http://evolve.elsevier.com/McCuistion/pharmacology/
Chronic obstructive pulmonary disease (COPD) and restrictive pulmonary disease are the two major categories of lower respiratory tract disorders. COPD is caused by airway obstruction with increased airway resistance of airflow to lung tissues. Four major pulmonary disorders cause COPD: (1) chronic bronchitis, (2) bronchiectasis, (3) emphysema, and (4) asthma. Chronic bronchitis, bronchiectasis, and emphysema frequently result in irreversible lung tissue damage. The lung tissue changes that result from an acute asthmatic attack are normally reversible; however, if the attacks are frequent and asthma becomes chronic, irreversible changes in the lung tissue may result. Patients with COPD usually have a decrease in forced expiratory volume in 1 second (FEV1) as measured by pulmonary function tests.
Restrictive lung disease is a decrease in total lung capacity as a result of fluid accumulation or loss of elasticity of the lung. Pulmonary edema, pulmonary fibrosis, pneumonitis, lung tumors, thoracic deformities (scoliosis), and disorders that affect the thoracic muscular wall, such as myasthenia gravis, are among the types and causes of restrictive pulmonary disease.
Drugs discussed in this chapter are primarily used to treat COPD, particularly asthma. These drugs include bronchodilators (sympathomimetics [primarily beta2-adrenergic agonists], methylxanthines [xanthines]), leukotriene antagonists, glucocorticoids, cromolyn, anticholinergics, and mucolytics. Some of these drugs may also be used to treat restrictive pulmonary diseases.
Chronic Obstructive Pulmonary Disease
Asthma is an inflammatory disorder of the airway walls associated with a varying amount of airway obstruction. This disorder is triggered by stimuli such as stress, allergens, and pollutants. When activated by stimuli, the bronchial airways become inflamed and edematous, leading to constriction of air passages. Inflammation aggravates airway hyperresponsiveness to stimuli, causing bronchial cells to produce more mucus, which obstructs air passages. This obstruction contributes to wheezing, coughing, dyspnea (breathlessness), and tightness in the chest, particularly at night or in the early morning.
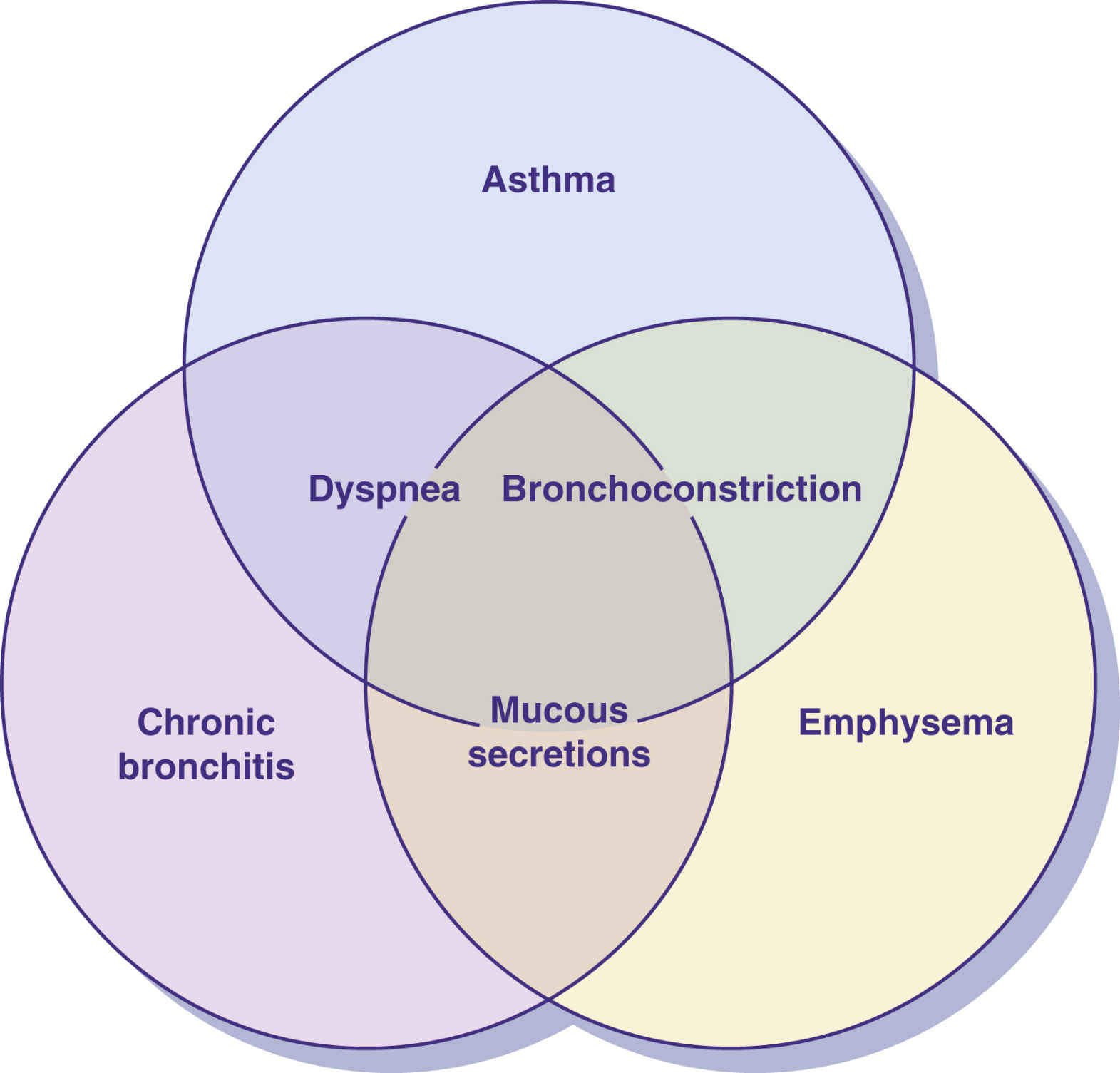
Bronchial asthma, one of the COPD lung diseases, is characterized by bronchospasm (constricted bronchioles), wheezing, mucous secretions, and dyspnea. There is resistance to airflow caused by obstruction of the airway. In acute and chronic asthma, minimal to no changes are seen in the structure and function of lung tissues when the disease process is in remission. In chronic bronchitis, emphysema, and bronchiectasis, irreversible damage is done to the physical structure of lung tissue. Symptoms are similar to those of asthma in these three pulmonary disorders, except wheezing does not occur. Fig. 36.1 shows the overlapping symptoms of COPD conditions. Frequently, a steady deterioration occurs over a period of years.
Chronic bronchitis is a progressive lung disease caused by smoking or chronic lung infections. Bronchial inflammation and excessive mucous secretion result in airway obstruction. Productive coughing is a response to excess mucous production and chronic bronchial irritation. Inspiratory and expiratory rhonchi may be heard on auscultation. Hypercapnia (increased carbon dioxide retention) and hypoxemia (decreased blood oxygen) lead to respiratory acidosis.
In bronchiectasis, dilation of the bronchi and bronchioles is abnormal secondary to frequent infection and inflammation. The bronchioles become obstructed by the breakdown of the epithelium of the bronchial mucosa, and tissue fibrosis may result.
Emphysema is a progressive lung disease caused by cigarette smoking, atmospheric contaminants, or lack of the alpha1-antitrypsin protein that inhibits proteolytic enzymes that destroy alveoli (air sacs). Proteolytic enzymes are released in the lung by bacteria or phagocytic cells. The terminal bronchioles become plugged with mucus, causing a loss in the fiber and elastin network in the alveoli. Alveoli enlarge as many of the alveolar walls are destroyed. Air becomes trapped in the overexpanded alveoli, leading to inadequate gas exchange (oxygen and carbon dioxide).
Cigarette smoking is the most common risk factor for COPD, especially with chronic bronchitis and emphysema. There is no known cure for COPD at this time; however, it remains preventable in most cases. Because cigarette smoking is the most directly related cause, not smoking significantly prevents COPD from developing. Quitting smoking will slow the disease process.
Medications frequently prescribed for COPD include the following:
• Bronchodilators such as sympathomimetics (adrenergics), parasympatholytics (anticholinergic drugs, ipratropium bromide), and methylxanthines (caffeine, theophylline) are used to assist in opening narrowed airways.
• Glucocorticoids (steroids) are used to decrease inflammation.
• Leukotriene modifiers reduce inflammation in the lung tissue, and cromolyn acts as an antiinflammatory agent by suppressing the release of histamine and other mediators from the mast cells.
• Expectorants are used to assist in loosening mucus from the airways.
