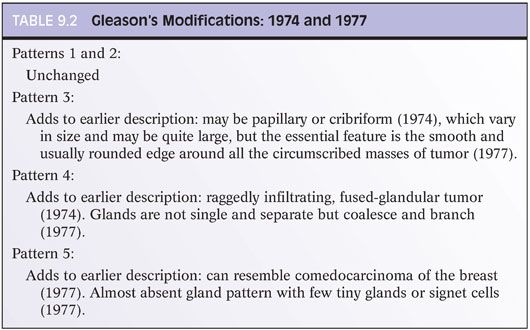
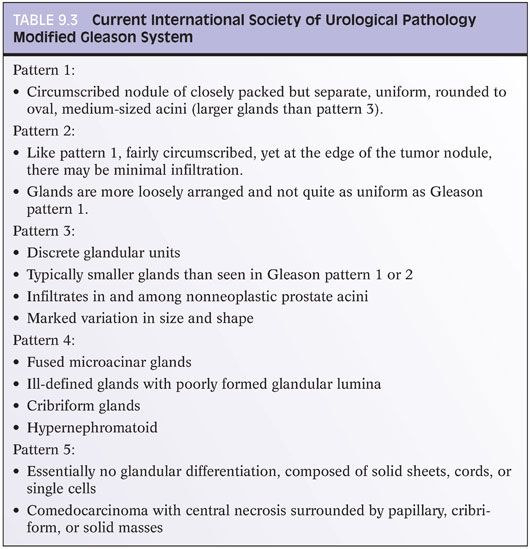
THE 2005 INTERNATIONAL SOCIETY OF UROLOGICAL PATHOLOGY MODIFICATIONS TO THE GLEASON GRADE
Why the Need for a Consensus on Gleason Grading?
Since the late 1960s when the Gleason grading system was derived, the field of prostate carcinoma has changed dramatically. In the 1960s, there was no screening for prostate cancer other than by digital rectal examination, as serum PSA had not yet been discovered. In Gleason’s 1974 study, the vast majority (86%) of men had advanced disease with either local extension out of the prostate on clinical exam or distant metastases. Only 6% of patients had nonpalpable tumor diagnosed by transurethral resection and only 8% of patients were diagnosed with a localized nodule on rectal examination.1 The method of obtaining prostate tissue was also very different from today’s practice. Typically, only a couple of thick-gauge needle biopsies were directed into an area of palpable abnormality. The use of 18-gauge thin biopsy needles and the concept of sextant needle biopsies to more extensively sample the prostate were not developed until the late 1980s.6 Consequently, the grading of prostate cancer in thin cores and in multiple cores from different sites of the prostate were not issues in Gleason’s era.
The Gleason system also predated the use of immunohistochemistry. It is likely that with immunostaining for basal cells that many of Gleason’s original 1 + 1 = 2 adenocarcinomas of the prostate would today be regarded as adenosis (atypical adenomatous hyperplasia), a mimicker of cancer.7 Similarly, many of the cases in 1967 diagnosed as cribriform Gleason pattern 3 carcinoma would probably be currently referred to as cribriform high-grade prostatic intraepithelial neoplasia (PIN) or intraductal carcinoma of the prostate, if labeled with basal cell markers.8,9
Another issue that was not dealt with in the original Gleason grading system is how to grade newly described variants of adenocarcinoma of the prostate. Some of the more common variants where grading issues arise include mucinous carcinoma (see Chapter 13), ductal adenocarcinoma (see Chapter 11), foamy gland carcinoma, and pseudohyperplastic adenocarcinoma of the prostate. In addition, there are certain patterns of adenocarcinoma of the prostate such as those with glomeruloid features and mucinous fibroplasia (collagenous micronodules) where the use of Gleason grading was not defined. The application of the Gleason system for all of the reasons noted earlier varies considerably in contemporary surgical pathology practice compared to Gleason’s era, and there arose a need for a formal updating of the Gleason grading system.
2005 International Society of Urological Pathology Consensus Conference
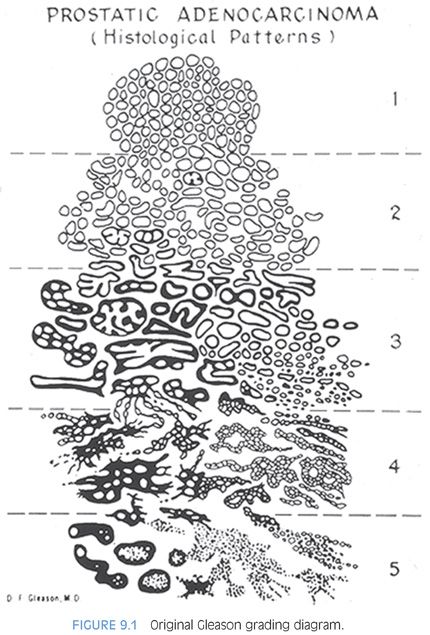
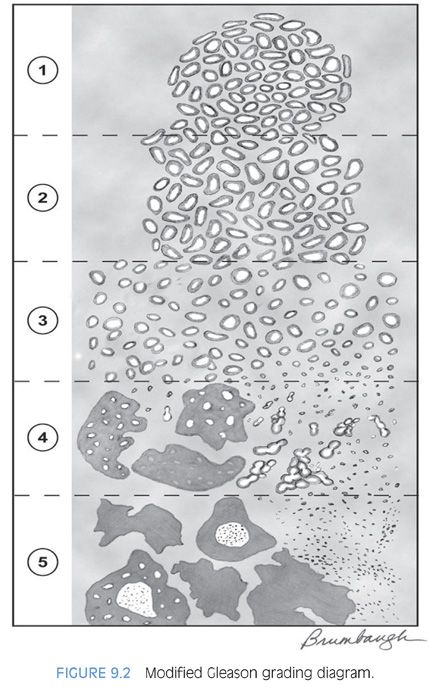
A group of urologic pathologists convened at the 2005 United States and Canadian Academy of Pathology (USCAP) meeting in an attempt to achieve consensus in controversial areas relating to the Gleason grading system.10 Over 70 urologic pathologists from around the world were invited to attend, with most attending. A schematic diagram was developed to reflect the modified Gleason grading system, which was subsequently slightly further modified to reflect changes in grading cribriform cancer (Table 9.3; Fig. 9.2, eFig. 9.1).
It is remarkable that nearly 40 years after the inception of the Gleason grading system, it remains one of the most powerful prognostic predictors in prostate cancer. In part, this system has remained timely by adaptations of the system to accommodate the changing practice of medicine. The Gleason grading consensus conference resulted in a modified updated Gleason grading system that is more relevant to today’s practice.
GENERAL APPLICATIONS OF THE GLEASON GRADING SYSTEM
The initial grading of prostate carcinoma should be performed at low magnification using the 4× and 10× objective.1,10 After one assesses the case at scanning magnification, one may proceed to use the 20× objective to verify the grade. For example, at low magnification, one may have the impression of fused glands or necrosis but may require higher magnification at 20× to confirm its presence. One should not initially use the 20× or 40× objectives to look for rare fused glands or a few individual cells seen only at higher power, which would lead to an overdiagnosis of Gleason pattern 4 or 5, respectively (eFig. 9.7).
The best way to report the Gleason grades in a pathology report is in a mathematical equation (i.e., Gleason score 3 + 3 = 6). Alternative methods in use may be misconstrued. For example, reports of “Gleason 3/5” could be interpreted as either Gleason score 3 + 5 = 8 or the tumor is Gleason pattern 3 out of a maximum of 5 patterns (i.e., Gleason score 3 + 3 = 6). Cases diagnosed as “Gleason grade 4” can be considered as either Gleason score 2 + 2 = 4 or Gleason score 4 + 4 = 8.
GLEASON PATTERNS
Gleason Patterns 1 and 2
Gleason patterns 1 and 2 consist of fairly circumscribed nodules of closely packed glands (eFigs. 9.8 to 9.14). The glands are uniform in their size and shape with slightly more variation in pattern 2 than pattern 1. Smaller glands typical of Gleason pattern 3 are absent. It is now accepted that Gleason score 2 to 4 should not be assigned to cancer on needle biopsy for several reasons including poor reproducibility even among experts. Several studies have demonstrated that tumors on needle biopsy assigned a Gleason score of 2 to 4 are not infrequently associated with higher grade and high-stage disease at radical prostatectomy.11–13 The major limitation of rendering a diagnosis of Gleason score 4 on needle biopsy is that one cannot see the entire edge of the lesion to determine if it is completely circumscribed. Consequently, most of the lesions that appear to be very low-grade on needle biopsies are diagnosed by urologic pathologists as Gleason score 3 + 2 = 5 or 3 + 3 = 6. Studies have shown a dramatic decrease in the incidence of diagnosing Gleason score 2 to 4 on needle biopsy over the last decade. In one study, 24% of pathologists rendered a diagnosis of Gleason score of 2 to 4 on biopsy in 1991, which decreased to 2.4% in 2001.14 In another study analyzing biopsies from 2002 to 2003, only 1.6% were graded as Gleason score 2 to 4 compared to 22.3% of the biopsies in 1994.12,15
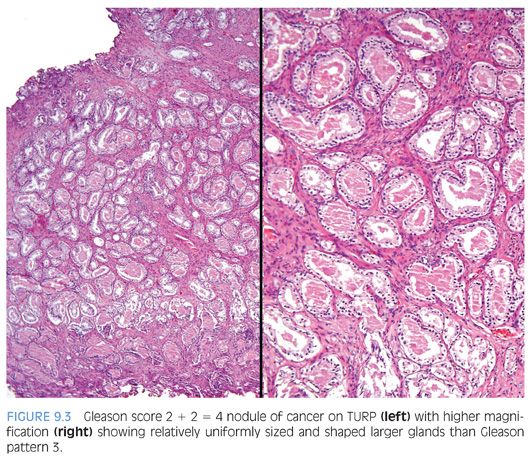
Low-grade cancers are rarely seen on needle biopsy because low-grade cancers are predominantly located anteriorly in the prostate within the transition zone and they tend to be small. Low-grade prostate cancer does exist and Gleason score 3 and 4 adenocarcinomas may be uncommonly diagnosed on transurethral resection of the prostate (TURP) (Fig. 9.3). Typically, both Gleason pattern 1 and Gleason pattern 2 carcinomas have abundant pale eosinophilic cytoplasm. It has been proposed that transition zone cancers be termed clear cell carcinomas.16,17 These tumors do not have a unique histology but rather reflect the finding that transition zone cancers are frequently low grade. Carcinomas with pale cytoplasm may also be found in the peripheral zone.
Gleason Pattern 3
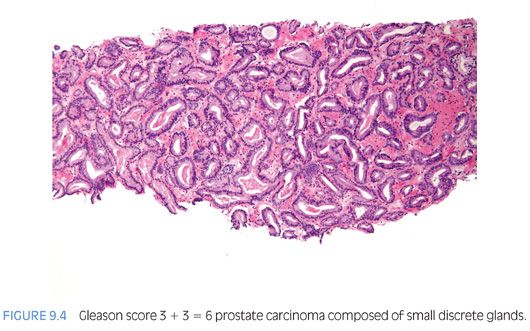
Gleason pattern 3 cancer consists of variably sized individual glands that are well formed (Fig. 9.4, eFigs. 9.15 to 9.27). In contrast to Gleason pattern 4, the glands in Gleason pattern 3 are discrete units. If one can mentally draw a circle around well-formed individual glands, then it is Gleason pattern 3. One should assign a Gleason grade at relatively low power (i.e., 2.5× or 4× objective). The presence of a few poorly formed glands at high power, which could represent a tangential section off of small well-formed glands, is still consistent with Gleason pattern 3 tumor. Gleason pattern 3 glands are either (a) infiltrative between benign glands, (b) more variably sized, or (c) smaller than Gleason patterns 1 and 2.
