Medullary Carcinoma
Key Facts
Terminology
Medullary carcinoma (MC)
Rare subtype of invasive breast cancer with characteristic histologic features
Etiology/Pathogenesis
Many MCs downregulate BRCA1 either by promoter methylation (2/3) or mutation (1/4)
MC is member of basal-like group of breast carcinomas by gene expression profiling
Typically negative for ER, PRP, and HER2
Majority have TP53 mutations
Clinical Issues
MC, when strictly defined by morphologic criteria, has favorable prognosis
Actuarial 10-year survival rates greater than 80% in some reports
Usually presents as palpable, often rapidly growing mass
Improved survival may be due to host immune response, syncytial growth pattern, &/or high mitotic rate leading to increased sensitivity to therapy
Top Differential Diagnoses
Atypical medullary carcinoma (AMC)
Carcinomas arising in women with BRCA1 mutations
13% have MC and 30-60% have carcinomas with medullary features
Intramammary nodal metastasis
Lymphoma
TERMINOLOGY
Abbreviations
Medullary carcinoma (MC)
Definitions
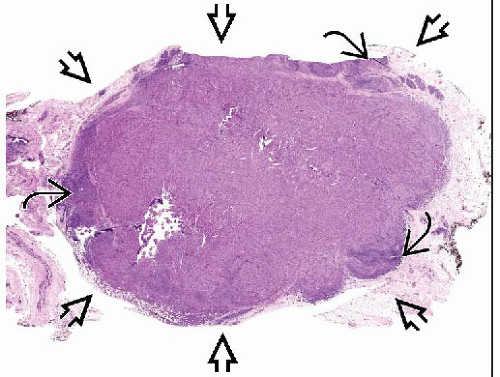
Rare histologic subtype of invasive breast cancer with characteristic histologic features
“Medullary” was applied to these carcinomas in 19th century based on their gross appearance
“Medullary” refers to marrow of bones, signifying soft mass
“Encephaloid” (resembling brain) was alternative term
Lack of desmoplastic stroma resulting in soft consistency distinguishes MC from other carcinomas that are hard or scirrhous
ETIOLOGY/PATHOGENESIS
Molecular Pathology of MC
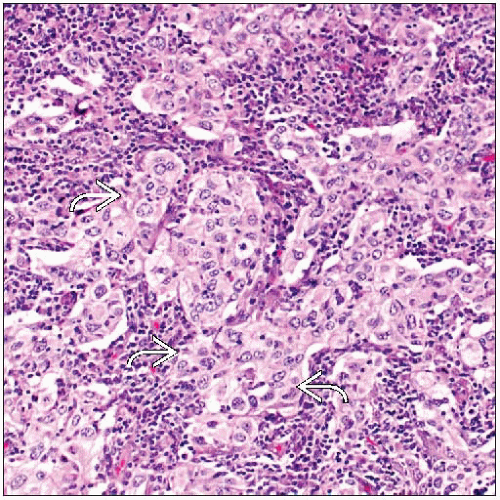
Syncytial growth pattern is critical for diagnosis and is linked to prognosis
MC has increased expression of cell adhesion proteins including E-cadherin and β-catenin
Tight cell adhesion may limit tumor cell dissemination via lymphatics correlating with fewer nodal and distant metastases
Many MC downregulate BRCA1
Approximately 25% of apparent sporadic MC have BRCA1 mutations
Approximately 2/3 of MCs without BRCA1 mutations have downregulation due to promoter methylation
In turn, MC accounts for 13% of breast tumors arising in BRCA1 mutation carriers
30-60% of carcinomas in BRCA1 mutation carriers have medullary features
Medullary features rare in women with BRCA2 mutations
Gene expression profiling
MC is member of basal-like group of breast carcinomas
MC has higher level of expression of CK5/6 and higher rates of gains and losses of DNA as compared to other basal-like carcinomas
Most basal-like carcinomas have poor prognosis
MC is exception as it has more favorable prognosis compared to carcinomas of no special type when strict diagnostic criteria are applied
CLINICAL ISSUES
Epidemiology
Incidence
MC represents 1-7% of all invasive breast cancers
Differences in incidence likely related to stringency of criteria used to make diagnosis
Age
Average age at presentation: 45-52 years
Compared with 55 years for patients with IDC, not otherwise specified
Presentation
Most patients present with palpable mass
May be soft and mobile and perceived as benign
Often grows rapidly
Lymphadenopathy may be present
Lymph nodes may be enlarged due to hyperplasia; metastases are uncommon
Treatment
Adjuvant therapy
Some medical oncologists take more conservative approach for MC due to favorable prognosis
However, favorable prognosis may not apply to large cancers or cancer in women with BRCA1 mutations
Therefore, strict criteria should be used for diagnosis to avoid undertreating patients with poorly differentiated carcinoma of no special type
Prognosis
MC, when strictly defined by morphologic criteria, has relatively favorable prognosis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree