• Auras: migraines can come without warning but often have symptoms (auras) a few minutes before onset of pain: blurring or bright spots of vision, anxiety, fatigue, disturbed thinking, unilateral peripheral numbness or tingling. • Migraine headaches are caused by excessive dilation of blood vessels in the head; they affect 15%-20% of men and 25%-30% of women. • Vascular headache pain (e.g., migraine): throbbing or pounding sharp pain; nonvascular headache (tension headache) pain: steady, constant, dull pain starting at base of skull or in forehead and spreading over entire head, giving sensation of pressure or vise grip applied to skull. Pain of headache comes from outside the brain because brain tissue is insensate. Pain arises from meninges and scalp, large cranial vessels, proximal intracranial vessels, and scalp vasculature and muscles when stretched or tensed. • Most common nonvascular headache is the tension headache, caused by tightened muscles of the face, neck, or scalp, resulting from stress or poor posture. Tightened muscles pinch nerves or their blood supply, causing pain and pressure. Relaxation of muscle usually brings immediate relief. • Cluster headache was once considered migraine-type because vasodilation is a key component. It is now separately classified. It is also called histamine cephalgia, Horton’s headache, or atypical facial neuralgia. It is much less common than migraine. • Chronic daily headache (CDH) (also called chronic tension headache, migraine with interparoxysmal headache, transformed migraine, evolutive migraine, mixed headache syndrome, tension-vascular HA): affects 40% of patients in headache clinics. • Vasomotor instability theory: superficial temporal vessels are visibly dilated. Local compression of these vessels or carotid artery temporarily relieves pain. Other types of extracranial vasodilation (heat or exercise induced) are not problematic. Patients are pale during headache despite extracranial vasodilation, and lower skin temperature of the affected side suggests constriction of small vessels. Focal or diffuse cerebral or brainstem dysfunction is attributed to intracranial vasoconstriction. Blood flow is greatly reduced during the prodromal stage, followed by a stage of increased blood flow persisting for >48 hours. Aura may be caused by cortical spreading depression, a process producing transient depression of spontaneous and evoked neuronal activity. During this time, the brain fails to maintain normal ionic homeostasis and efflux of excitatory amino acids from neurons. Cortical spreading depression may be linked to decreased cerebral blood flow during aura. This stage may be followed by phase of increased blood flow that can persist for >48 hours. Migraine patients may have functional abnormality of vasomotor control, suggested by orthostatic symptoms and abnormal sensitivity to vasodilatory effects of physical and chemical agents. Migraineurs experience heightened central nervous system activity, which appears to be mediated by the trigeminovascular system. • Platelet disorder theory: migraine platelets show increased spontaneous aggregation, aberrant manner of serotonin release, and aberrant platelet composition. Hanington theory: most common precipitant of migraine is emotional stressor causing increased plasma catecholamine, triggering serotonin release, platelet aggregation, and vasoconstriction. Migraineurs’ platelets aggregate more readily than normal, both spontaneously and when exposed to serotonin, adenosine diphosphate (ADP), and catecholamines, similar to transient cerebral ischemic attacks (TIA). TIA symptoms resemble prodromal phase of migraine headache. Attack onset is accompanied by elevated plasma serotonin, followed by increased urinary 5-hydroxyindoleacetic acid (5-HIAA), a breakdown product of serotonin metabolism. Blood serotonin is normally stored in platelets and released by aggregation and in response to stimuli (catecholamines). Total serotonin content in normal and migraine platelets is identical. Quantity of serotonin released by migraine platelets, in response to serotonin stimulation, is normal (or subnormal) after attack but progressively higher as next attack approaches. Plasma serotonin elevation may not be causative; it may be self-defense mechanism or epiphenomenon produced by neurogenic inflammation. Yet platelet deactivating agents (aspirin, feverfew, essential fatty acids) help prevent migraines. Platelet hypothesis evidence: classic migraine patients have twofold increase in incidence of mitral valve prolapse. Prolapsing mitral valve damages platelets and increases aggregation and possibly release of serotonin and other vasoactive substances. • Neuronal disorder theory: trigeminovascular neurons, which innervate pial arteries, release peptide substance P either in direct response to initiators or secondarily to changes in the central nervous system. Substance P is a mediator of pain released into arteries, linked to vasodilation, mast cell degranulation, and increased vascular permeability. Arterial endothelial cells may respond to substance P by releasing vasoactive substances; functional changes within the noradrenergic system may be the threshold for migraine activation. Potentiators may exert effects by modulating sympathetic activity. Chronic stress is a potentiator in this model. • Migraine as a “serotonin deficiency” syndrome: 5-HIAA increases in urine during migraine arising from increased breakdown of serotonin from increased activity of monoamine oxidase. Migraine sufferers have low tissue serotonin (low serotonin syndrome). Low serotonin may cause decreased pain threshold. Positive clinical results are seen with serotonin precursor 5-hydroxytryptophan (5-HTP) (Textbook, “5-Hydroxytryptophan”). Link between low serotonin and headache is the basis of many migraine prescription drugs. Monoamine oxidase inhibitors (which increase serotonin) prevent headaches. Increasing serotonin relieves chronic migraines. Effects of 5-HTP and drugs on the serotonin system are complex because of the multiple types of serotonin receptors. Binding to 5-HT1c receptors triggers mi-graines; inhibiting 5-HT1c prevents migraines. Binding receptor 5-HT1d may prevent and stop migraines. 5-HT1c receptors are desensitized, that is, they lose affinity for serotonin, by increasing serotonin exposure by using 5-HTP. Serotonin binds instead to 5-HT1d receptor, decreasing headaches. Evidence for theory: 5-HTP is more effective over time (after 60 days of use rather than after 30). Antimigraine triptan drugs are 5-HT1b and 5-HT1d receptor agonists that constrict blood vessels, and block neurogenic inflammation and neural peptide release. They may also inhibit neuronal activity within the trigeminovascular system. Safety issue: triptans activate serotonin receptors on cerebral vessels and coronary arteries; avoid in patients with ischemic heart disease, uncontrolled hypertension, or cerebrovascular disease. Avoid using triptans, ergotamine-based drugs, and selective serotonin reuptake inhibitors (SSRIs) concurrently, although risk of serotonin syndrome is low. Some practitioners use 5-HTP successfully with SSRIs, but caution is advised. Although SSRIs are used for migraine prophylaxis, their biochemical effect is unknown, quality of evidence is poor, and clinical impact is low. • Unified hypothesis: migraine has a three-stage process: initiation, prodrome, and headache. Initiation depends on accumulation over time of several stressors that ultimately affect serotonin metabolism. At a critical point of susceptibility (or threshold), a cascade event is initiated. Susceptibility is a combination of decreased tissue serotonin, platelet changes, altered responsiveness of key cerebrovascular end organs, increased sensitivity of intrinsic noradrenergic system of the brain, and buildup of histamine, arachidonic acid metabolites, or other mediators of inflammation. Platelet changes: increased adhesiveness, enhanced tendency to release serotonin, and increased membrane arachidonic acid. When platelets are stimulated to secrete serotonin, platelet aggregation, vasospasm, and inflammatory processes cause local cerebral ischemia. This is followed by rebound vasodilation and release of peptide substance P and other mediators of pain. • Symptoms of chronic poisoning result from blood vessel contraction and reduced circulation (numbness and coldness of extremities, tingling, chest pain, heart valve lesions, hair loss, decreased urination, and gangrene of fingers and toes) and those resulting from nervous system disturbances (vomiting, diarrhea, headache, tremors, contractions of facial muscles, and convulsions). • Regular ergotamine use in migraine is linked to dependency