DRUG CLASSES
Aminosalicylates
Antidiarrheals
Antiflatulents
Laxatives
The large intestine is responsible for the absorption of water and some of the nutrients from the food and fluids we eat. The speed of transit determines what will be absorbed. Transit of contents rapidly through the bowel is called diarrhea. When contents move sluggishly, more water is absorbed, and the fecal material gets harder, resulting in constipation. Transit can be triggered by many things. Illness, such as irritable bowel syndrome or ulcerative colitis; bacterial infection; or drugs such as anti-infectives can make transit faster, resulting in diarrhea. Conditions such as Parkinson’s disease can slow the bowel, causing constipation. Treatment with opioid drugs and the aftereffects of abdominal surgery can also cause constipation.
Conditions that affect the function of the lower GI system can have a significant impact on activities of daily living; if proper absorption does not occur, people may not have the energy to engage in activities. One such condition that affects function is inflammatory bowel disease (IBD; Fig. 41.1). Another condition, irritable bowel syndrome (IBS), also affects the lower GI system. The pain and bloating of a sluggish bowel or fear of stool incontinence may prevent people from socializing, again affecting daily life. The drugs described in this chapter affect the function of the bowel. Antidiarrheals and laxatives, as well as drugs to treat IBD and IBS, are presented. Some of the more common drugs are listed in the Summary Drug Table: Lower Gastrointestinal System Drugs.
PHARMACOLOGY IN PRACTICE

Betty Peterson comes into the clinic and states, “Things just aren’t right.” During your assessment you learn she has become constipated after taking a cold preparation recently. After reading this chapter, determine why Betty has constipation and what should be recommended to help her.
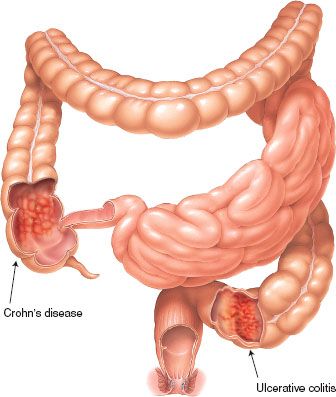
Figure 41.1 Examples of inflammatory bowel diseases. (Courtesy of Anatomical Chart Co.)
Inflammatory Bowel Disease
According to the Crohn’s and Colitis Foundation of America (2012), as many as 1.4 million Americans have IBD. The term IBD is used collectively for Crohn’s disease and ulcerative colitis, diseases that cause inflammation in the intestines. The cause of these diseases is unknown, although it is thought that a virus or bacterial organism interacting with the body’s immune system may be the cause. Clinical manifestations of Crohn’s disease include abdominal pain and distention. As the disease progresses, other GI symptoms present, such as anorexia, diarrhea, weight loss, dehydration, and nutritional deficiencies. Ulcerative colitis has a more abrupt onset; patients experience the sudden need to defecate, resulting in severe, blood- and mucus-filled diarrhea or no stool at all. Pain and fatigue accompany this disorder as well. No evidence has been found to support the theory that IBD is caused by tension, anxiety, or any other psychological factor or disorder (NIH, 2012). Drugs used to treat IBD include antibiotics, corticosteroids, biologic agents, and aminosalicylates. Aminosalicylates are described in this chapter; other drugs used in the treatment of IBD are included in their respective chapters.
AMINOSALICYLATES
Actions and Uses
Aminosalicylates are aspirin-like compounds with anti-inflammatory action. The drugs exert a topical anti-inflammatory effect in the bowel. The exact mechanism of action of these drugs is unknown. The aminosalicylates are used to treat Crohn’s disease and ulcerative colitis as well as other inflammatory diseases.
Adverse Reactions
Because these drugs are topical anti-inflammatory drugs, the most common adverse reactions happen in the GI system and include abdominal pain, nausea, and diarrhea. Other general adverse reactions include headache, dizziness, fever, and weakness.
Contraindications and Precautions
Aminosalicylates are contraindicated in patients with a known hypersensitivity to the drugs or salicylate-containing drugs. In addition, these drugs are contraindicated in patients who have hypersensitivity to sulfonamides and sulfites or intestinal obstruction, and in children younger than 2 years. Aminosalicylates are pregnancy category B drugs (except olsalazine, which is in pregnancy category C); all are used with caution during pregnancy and lactation (safety has not been established).
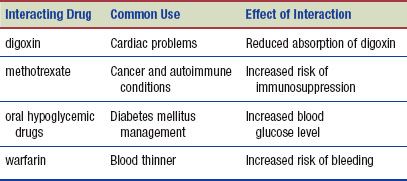
Interactions
The following interactions may occur when an aminosalicylate is administered with another agent:
 HERBAL CONSIDERATIONS
HERBAL CONSIDERATIONS
Chamomile has several uses in traditional herbal therapy, including as a mild sedative and for treatment of digestive upsets, menstrual cramps, and stomach ulcers. It has been used topically for skin irritation and inflammation. Chamomile is on the U.S. Food and Drug Administration (FDA) list of herbs generally recognized as safe. It is one of the most popular teas in Europe. When used as an infusion, it appears to produce an antispasmodic effect on the smooth muscle of the GI tract and to protect against the development of stomach ulcers. Although the herb is generally safe and nontoxic, the infusion is prepared from the pollen-filled flower heads and has resulted in mild symptoms of contact dermatitis to severe anaphylactic reactions in individuals hypersensitive to ragweed, asters, and chrysanthemums (DerMarderosian, 2003).
