Lymphomatoid Granulomatosis
Aaron Auerbach, MD, PhD
Key Facts
Terminology
Extranodal angiocentric mature B-cell lymphoma that expresses Epstein-Barr virus (EBV) antigens
Etiology/Pathogenesis
Associated with immunodeficiency, ↑ involvement with allogeneic organ transplant, human immunodeficiency virus infection, X-linked lymphoproliferative disorder, and Wiskott-Aldrich syndrome
Clinical Issues
Most common site is lung (usually multiple nodules); skin is most common extrapulmonary site
Cases with larger number of atypical B cells expressing EBV have worse prognosis
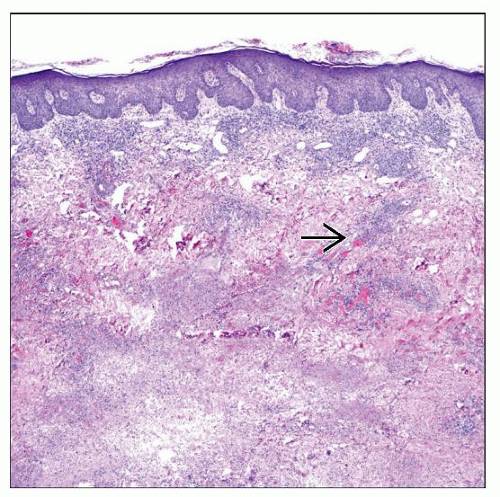
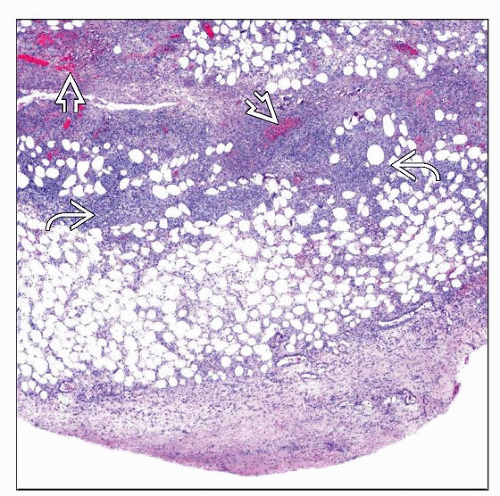
Microscopic Pathology
B cells in subcutis and sometimes dermis are scattered and often do not form sheets; B cells may be immunoblasts, multinucleated, and Reed-Sternberg cell-like
Tumor cells angiocentric, angiodestructive with lymphocytic vasculitis and fibrinoid necrosis of injured blood vessels
Ancillary Tests
CD20(+), pax-5(+), EBV(+) (less in skin than lung), CD30(+/−), CD15(−)
Clonal Ig heavy chain (IgH) gene rearrangement more often in higher grades lesions
Mixed population of T cells, but most express CD4
TERMINOLOGY
Abbreviations
Lymphomatoid granulomatosis (LYG)
Synonyms
Angiocentric immunoproliferative lesion, angiocentric lymphoma
Definitions
Extranodal angiocentric mature B-cell lymphoma that expresses Epstein-Barr virus (EBV) antigens
ETIOLOGY/PATHOGENESIS
Immunodeficiency
Associated with immunodeficiency, ↑ involvement with allogeneic organ transplant, human immunodeficiency virus infection, X-linked lymphoproliferative disorder, and Wiskott-Aldrich syndrome
Cytokines
IP10 and Mig are implicated in pathogenesis of blood vessel damage
CLINICAL ISSUES
Epidemiology
Age
Mostly adults, commonly in 50s, also in children with immunodeficiency syndromes
Gender
M:F > 2.0:1.0
Site
Most common site is lung (usually multiple nodules); skin is most frequent extrapulmonary site
For skin lesions, often trunk or limbs, cutaneous nodules often develop after pulmonary disease
Also involve kidney, liver, and brain; usually not found in lymph nodes or spleen
Presentation
Variable cutaneous lesions can be papules or nodules, often multiple and sometimes with ulceration; plaques are less common
Pulmonary symptoms (cough and dyspnea)
Prognosis
Variable, but often related to grading
Most patients have aggressive disease, survival < 2 years
Cases with increased numbers of small lymphocytes and histiocytes have more favorable prognosis
Cases with larger number of atypical B cells expressing EBV have worse prognosis
Grading based on number of EBV(+) B cells compared to background reactive T cells
Grade 1: < 5 EBER(+) cells per high-power field, large atypical B cells are rare, polymorphous background infiltrate, focal or no necrosis
Grade 2: 5-20 EBER(+) cells per high-power field, small clusters of B cells, more necrosis
Grade 3: > 20 EBER(+) cells per high-power field, large atypical B cells, larger B-cell aggregates, often Reed-Sternberg-like cells, more necrosis
Grade 3 lesions show some response to aggressive chemotherapy + rituximab
MICROSCOPIC PATHOLOGY
Histologic Features
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree