Amyloid
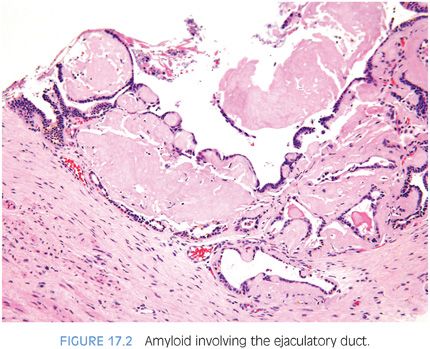
Vascular amyloid can be identified in 2% to 10% of prostates removed for hyperplasia or carcinoma.19–22 Patients with multiple myeloma, primary amyloidosis of the kidney, or chronic debilitating diseases have a higher incidence of prostatic amyloidosis. In these cases, amyloid is located in subepithelial areas as well as in vessels. Usually, amyloid within the prostate is an incidental finding, although rarely, it may mimic carcinoma on rectal examination. Amyloidosis, which involves the seminal vesicles in about 10% of radical prostatectomy specimens, can also extend into the ejaculatory duct and can be sampled on needle biopsy19 (Fig. 17.2, eFig. 17.2). Corpora amylacea often stain nonspecifically for amyloid.23
Calculi and Calcification
Prostatic calculi are found within the tissues or acini of the gland, in contrast to urinary calculi that are found within the prostatic urethra.24,25 Prostatic calculi are present in 70% to 100% of the glands studied at autopsy, most commonly in men older than 50 years of age. Generally, prostatic calculi are multiple and small with an average diameter of less than 5 mm. Histologically, calculi are composed of concentric layers resembling calcified corpora amylacea. They form by the consolidation and calcification of corpora amylacea or by calcification of precipitated prostatic secretions. Although prostatic calculi are common, they are usually asymptomatic and are discovered incidentally. Abscesses may occur in patients who have urinary tract infections resistant to antimicrobial therapy in which the prostatic calculi are infected and provide a continual source of infection. Prostatic calculi are also significant in that they may be confused on rectal examination with carcinoma of the prostate.
Basal cell hyperplasia is the most common lesion containing laminated calcifications resembling psammoma bodies. The latter have been encountered in approximately one-fifth of basal cell hyperplasia cases on needle biopsy.26,27 This finding may be a diagnostic aid, because only rarely do carcinomas contain laminated calcifications. Calcifications within prostate cancers tend to be small stippled granular calcifications in areas of central necrosis, most commonly seen in high-grade carcinomas and ductal adenocarcinomas.
Infarcts
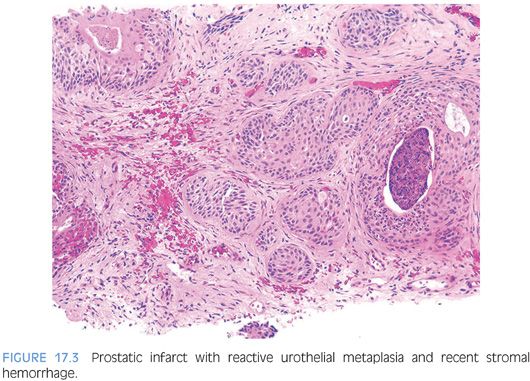
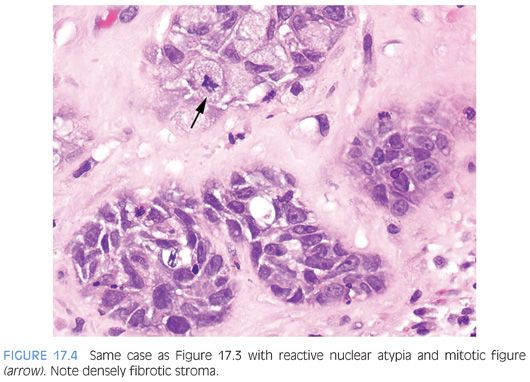
In between 20% and 25% of specimens removed for benign prostatic hyperplasia, prostatic infarcts ranging in size from a few millimeters to 5 cm may be found.28–30 Patients with acute prostatic infarcts have prostate glands that are twice as large as those without infarcts. Also, patients with infarcts are more prone to acute urinary retention and gross hematuria than those without infarcts. These symptoms, however, may not be due to the infarcts but rather may be due to the larger size of the gland containing them, because the infarcts are often small and not close to the urethra. Acute prostatic infarcts are discrete lesions with a characteristic histologic zonation (Figs. 17.3 and 17.4, eFigs. 