ANTIDIARRHEALS
Actions and Uses
Antidiarrheals are used in the treatment of diarrhea. Difenoxin (Motofen) and diphenoxylate (Lomotil) are chemically related to opioid drugs; therefore, they decrease intestinal peristalsis, which often is increased when the patient has diarrhea. Because these drugs are opioid related, they may have sedative and euphoric effects, but no analgesic activity. A drug dependence potential exists; therefore, the drugs are combined with atropine (a cholinergic blocking drug), which causes dry mouth and other mild adverse effects. Abuse potential is reduced because of these unpleasant adverse effects.
Loperamide (Imodium) acts directly on the muscle wall of the bowel to slow motility and is not related to the opioids. It therefore is also used in treating chronic diarrhea associated with IBD.
Adverse Reactions
Gastrointestinal System Reactions
• Anorexia, nausea, vomiting, and constipation
• Abdominal discomfort, pain, and distention
Other System Reactions
• Dizziness, drowsiness, and headache
• Sedation and euphoria
• Rash
Contraindications and Precautions
These drugs are contraindicated in patients whose diarrhea is associated with organisms that can harm the intestinal mucosa (Escherichia coli, Salmonella and Shigella spp.). Patients with pseudomembranous colitis, abdominal pain of unknown origin, and obstructive jaundice also should not take antidiarrheals. Antidiarrheal drugs are contraindicated in children younger than 2 years of age.
 NURSING ALERT
NURSING ALERT
If diarrhea persists for more than 2 days when over-the-counter (OTC) antidiarrheal drugs are being used, the patient should discontinue use and seek treatment from the primary health care provider.
The antidiarrheal drugs are used cautiously in patients with severe hepatic impairment. Antidiarrheals are classified as pregnancy category C drugs and should be used cautiously during pregnancy and lactation. Loperamide is a pregnancy category B drug but is not recommended for use during pregnancy and lactation.
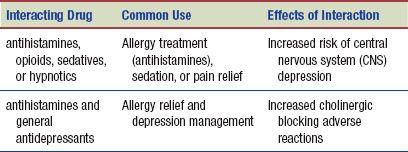
Interactions
The following interactions may occur when an antidiarrheal drug is administered with another agent:

ANTIFLATULENTS
Actions
Simethicone (Mylicon) and charcoal are used as antiflatulents (drugs that reduce flatus or gas in the intestinal tract). These drugs do not absorb or remove gas; rather, they act to help the body release the gas by belching or flatus (passing gas). Simethicone has a defoaming action that disperses and prevents the formation of gas pockets in the intestine. Charcoal helps bind gas for expulsion.
Uses
Antiflatulents are used to relieve painful symptoms of excess gas in the digestive tract that may be caused by the following:
• Postoperative gaseous distention and air swallowing
• Dyspepsia (fullness or epigastric discomfort)
• Peptic ulcer
• Irritable bowel syndrome or diverticulosis
In addition to its use for the relief of intestinal gas, charcoal may be used in the prevention of nonspecific pruritus associated with kidney dialysis treatment and as an antidote in poisoning. Simethicone is in some antacid products, such as Mylanta Liquid and Di-Gel Liquid.
Adverse Reactions
No adverse reactions have been reported with the use of antiflatulents.
Contraindications and Precautions
Antiflatulents are contraindicated in patients with known hypersensitivity to any components of the drug. The pregnancy category of simethicone has not been determined; because it is not absorbed, it may be safe for use during pregnancy, although the primary health care provider should be consulted whenever any drug is to be taken. Charcoal is a pregnancy category C drug.
Interactions
There may be a decreased effectiveness of other drugs because of adsorption by charcoal, which can also adsorb other drugs in the GI tract. There are no known interactions with simethicone.
LAXATIVES
Actions
There are various types of laxatives (see the Summary Drug Table: Lower Gastrointestinal System Drugs). The action of each laxative is somewhat different, yet they all produce the same result—relief of constipation. The manner of action of the various laxative groups is explained in Display 41.1.
Display 41.1 Actions of Different Types of Laxatives
- Bulk-producing laxatives are not digested by the body and therefore add bulk and water to the contents of the intestines. The added bulk in the intestines stimulates peristalsis, moves the products of digestion through the intestine, and encourages evacuation of the stool. Examples of bulk-forming laxatives are psyllium (Metamucil) and polycarbophil (FiberCon). Sometimes these laxatives are used with severe diarrhea to add bulk to the watery bowel contents and slow transit through the bowel.
- Emollient laxatives lubricate the intestinal walls and soften the stool, thereby enhancing passage of fecal material. Mineral oil is an emollient laxative.
- Stool softeners promote water retention in the fecal mass and soften the stool. One difference between emollient laxatives and stool softeners is that the emollient laxatives do not promote the retention of water in the stool. Examples of stool softeners include docusate (Colace).
- Hyperosmolar drugs dehydrate local tissues, which causes irritation and increased peristalsis, with consequent evacuation of the fecal mass. Glycerin is a hyperosmolar drug.
- Irritant or stimulant laxatives increase peristalsis by direct action on the intestine. An example of an irritant laxative is senna (Senokot) or bisacodyl.
- Saline laxatives attract or pull water into the intestine, thereby increasing pressure in the intestine, followed by an increase in peristalsis. Magnesium (Milk of Magnesia) is a saline laxative.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