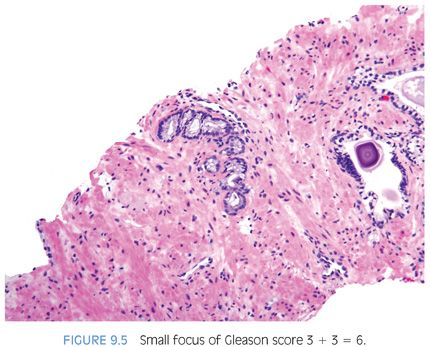
Some pathologists may not feel comfortable assigning both a primary and secondary pattern 3 to very small foci of carcinoma on biopsy. However, small foci of Gleason score 3 + 3 = 6 cancer on biopsy is more often associated with Gleason score 3 + 3 = 6 at radical prostatectomy compared to cases with more extensive Gleason score 3 + 3 = 6 on biopsy (Fig. 9.5).12 The reason is that greater amounts of cancer on needle biopsy correlate with larger tumors that are more likely to have areas of pattern 4 at radical prostatectomy.
A major point of divergence from the original Gleason system is with assignment of grade to cribriform glands. Within Gleason’s18 original illustrations of his cribriform pattern 3, he depicts large, cribriform glands. At the time of the 2005 International Society of Urological Pathology (ISUP) grading consensus meeting, expert uropathologists uniformly had been diagnosing these lesions as cribriform pattern 4 (Figure 3D in 19). The consensus conference proposed extremely stringent criteria for cribriform Gleason pattern 3.10 Subsequently, a study showed that even in a highly selected set of images thought to be the best candidates for cribriform pattern 3, most experts interpreted the cribriform patterns as pattern 4.20 In a subsequent study specifically addressing the prognosis of cribriform prostate cancer glands, both small and large cribriform glands were equally linked to progression after radical prostatectomy.21 These findings fit conceptually, because one would expect the change in grade from pattern 3 to pattern 4 to be reflected in a distinct architectural paradigm shift where cribriform as opposed to individual glands are formed rather than merely a subjective continuum of differences in size, shape, and contour of cribriform glands. The only reason why cribriform pattern 3 even exists is because of the original Gleason schematic diagram. However, Gleason never specifically published the prognostic difference between what he called cribriform Gleason pattern 3 compared to cribriform Gleason pattern 4. Many of Gleason’s cribriform Gleason pattern 3 cancers may not even have been infiltrating carcinomas due to the lack of availability of immunohistochemistry for basal cell markers. Today, we might have diagnosed them either as cribriform high-grade PIN or intraductal carcinoma of the prostate (concepts not present in Gleason’s era).8,9 Based on all the given data, all cribriform cancer should be interpreted as Gleason pattern 4.
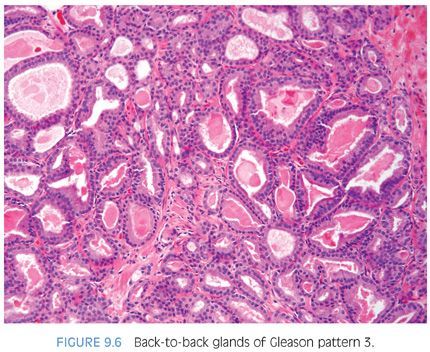
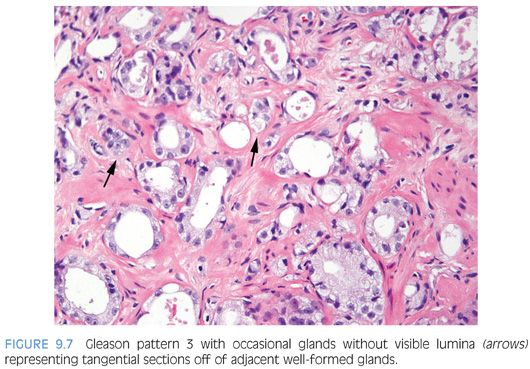
There are certain situations that lead to overgrading of Gleason pattern 3 as pattern 4. Crowded glands at low magnification can have the appearance of fused glands, mimicking Gleason pattern 4 cancer (Fig. 9.6). Small glands are acceptable for Gleason pattern 3 as long as they are well formed and not fused with other glands. Probably, the most common scenario where Gleason pattern 3 is overgraded as Gleason pattern 4 is when a few tangentially sectioned small glands of pattern 3 are present and seen at higher magnification. Given the presence of small glands in Gleason pattern 3, a few glands will invariably be tangentially sectioned, resulting in a gland that appears not well formed (Fig. 9.7). Consequently, only when there is a cluster of poorly formed glands seen at 10× where it is unlikely that they all represent tangentially sectioned glands should Gleason pattern 4 be diagnosed. Branching glands appear more complex than simple round glands, yet as long as they are not fused or cribriform, branching glands are still consistent with Gleason pattern 3. Glands that artifactually appear poorly formed as a result of crush artifact must be distinguished from Gleason pattern 4. Thick, poorly sectioned tissue can result in multilayering and the appearance of poorly formed glands or solid nests of cells, mimicking higher grade carcinoma.
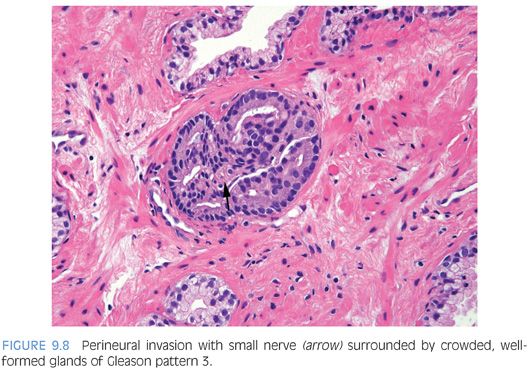
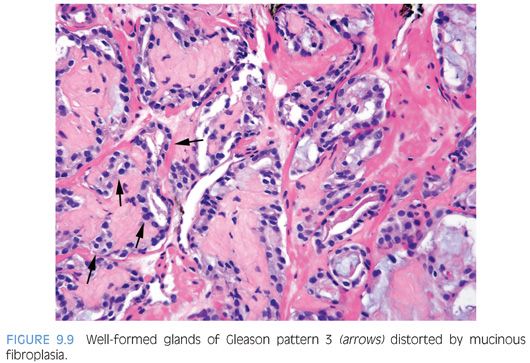
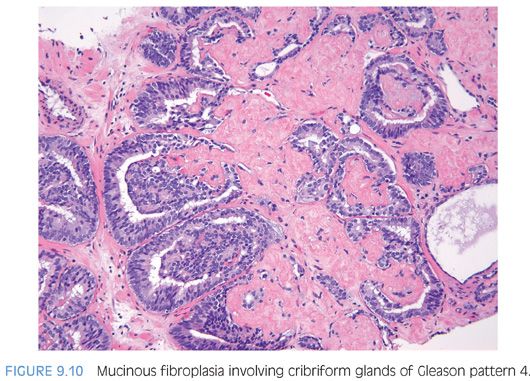
When glands surround a nerve (perineural invasion), the glands often develop a more complex papillary, crowded appearance (Fig. 9.8). Consequently, one should be cautious in diagnosing Gleason pattern 4 based on glands within perineural invasion in the absence of Gleason pattern 4 elsewhere. Similarly, the delicate ingrowth of fibrous tissue seen with mucinous fibroplasia (collagenous micronodules) can result in glands appearing to be fused resembling cribriform structures, although the underlying architecture is really that of individual discrete rounded glands invested by loose collagen. The tumor should be graded on the underlying glandular architecture, whereby the majority are graded as Gleason score 3 + 3 = 6 (Fig. 9.9).22 Only when there are distinct cribriform glands in areas of mucinous fibroplasia should Gleason pattern 4 be diagnosed (Fig. 9.10).
