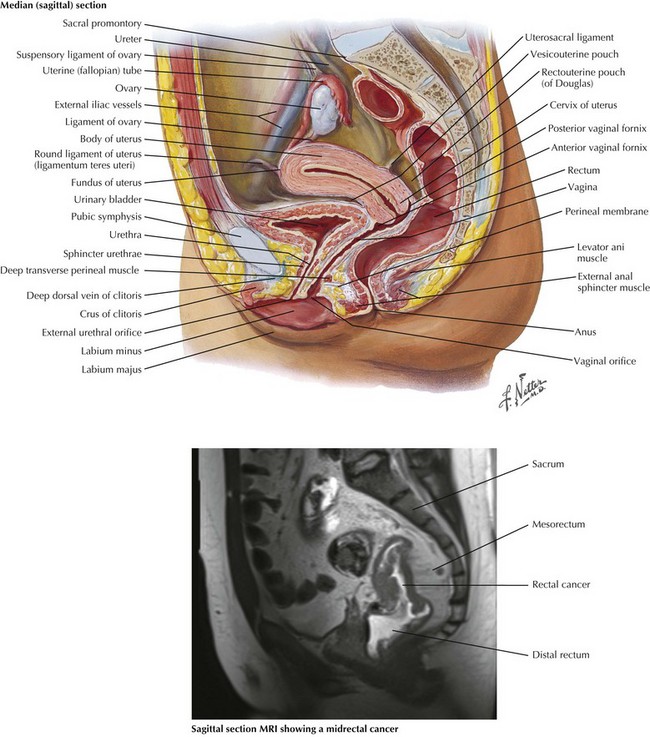
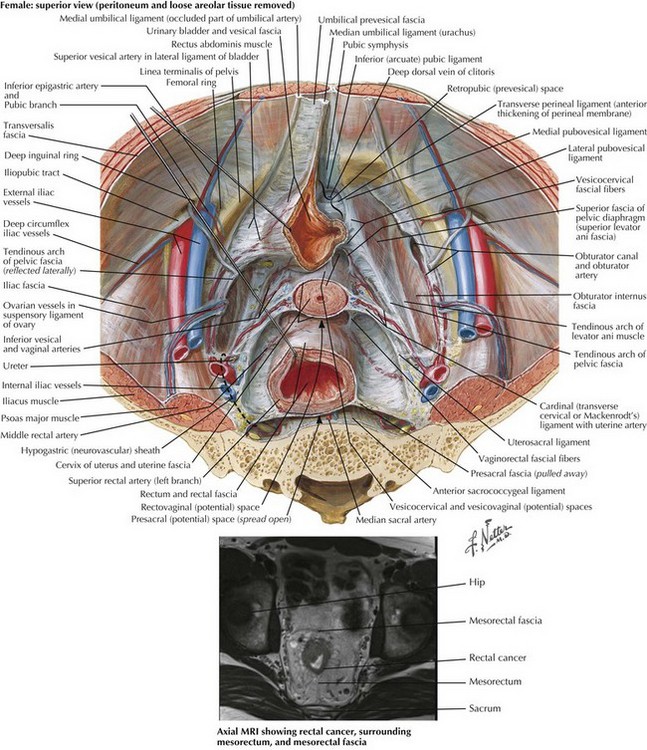
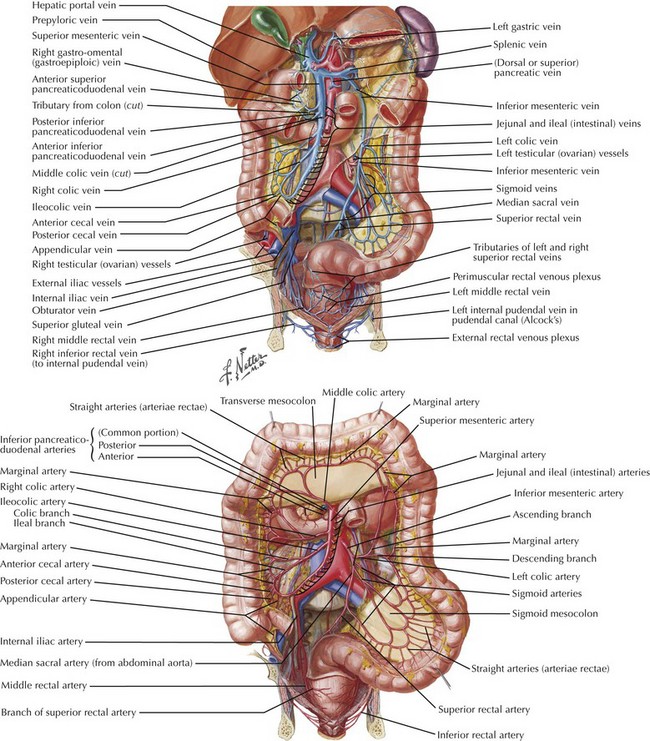
Chapter 24 The current standards of care for patients with low rectal cancer include complete excision of the rectum and surrounding mesorectum, generally ensuring a minimal distal margin of 2 cm before a coloanal anastomosis is performed. In general, this procedure is performed in conjunction with a high ligation of the inferior mesenteric artery and vein and mobilization of the splenic flexure (see Chapter 22). The autonomic nerves are carefully protected. Patients with colon cancer require a minimum 5-cm proximal and distal margin, with at least 12 lymph nodes being harvested in the mesocolic excision. Patients with rectal cancer require a 1- to 2-cm margin depending on anatomy, tumor location, and tumor differentiation. Preoperative imaging of rectal cancer is extremely important and helps define tumors that may threaten the circumferential resection margin, therefore requiring preoperative chemoradiation. Both sagittal and coronal views are obtained, and magnetic resonance imaging (MRI) is used more frequently because of the high-quality resolution obtained (Figs. 24-1 and 24-2). Ultrasound is also used in the assessment of rectal cancer and can provide excellent results for T staging (tumor infiltration), particularly of early T-stage lesions. The anatomy of the vascular supply to the colon is demonstrated in Figure 24-3. A knowledge of these vessels, the autonomic nerves, and the ureters is required before the surgeon begins the steps of the procedure (Figs. 24-4 and 24-5).
Low Anterior Resection with Total Mesorectal Excision and Anastomosis
Surgical Principles
Anatomy for Preoperative Imaging
Anatomy for Colonic Mobilization and Dissection
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Basicmedical Key
Fastest Basicmedical Insight Engine