syndrome—severe chronic headache with increased intensity—on ceasing medicine. Most migraines rarely occur more than once or twice a week; presence of daily migraine-type head-ache in persons taking ergotamine is a good clue for ERHA. Dosage can be a clue: weekly dosages >10 mg (some patients take 10-15 mg q.d.). • Stopping ergotamine causes predictable, protracted, debilitating headache with nausea and vomiting within 72 hours and may last another 72 hours. Improvement after cessation is common. Ginger may lessen ergotamine withdrawal symptoms. • Idiopathic response to a pharmacologically active substance, such as tyramine • Monoamine oxidase deficiency • Platelet phenolsulfotransferase deficiency; immunologically me-diated food allergy • Red wine is more problematic than white wine because it has 20-200 times the amount of histamine, and it stimulates release of vasoactive compounds by platelets. Being much higher in flavonoids, it inhibits enzyme (phenolsulfotransferase), which breaks down serotonin and other vasoactive amines in platelets. Migraine sufferers have much lower levels of this enzyme. High vasoactive amine foods (cheese, chocolate) worsen the problem. • Standard treatment of histamine-induced headache is a histamine-free diet plus vitamin B6. • Enzyme diamine oxidase, which breaks down histamine in small intestine mucosa before absorption into circulation, influences whether a person reacts to dietary histamine. Persons sensitive to dietary histamine have less of this enzyme than control subjects. Diamine oxidase is vitamin B6 dependent. Compounds inhibiting B6 (that also inhibit diamine oxidase): food color-ing agents (hydrazine dyes: FD&C yellow #5), drugs (iso-niazid, hydralazine, dopamine, penicillamine), birth control pills, alcohol, and excessive protein intake. Yellow dye #5 (tartrazine) is consumed in greater quantities (15 mg q.d.) than the recommended daily allowance for vitamin B6 (2.0 mg for males and 1.6 mg for females). • Vitamin B 6 (1 mg/kg body weight) improves histamine tolerance, presumably by increasing diamine oxidase activity. Women have lower diamine oxidase. This may explain the higher incidence of histamine-induced headaches among women. Women are more frequently intolerant of red wine. Level of diamine oxidase in women increases by more than 500 times during pregnancy; women with histamine-induced headaches commonly have complete remission during pregnancy. • Diet-related triggers: hypoglycemia can trigger migraine and is correctable by dietary manipulation. Hypoglycemia may arise from refined carbohydrate intake, especially when insulin becomes elevated. Excessive sodium intake may increase antiotensin in response to sodium ingestion. For lactose intolerance, avoiding dairy may afford improvement. Aspartame, a common sweetener, may increase migraine incidence. • Dysbiosis and detoxification: migraine is not just food intolerance; digestive and detoxification aberrations complicate matters. Metabolic waste of pathogenic organisms may produce headache. Correct intestinal dysbiosis is identified clinically or by stool culture, organic acids analysis, or intestinal permeability assessment. Helicobacter pylori was detected in 40% of migraine patients; eradication of the bacterium improved headache intensity, duration, and frequency in 100% of patients treated. Toxic overload or suboptimal function of detoxification enzymes may trigger headache. Susceptibility to toxicity is produced by excessive environmental exposures, genetic polymorphisms in detoxification enzyme production, and depletion of nutrient cofactors catalyzing phase I and/or phase II detoxification reactions.
Magraine Headache
DIAGNOSTIC SUMMARY
GENERAL CONSIDERATIONS
Classification and Diagnosis
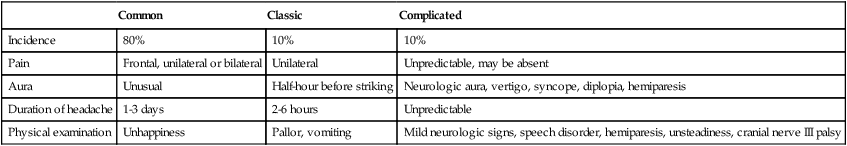
Common
Classic
Complicated
Incidence
80%
10%
10%
Pain
Frontal, unilateral or bilateral
Unilateral
Unpredictable, may be absent
Aura
Unusual
Half-hour before striking
Neurologic aura, vertigo, syncope, diplopia, hemiparesis
Duration of headache
1-3 days
2-6 hours
Unpredictable
Physical examination
Unhappiness
Pallor, vomiting
Mild neurologic signs, speech disorder, hemiparesis, unsteadiness, cranial nerve III palsy
Pathophysiology
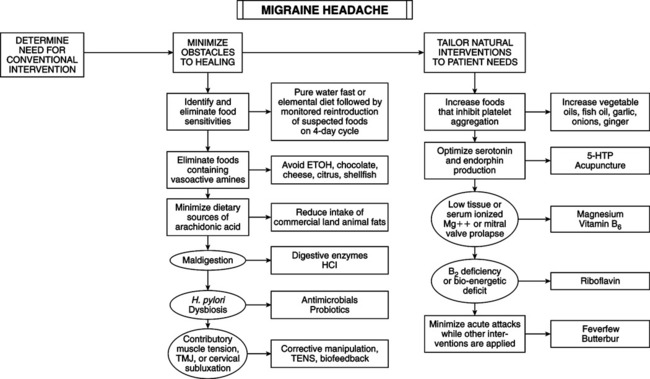
THERAPEUTIC CONSIDERATIONS
Drug Reaction
Diet
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Magraine Headache