Gleason Pattern 4
The 2005 ISUP consensus conference agreed with the original Gleason system that fused glands, irregular cribriform glands, and the hypernephroma pattern were designated as Gleason pattern 4.10 As described earlier, subsequent studies support the inclusion of any cribriform glands as pattern 4 (eFigs. 9.28 to 9.93). In addition, the consensus conference reported that ill-defined glands with poorly formed glandular lumina also warrant the diagnosis of Gleason pattern 4. In contrast, Gleason’s original description of pattern 4 included only the hypernephromatoid pattern and in subsequent years, fused glandular masses.19,23 Gleason pattern 4 closely resembling renal cell carcinoma (hypernephromatoid pattern) is rare, despite occupying a prominent role in the original Gleason grading system. Cribriform glands in one study were associated with a higher risk of postradical prostatectomy failure as compared to fused glands.21 The current spectrum of morphology in Gleason pattern 4 is depicted schematically in Figure 9.2.
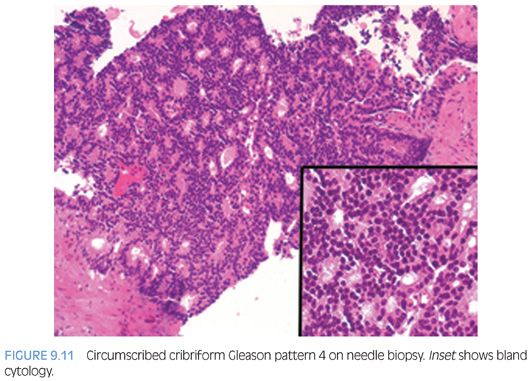
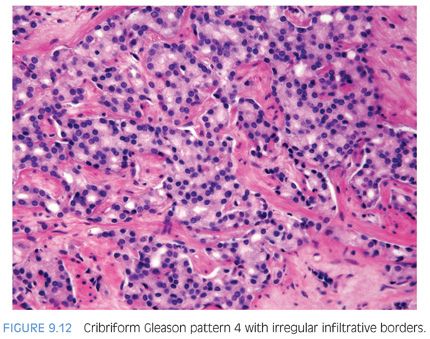
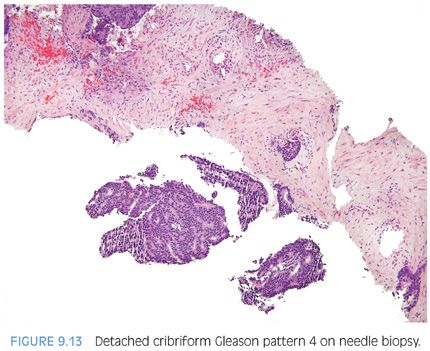
There are some difficulties in distinguishing better developed cribriform glands of pattern 4 from poorly formed cribriform glands with barely identifiable acini that are best characterized as pattern 5 (see Gleason pattern 5 in the following discussion). Despite being high grade based on the architectural pattern, cribriform Gleason pattern 4 can be cytologically bland (Fig. 9.11). Cribriform pattern 4 glands on biopsy can appear rounded irregularly and shaped with ragged borders (Fig. 9.12). On needle biopsy, cribriform Gleason pattern 4 tumor often manifests as fragments of cribriform tumor because there is little supporting stroma in larger cribriform glands (Fig. 9.13).
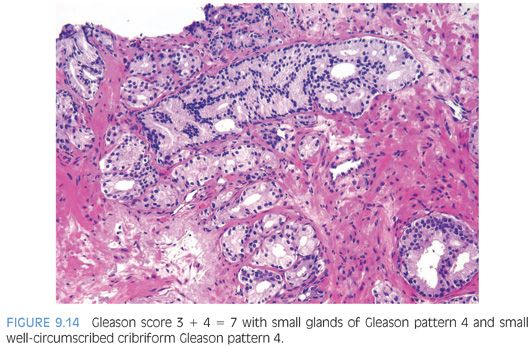
Cribriform prostate cancer glands span a broad spectrum in terms of their differentiation. At one end, there are well-developed cribriform glands with well-formed lumina (Fig. 9.14). In some less differentiated examples, cribriform glands have lumina that are not as open, yet they are still readily recognizable as cribriform structures and hence are still considered Gleason pattern 4 (Fig. 9.15). These cases are better differentiated than some cases of Gleason pattern 5 where the cribriform structures are so poorly developed that they are barely recognizable (see Gleason pattern 5 in the following section).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