17.3 to 17.21). The center of the infarct is characterized by acute coagulative necrosis and some recent hemorrhage. Immediately adjacent to the infarcted tissue, reactive epithelial nests with prominent nucleoli, some pleomorphism, and even atypical mitotic figures can be seen (Fig. 17.4). Progressing away from the center of the infarct, more mature squamous metaplasia is seen. Another finding seen within prostatic infarcts is squamous islands with central cystic formation containing cellular debris. Remote infarcts may also be recognized by finding local areas of densely fibrotic stroma admixed with small glands containing immature squamous metaplasia (eFig. 17.22). Prostatic infarcts may rarely be sampled on needle biopsy, where it may be more difficult to appreciate the zonation.29 If the infarct is not recognized, the reactive squamous metaplasia cases may be misdiagnosed as urothelial carcinoma.
Miscellaneous
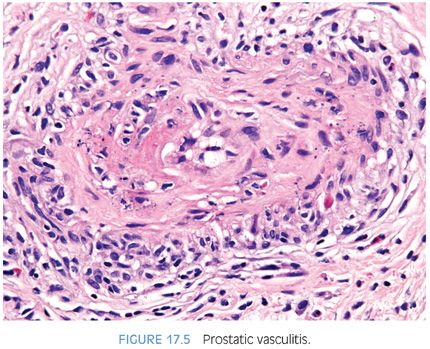
In a study of prostates from a medical examiner’s office, 9% of prostates contained sperm (eFig. 17.23).31 Spermatozoa have been found in approximately one-quarter of whole mount–examined prostatectomies with the aid of special stains.32 Rare cases of prostatic endometriosis, hair granuloma, and lymphangiolipomatosis have been diagnosed.33–35 Vasculitis involving the prostate may occur, including polyarteritis nodosa, Wegener granulomatosis, and giant cell arteritis36–38 (Fig. 17.5, eFigs. 17.24 to 17.26). Extramedullary hematopoiesis, ganglioneuroma, and ectopic salivary gland tissue have been described in the prostate.39–41 A form of metaplasia has been designated “Paneth cell-like metaplasia” or “Paneth cell-like change.”42–44 Histologically, it is characterized by bright eosinophilic neuroendocrine granules filling the apical cytoplasm. The cells are immunoreactive with neuroendocrine markers and some have suggested the use of the alternative terminology of neuroendocrine cells with large eosinophilic granules.44,45 We prefer the term Paneth cell-like neuroendocrine differentiation, which may also be seen in prostatic adenocarcinoma that was previously discussed in Chapter 12.46
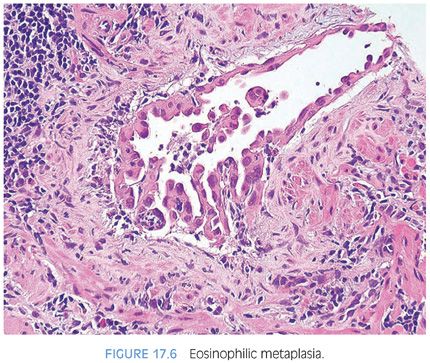
Another form of cytoplasmic metaplastic change that occasionally occurs in benign acini is “eosinophilic metaplasia” (Fig. 17.6, eFig. 17.27).47
Rarely, the ejaculatory duct may be a site of pathology. Cases of an adenofibroma and an adenomatoid tumor involving this structure have been reported.48,49
Finally, a rare case of benign prostatic hyperplasia occurring in an adolescent or pediatric patient have been reported and termed juvenile prostatic hyperplasia.50,51
MALIGNANT LESIONS
Basal Cell Carcinomas
At the other end of the spectrum of basal cell hyperplasia (see Chapter 7) of the prostate is basal cell carcinoma.52–55 The histologic variability of basal cell carcinomas of the prostate is greater than that of basal cell hyperplasia. They may resemble basal cell carcinomas of the skin with large basaloid nests, peripheral palisading, and necrosis (Fig. 17.7, eFig. 17.28). Other basal cell carcinomas resemble the adenoid basal cell pattern of basal cell hyperplasia26,56 and have been referred to by some as adenoid cystic carcinoma of the prostate56,57 (Fig. 17.8, eFigs. 17.29 to 17.34).