• Antibiotics may be prescribed to prevent serious complications from bacterial infections.
Bronchial Asthma
Bronchial asthma is a COPD characterized by periods of bronchospasm resulting in wheezing and difficulty breathing. Bronchospasm, or bronchoconstriction, results when the lung tissue is exposed to extrinsic or intrinsic factors that stimulate a bronchoconstrictive response. Factors that can trigger an asthmatic attack (bronchospasm) include humidity; air pressure changes; temperature changes; smoke; fumes (exhaust, perfume); stress; emotional upset; exercise; and allergies to animal dander, dust mites, food, and drugs (e.g., aspirin, ibuprofen, beta-adrenergic blockers). Reactive airway disease (RAD) is a cause of asthma that results from sensitivity stimulation from allergens, dust, temperature changes, and cigarette smoking.
Pathophysiology
Mast cells found in connective tissue throughout the body are directly involved in the asthmatic response, particularly to extrinsic factors. Allergens attach themselves to mast cells and basophils, resulting in an antigen-antibody reaction on the mast cells in the lung; thus the mast cells stimulate the release of chemical mediators such as histamines, cytokines, serotonin, eosinophil chemotactic factor of anaphylaxis (ECF-A), and leukotrienes. Eosinophil counts are usually elevated during an allergic reaction, which indicates that an inflammatory process is occurring. These chemical mediators stimulate bronchial constriction, mucous secretions, inflammation, and pulmonary congestion. Histamine and ECF-A are strong bronchoconstrictors. Bronchial smooth muscles are wrapped spirally around the bronchioles and contract as they are stimulated by these mediators. Exposure to an allergen results in bronchial hyperresponsiveness, epithelial shedding of the bronchial wall, mucous gland hyperplasia and hypersecretion, leakage of plasma that leads to swelling, and bronchoconstriction.
Fig. 36.2 shows factors that contribute to bronchoconstriction. Cyclic adenosine monophosphate (cyclic AMP, or cAMP), a cellular signaling molecule, is involved in many cellular activities and is responsible for maintaining bronchodilation. When histamine, ECF-A, and leukotrienes inhibit the action of cAMP, bronchoconstriction results. The sympathomimetic (adrenergic) bronchodilators and methylxanthines increase the amount of cAMP in bronchial tissue cells.
In an acute asthmatic attack, the short-acting sympathomimetics (beta2-adrenergic agonists) are the first line of defense. They promote cAMP production and enhance bronchodilation. Long-acting sympathomimetics are used for maintenance. Sympathomimetics (adrenergics) are also discussed in Chapter 15.
Sympathomimetics: Alpha- and Beta2-Adrenergic Agonists
Sympathomimetics increase cAMP, causing dilation of the bronchioles. In an acute bronchospasm caused by anaphylaxis from an allergic reaction, the nonselective sympathomimetic epinephrine—an alpha1, beta1, and beta2 agonist—is given subcutaneously to promote bronchodilation and elevate blood pressure. Epinephrine is administered in emergency situations to restore circulation and increase airway patency (see Chapter 55).
For bronchospasm associated with chronic asthma or COPD, selective beta2-adrenergic agonists are given by aerosol or as a tablet. These drugs act primarily on the beta2 receptors, therefore side effects are less severe than those of epinephrine, which acts on alpha1, beta1, and beta2 receptors.
Albuterol
The newer beta-adrenergic drugs for asthma are more selective for beta2 receptors. High doses or overuse of the beta2-adrenergic agents for asthma may cause some degree of beta1 response, such as nervousness, tremor, and increased pulse rate. The ideal beta2 agonist is one that has a rapid onset of action, longer duration of action, and few side effects. Albuterol is a selective beta2 drug that is effective for treatment and control of asthma by causing bronchodilation with a long duration of action. (See Prototype Drug Chart 15.2 for drug data related to albuterol.)
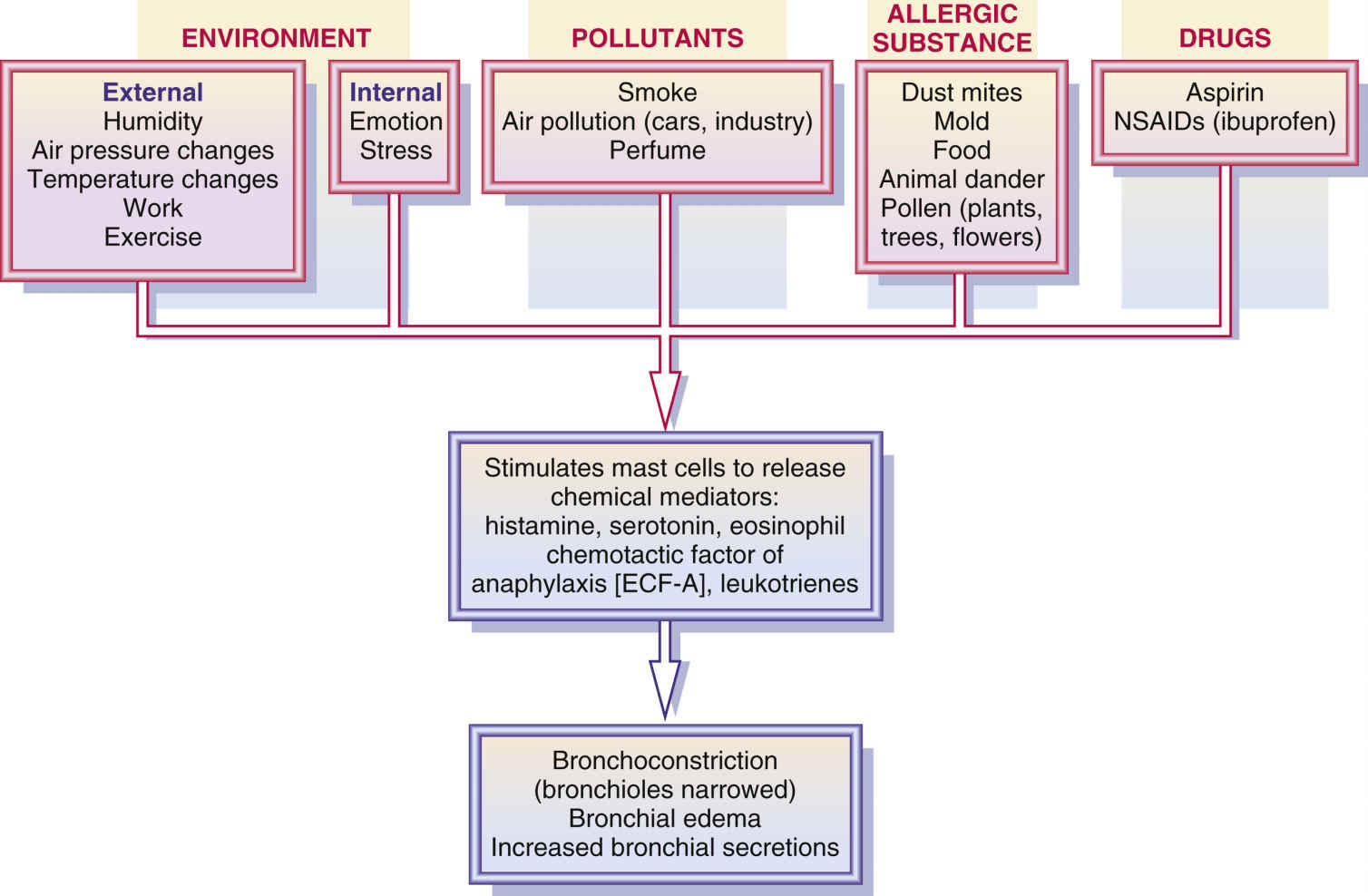
FIG. 36.2 Factors that contribute to bronchoconstriction. NSAIDs, nonsteroidal antiinflammatory drugs.
Metaproterenol
The beta-adrenergic agent metaproterenol has some beta1 effect but is primarily used as a beta2 agent. It can be administered orally or by inhalation with a metered-dose inhaler (MDI) or a nebulizer.
For long-term asthma treatment, beta2-adrenergic agonists are frequently administered by inhalation. This route of administration usually delivers more of the drug directly to the constricted bronchial site. The effective inhalation drug dose is less than it would be by the oral route, and there are also fewer side effects using this route. The onset of action is 1 minute by oral inhalation, 5 to 30 minutes by nebulization, and 15 to 30 minutes when taken orally. The peak for inhalation and oral administration is 1 hour with a duration of 4 hours.
