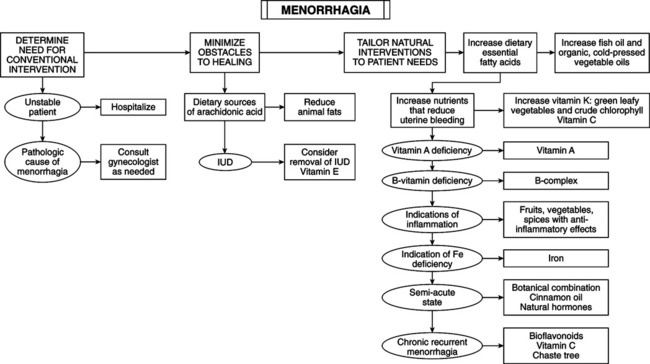
• Excessive menstrual bleeding (blood loss >80 mL) occurring at regular cyclical intervals (cycles are usually, but not necessarily, of normal length). • May be caused by dysfunctional uterine bleeding (no organic cause) or local lesions (e.g., uterine myomas [fibroids], endometrial polyps, endometrial hyperplasia, endometrial cancer, adenomyosis, and endometritis). Other causes include bleeding disorders and hypothyroidism. • Key to diagnosis begins with history and physical examination. Pelvic ultrasound, hysterosonography, hysteroscopy, Pap smear, thyroid function studies, pregnancy test, complete blood count, ferritin, liver function or coagulation studies, follicle-stimulating hormone/luteinizing hormone (LH), serum progesterone, testosterone, dehydroepiandrosterone sulfate, sexually transmitted disease testing, endometrial biopsies or dilation and curettage—used for diagnosis and management as needed. • DUB definition: abnormal uterine bleeding without demonstrable organic cause. DUB includes menorrhagia, oligomenorrhea, polymenorrhea, metrorrhagia, menometrorrhagia, and intermenstrual bleeding. • Abnormal bleeding categories: hormonal, mechanical, and clotting abnormalities. Not all cause menorrhagia, but rather other abnormal bleeding patterns. • Hormonal causes: anovulation and luteal phase defects and stress (DUB), exogenous hormones, hypothyroidism, ovarian cysts. • Mechanical causes: uterine polyps, uterine fibroids, uterine can-cer, intrauterine devices, ectopic pregnancy, pregnancy, endometriosis, endometritis. • Clotting abnormalities: vitamin K deficiency, drug-induced hem-orrhage (heparin, warfarin, aspirin), dysproteinemias, disseminated intravascular coagulation, severe hepatic disease, primary fibrinolysis, circulating inhibitors of coagulation. • Abnormalities in prostaglandin metabolism: menorrhagic endo-metrium excessively incorporates arachidonic acid into neutral lipids and inadequately incorporates it into phospholipids. Increased arachidonic acid release during menses increases production of series 2 prostaglandins—a major factor in excess menstrual bleeding and dysmenorrhea. Excessive bleeding during first 3 days is caused by vasodilation by prostaglandin (PG) E2 and PGI2 and antiaggregating activity of PGI2; pain of dysmenorrhea is caused by excess PGF2alpha. • Thyroid abnormalities: overt hypothyroidism and hyperthyroidism are linked to menstrual disturbances. Minimal, subclinical insufficiency (thyroid stimulation test) may cause menorrhagia and other menstrual disturbances. Minimal hypothyroid patients with menorrhagia may respond dramatically to thyroxine. Consider thyroid-stimulating hormone testing for patients with longstanding menstrual dysfunction (with no obvious uterine pathosis). This is preferred to empirical use of thyroid hormone. • Assessing blood loss by asking for an estimate of number of pads or tampons used during each period and duration of period is inaccurate. Forty percent of women losing >80 mL considered their periods only moderately heavy or scanty; 14% with loss of <20 mL judged their periods to be heavy. • Serum ferritin is best indicator of blood loss but may be impractical for immediate information. Attempt to understand blood loss. Be concerned about excess bleeding >7 straight days, more frequently than every 21 days, new pad or tampon every hour for more than half a day. Changing pad or tampon every half hour or less requires urgent attention; it may be an emergency. Any bleeding in postmenopausal women is abnormal. Pathologic Causes of Menorrhagia • Abnormalities of prostaglandin metabolism: menorrhagic endometrium incorporates arachidonic acid (AA) into neutral lipids to much greater extent than normal while incorporation into phospholipids is decreased; increased AA release during menses increases production of series 2 prostaglandins, a major factor in excess bleeding and dysmenorrhea; excess bleeding during first 3 days from the vasodilatory properties of PGE2 and PGI2 and antiaggregating activity of PGI2; pain of dysmenorrhea is due to overproducing PGF2a. • Other contributing factors: iron deficiency, hypothyroidism, vitamin A deficiency, intrauterine devices, local factors (uterine myomas, endometrial polyps, adenomyosis, endometrial hyperplasia, salpingitis, endometritis).
Menorrhagia
DIAGNOSTIC SUMMARY
GENERAL CONSIDERATIONS
Etiology
Estimating Menstrual Blood Loss
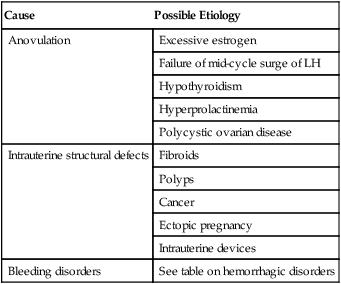
Cause
Possible Etiology
Anovulation
Excessive estrogen
Failure of mid-cycle surge of LH
Hypothyroidism
Hyperprolactinemia
Polycystic ovarian disease
Intrauterine structural defects
Fibroids
Polyps
Cancer
Ectopic pregnancy
Intrauterine devices
Bleeding disorders
See table on hemorrhagic disorders
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