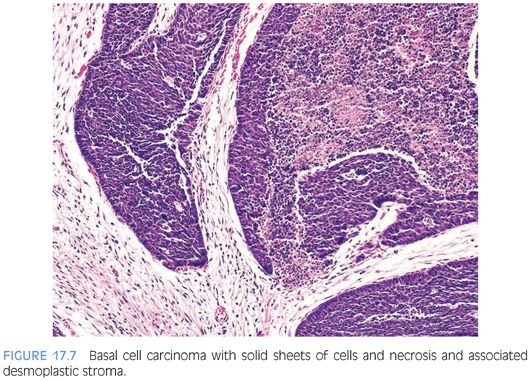
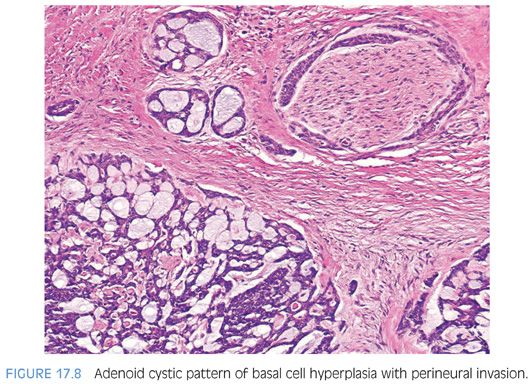
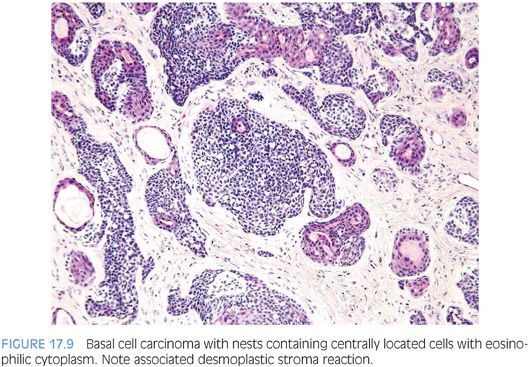
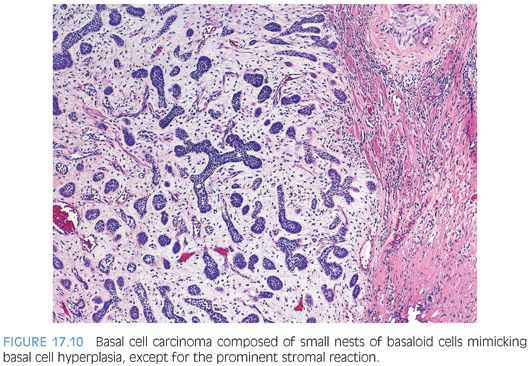
In addition to the adenoid cystic pattern and large basaloid nests with necrosis being pathognomonic of basal cell carcinoma, we have noted two other patterns that were only seen with basal cell carcinoma and not basal cell hyperplasia26,27,52,58 (Table 17.1). One was the finding of anastomosing basaloid nests and tubules centrally lined by eosinophilic cells (Fig. 17.9, eFigs. 17.35 to 17.38). A more subjective assessment of architecture that we identified only in basal cell carcinoma was variably small/medium-sized nests with irregular shapes (Fig. 17.9, eFig. 17.39). Infiltrativeness is another characteristic of basal cell carcinoma that in some cases may be difficult to assess. Although readily diagnostic of malignancy, extension of basal cell carcinoma into periprostatic adipose tissue or seminal vesicles is typically seen in resection rather than diagnostic specimens. More commonly, infiltration in basal cell carcinoma manifests by extension into the thick muscle bundles of the bladder neck, which is not seen in basal cell hyperplasia (eFig. 17.39). A more problematic diagnostic criterion of basal cell malignancy is widespread infiltration of the malignant basal elements between benign prostatic glands (eFigs. 17.40 to 17.42). Florid basal cell hyperplasia may also appear infiltrative between benign glands, although it may represent focal basal cell hyperplasia arising amongst benign prostatic glands, giving the impression of an infiltrative process (eFig 17.43). In contrast to basal cell carcinoma, the nests or tubules of basal cell hyperplasia are more evenly and orderly arranged between benign prostate glands and tend not to infiltrate as isolated units but rather as clusters of nests or tubules. In summary, although basal cell carcinoma can occasionally resemble basal cell hyperplasia, the diagnosis of malignancy is usually based on either (a) extensive infiltration in between normal prostate glands, (b) extension out of the prostate, (c) perineural invasion, (d) necrosis, or (e) the presence of a dense stromal response (Fig. 17.10, eFig. 17.44). Florid basal cell hyperplasia may have a subtle myxoid stromal reaction but lacks the extensive myxoid or desmoplastic reaction that characterizes some basal cell carcinomas.26 Other findings that may be seen in association with basal cell carcinoma include collagenous globules, squamous differentiation (eFig. 17.45), focal microcalcifications, and vacuoles.