Use of an Aerosol Inhaler
If the beta2 agonist is given by MDI or dry-powder inhaler (DPI), correct use of the inhaler and dosage intervals need to be explained to the patient. If the patient does not receive effective relief from the inhaler, either the technique is faulty or the canister is empty. A spacer device may be attached to the inhaler to improve drug delivery to the lung with less deposition in the mouth. If the patient does not use the inhaler properly to deliver the drug dose, the medication may be trapped in the upper airways. Because of drug inhalation, mouth dryness and throat irritation could result.
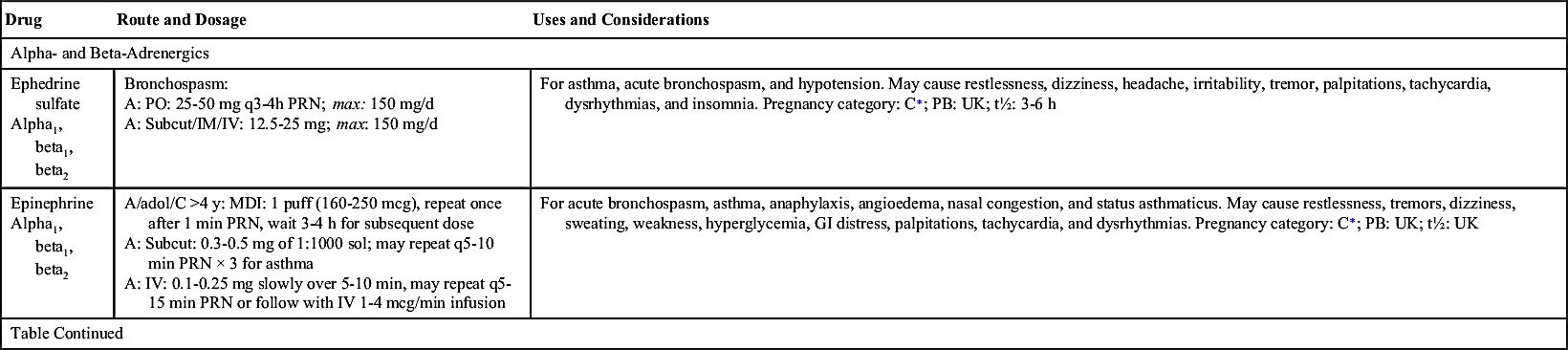
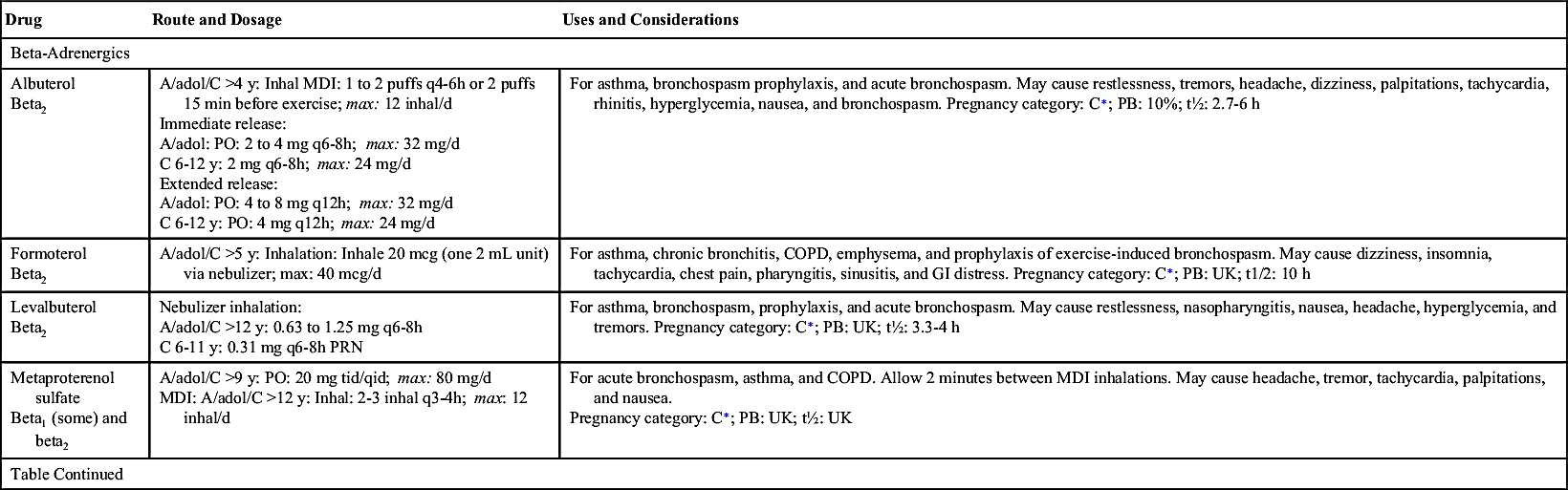
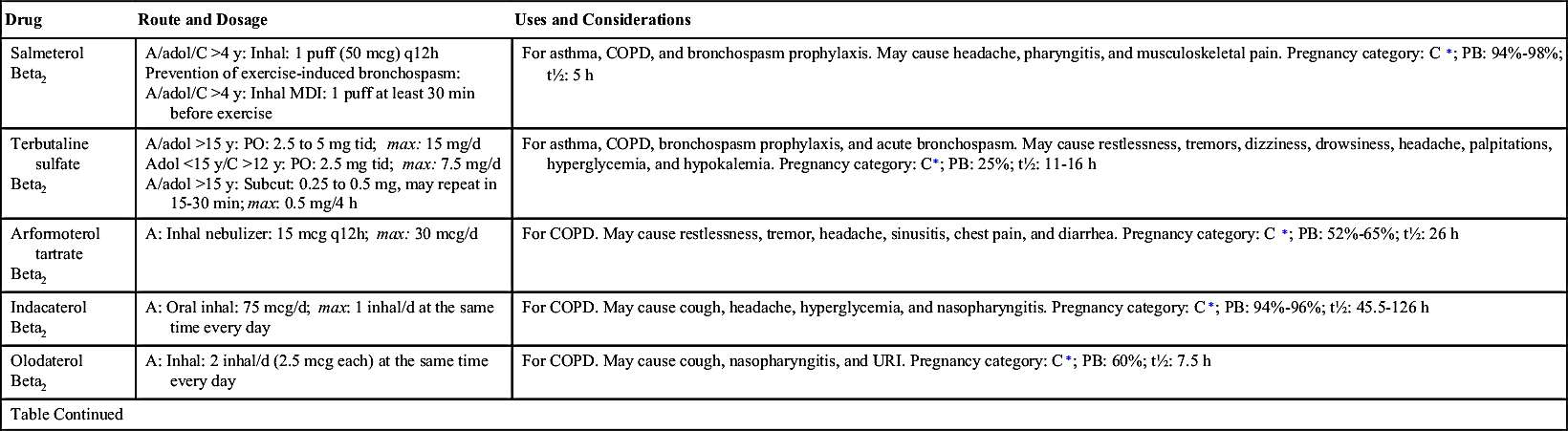
Excessive use of the aerosol drug can lead to tolerance and loss of drug effectiveness. Occasionally, severe paradoxic airway resistance (bronchoconstriction) develops with repeated, excessive use of sympathomimetic oral inhalation. Frequent dosing can cause tremors, nervousness, and increased heart rate. Table 36.1 lists the sympathomimetics used as bronchodilators.
Side Effects and Adverse Reactions
The side effects and adverse reactions of epinephrine include tremors, dizziness, hypertension, tachycardia, heart palpitations, cardiac dysrhythmias, and angina. The patient needs to be closely monitored when epinephrine is administered.
The side effects associated with beta2-adrenergic drugs, such as albuterol, include tremors, headaches, nervousness, increased pulse rate, and palpitations (high doses). The beta2 agonists may increase blood glucose levels, so patients with diabetes should be taught to closely monitor their serum glucose levels. Side effects of beta2 agonists may diminish after 1 week or longer. The bronchodilating effects may decrease with continued use. It is believed that tolerance to these drugs can develop; if this occurs, the dose may need to be increased. Failure to respond to a previously effective dose may indicate worsening asthma that requires reevaluation before increasing the dose.
