratoma (favorable) component, and lymphovascular invasion
Cure rate > 95% for stage I and stage II disease
Cure rate approximately 70-85% for stage III disease
IMAGE FINDINGS
Radiographic Findings
Heterogeneous testicular mass on ultrasound examination
May be accompanied by retroperitoneal lymph node enlargement
MACROSCOPIC FEATURES
General Features
Variegated cystic and solid mass with hemorrhage and necrosis
Seminomatous germ cell component with solid white and gray areas
Nonseminomatous component with granular and firm areas with hemorrhage, necrosis, and cystic areas
Teratoma with bone, cartilage, and skin elements
Sections to Be Submitted
Multiple sections of different areas of tumor and at least 1 section per cm tumor
Should include necrotic and hemorrhagic areas
Size
Variable, often large bulky mass
MICROSCOPIC PATHOLOGY
Histologic Features
Variable combination and percentage of all germ cell tumor components
Embryonal carcinoma (EC) and teratoma (T) are most common (26%)
Other combinations include
EC and seminoma (S) (16%)
EC, yolk sac tumor (YST), and T (11%)
EC, T, and choriocarcinoma (CC) (7%)
EC, T, and S (6%)
T and S (6%)
EC and YST (4%)
EC and CC (4%)
Other combinations may occur (16%)
Areas of necrosis and hemorrhage are common
Rare variants include polyembryoma and diffuse embryoma
Polyembryoma is composed of entirely or predominantly embryoid bodies with embryonic disc, yolk sac, and surrounded by myxoid stroma
Diffuse embryoma is characterized by intimately admixture of EC and YST with YST wrapping around EC component
Cytologic Features
Reflects histologic composition of each component
Predominant Pattern/Injury Type
Neoplastic
Predominant Cell/Compartment Type
> 1 type of germ cell tumor component
ANCILLARY TESTS
Immunohistochemistry
Immunoprofile reflects histologic component of different germ cell tumors
1st-line germ cell markers: Oct3/4, PLAP, Podoplanin(D2-40), CD30(BerH2), α-fetoprotein, HCG, cytokeratin
Other germ cell markers: CD117, glypican-3, SALL4, NANOG
DIFFERENTIAL DIAGNOSIS
Pure Germ Cell Tumor
Such as embryonal carcinoma, yolk sac tumor, or teratoma
Multiple sections are required to demonstrate different germ cell tumor components
Metastatic Carcinoma
Old age, history, and bilaterality
Interstitial pattern is frequently seen in metastatic carcinoma
Positive for EMA/MUC1; negative for germ cell tumor markers
DIAGNOSTIC CHECKLIST
Pathologic Interpretation Pearls
Mixture of different histologic components of germ cell neoplasm
REPORTING CONSIDERATIONS
Key Elements to Report
Specific histologic types and percentage of each component
Lymphovascular invasion
Involvement of rete testis, epididymis, spermatic cord, and tunica
Pathology of uninvolved testicular parenchyma
SELECTED REFERENCES
1. Berney DM et al: Malignant germ cell tumours in the elderly: a histopathological review of 50 cases in men aged 60 years or over. Mod Pathol. 21(1):54-9, 2008
2. Mosharafa AA et al: Histology in mixed germ cell tumors. Is there a favorite pairing? J Urol. 171(4):1471-3, 2004
3. Sesterhenn IA et al: Pathology of germ cell tumors of the testis. Cancer Control. 11(6):374-87, 2004
4. Ayala AG et al: Testicular tumors: clinically relevant histological findings. Semin Urol Oncol. 16(2):72-81, 1998
Image Gallery
Gross and Microscopic Features
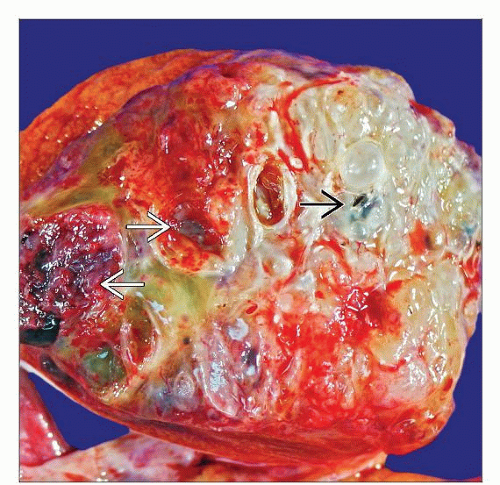
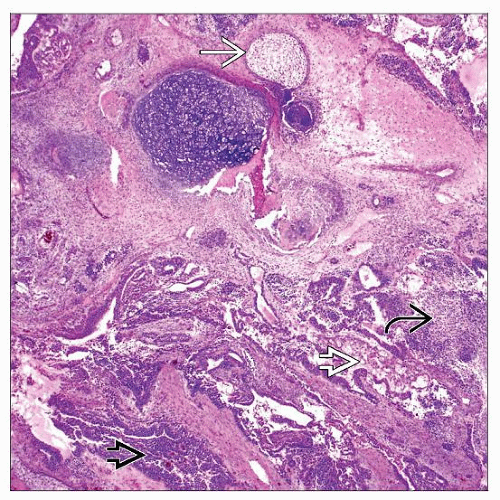
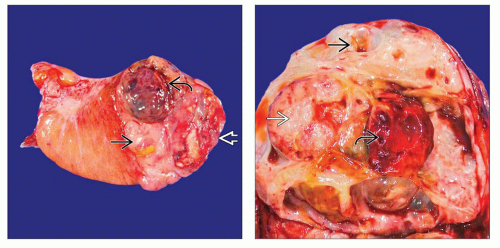 (Left) MGCT usually shows an irregular mass with variegated cut surface. Creamy gray lobulated areas suggest seminoma
 , mucoid areas suggest teratoma , mucoid areas suggest teratoma  , and hemorrhagic brown areas suggest EC , and hemorrhagic brown areas suggest EC  . Gross appearances are not absolutely specific for histologic subtype. (Right) MGCT with typical variegated cut surface is shown. The cystic mucoid areas represent mature teratoma . Gross appearances are not absolutely specific for histologic subtype. (Right) MGCT with typical variegated cut surface is shown. The cystic mucoid areas represent mature teratoma  , the tan fleshy area represents seminoma , the tan fleshy area represents seminoma  , and hemorrhagic and necrotic areas represent EC , and hemorrhagic and necrotic areas represent EC  . .Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|