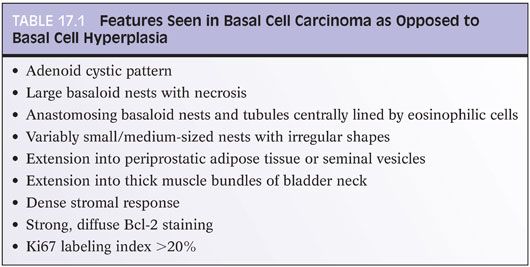
Bcl-2 labels basal cell carcinoma more strongly and diffusely than basal cell hyperplasia55 (eFig. 17.46). Ki67 staining is greater than 20% in approximately one-half of basal cell carcinomas52 (eFig. 17.47). Immunohistochemistry for ki67 can be helpful in differentiating basal cell carcinoma from florid basal cell hyperplasia, as basal cell hyperplasia typically shows less than 5% positivity.55 Basal cell markers (p63, high molecular weight cytokeratin) may highlight multiple cell layers, just the outermost layers or only a few scattered cells with some basal cell carcinomas being negative for high molecular weight cytokeratin (eFigs. 17.48 and 17.49). Overall, only a small subset of basal cell carcinomas behaves aggressively with local recurrences and distant metastases. In previously reported cases, these have been of the adenoid cystic variant.57,59,60 In our more recent series, among those with an aggressive behavior, the predominant pattern were cases with large solid nests more often with central necrosis, high Ki67 percentage, and less staining with basal cell markers (eFig. 17.50).52
Carcinomas with Squamous Differentiation
Pure squamous cell carcinomas develop osteolytic metastases, do not respond to estrogen therapy, and do not develop elevated serum acid phosphatase levels with metastatic disease (eFig. 17.51).61,62 Metastases also are seen in the liver, lung, and lymph nodes. Serum PSA levels are not elevated. The diagnosis of primary prostatic squamous cell carcinomas requires (a) lack of glandular differentiation, (b) no prior hormonal therapy, and (c) absence of secondary involvement of the gland by bladder or urethral squamous carcinomas. Squamous cell carcinoma of the prostate must also be differentiated from squamous metaplasia adjacent to a prostatic infarct (see earlier discussion). Primary prostatic squamous cell carcinomas have a poor prognosis with an average survival of about 1 year. Treatment is multimodal with surgery, chemotherapy, and radiation.