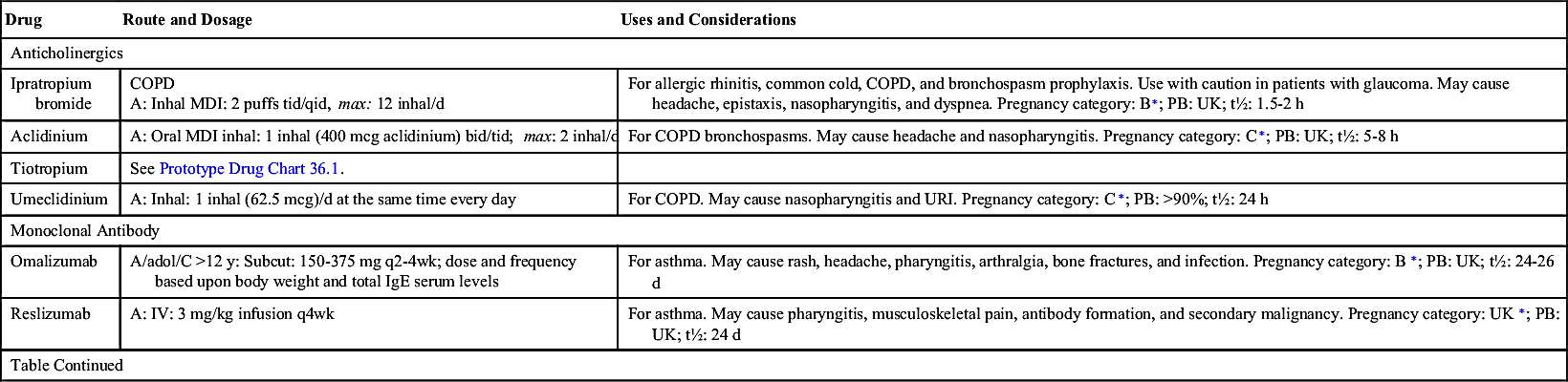
Anticholinergics
Tiotropium is an anticholinergic drug used for maintenance treatment of bronchospasms associated with COPD. This drug is administered by inhalation only with the HandiHaler device (dry-powder capsule inhaler). Patients should discard any capsules that are opened and not used immediately. HandiHalers should be washed with warm water and dried. The most common adverse effects of tiotropium include dry mouth, constipation, vomiting, dyspepsia, abdominal pain, depression, insomnia, headache, joint pain, and peripheral edema. Chest pain has been reported following tiotropium administration. Prototype Drug Chart 36.1 lists the drug data related to tiotropium.
The anticholinergic drug ipratropium bromide is used to treat asthmatic conditions by dilating the bronchioles. Unlike other anticholinergics, ipratropium bromide has few systemic effects. It is administered by MDI.
The combination of ipratropium bromide with albuterol sulfate is used to treat COPD. The combination is more effective and has a longer duration of action than either agent used alone. These two agents combined increase the FEV1, the index used to evaluate asthma and obstructive lung disease and the patient’s response to bronchodilator therapy. Table 36.2 lists the inhalants for asthma control.
Methylxanthine (Xanthine) Derivatives
The second major group of bronchodilators used to treat asthma is the methylxanthine (xanthine) derivatives, which include aminophylline, theophylline, and caffeine. Xanthines also stimulate the central nervous system (CNS) and respiration, dilate coronary and pulmonary vessels, and cause diuresis. Because of their effect on respiration and pulmonary vessels, xanthines are used in the treatment of asthma.
Theophylline
Theophylline relaxes the smooth muscles of the bronchi, bronchioles, and pulmonary blood vessels by inhibiting the enzyme phosphodiesterase, resulting in an increase in cAMP, which promotes bronchodilation.
Theophylline has a low therapeutic index and a narrow desired therapeutic range (5-15 mcg/mL). The serum or plasma theophylline concentration level should be monitored frequently to avoid severe adverse effects. Toxicity is likely to occur when the serum level is greater than 20 mcg/mL. Certain theophylline preparations can be given with sympathomimetic (adrenergic) agents, but the dose may need to be adjusted.
Theophylline was once used as the first-line drug for treating patients with chronic asthma and other COPDs. However, theophylline use has declined sharply because of a potential danger of serious adverse effects—including dysrhythmias, convulsions, and cardiorespiratory collapse—and efficacy has not been found to be greater than that of beta agonists or glucocorticoids. Because of its numerous adverse reactions, drug-drug interactions, and narrow therapeutic drug range, theophylline is prescribed mostly for maintenance therapy in patients with chronic stable asthma and other COPDs when other drugs have failed to show improvement. Theophylline drugs are not prescribed for patients with seizure disorders or cardiac, renal, or liver disease. Patients who receive theophylline preparations need to be closely monitored for serious side effects and drug interactions.