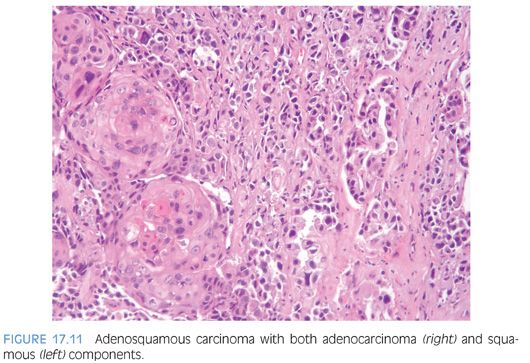
Adenosquamous carcinomas may also be seen in the prostate with and without a prior history of endocrine and/or radiation therapy (Fig. 17.11, eFig. 17.52).63,64 In the largest series reported on adenosquamous carcinomas of the prostate (33 cases from two institutions), the majority of the tumors occurred in patients with a prior established diagnosis of prostatic adenocarcinoma. Approximately one-half of the patients had received prior hormonal therapy and/or radiotherapy.65 The squamous components only rarely demonstrated focal positivity for PSA or PSAP. Diffuse positivity for high molecular weight cytokeratin was encountered in the squamous components of the tumors. The average survival was 24 months (see also Chapter 14).
Sarcomatoid Carcinoma
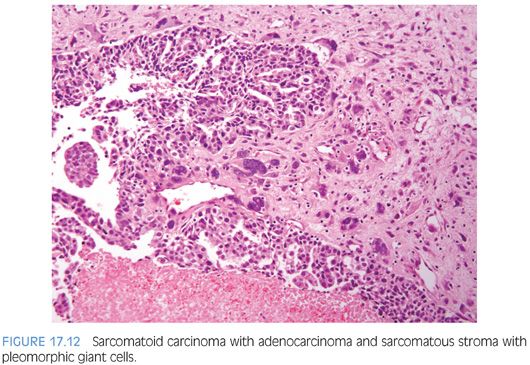
Sarcomatoid carcinoma (carcinosarcoma) is a rare type of prostatic cancer with approximately 100 cases reported in the literature, most reported in three large series of 42, 21, and 12 patients, respectively (Figs. 17.12 and 17.13, eFigs. 17.53 to 17.56).66–68 Tumors are most commonly composed of an admixture of both malignant glandular and spindle cell elements, in which cases with predominantly a sarcomatoid component may be mistaken for a sarcoma. Patients with sarcomatoid carcinoma often have a history of acinar adenocarcinoma of the prostate, although in some cases, the diagnosis may have been as remote as 16 years prior. In our study, the vast majority of patients with known treatment history following the original diagnosis of acinar adenocarcinoma had received external beam radiation, brachytherapy, and/or hormone therapy.67 The interval between the diagnosis of acinar adenocarcinoma and sarcomatoid carcinoma ranged from 6 months to 16 years (mean 6.8 years). Patients are on average about 70 years old. They typically present with urinary tract obstruction and its symptoms. On digital rectal examination, the palpable prostate is often enlarged, nodular, and hard. PSA elevations are variable. Morphologically, sarcomatoid carcinoma demonstrates a variety of patterns. Typically, the glandular component is composed of high-grade acinar adenocarcinoma or an unusual subtype of prostatic carcinoma (small cell, foamy gland, basal cell, ductal, or adenosquamous carcinoma). The sarcomatoid component, which may account for as little as 5% of the tumor, usually demonstrates frank malignant features including hypercellularity, nuclear atypia, frequent mitoses, and focal necrosis. Bizarre tumor giant cells may be present. In approximately one-third of cases, a heterologous element such as osteosarcoma, chondrosarcoma, or rhabdomyosarcoma is encountered. We diagnose these lesions as “sarcomatoid carcinoma (carcinosarcoma).” The epithelial component consists of acinar adenocarcinoma, small cell carcinoma, ductal adenocarcinoma, and so forth, and the mesenchymal component consists of nonspecific malignant spindle cells, osteosarcoma, chondrosarcoma, and so forth. Although there is no prognostic significance to the various histologic elements present, we note them in the report so that if there are subsequent metastases with one of the elements other than usual prostatic adenocarcinoma, one would be still be able to recognize that the metastasis came from the prostatic sarcomatoid carcinoma based on its report.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


