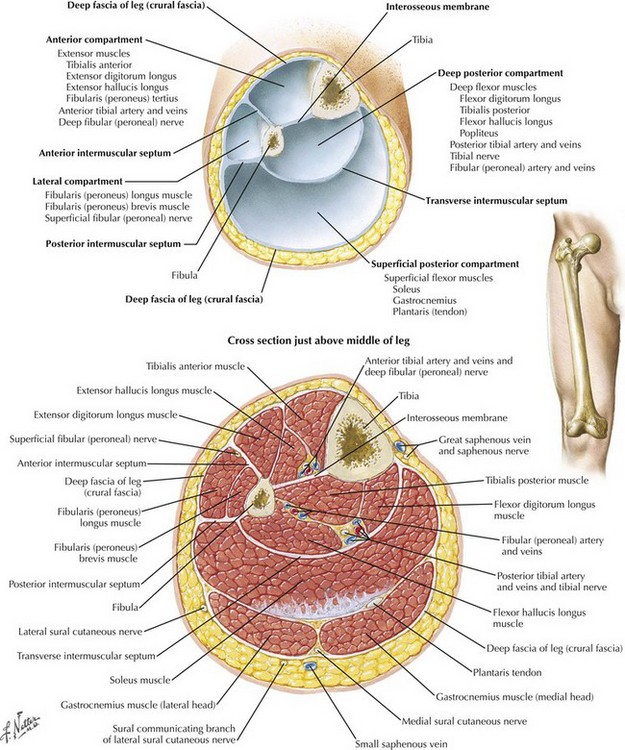
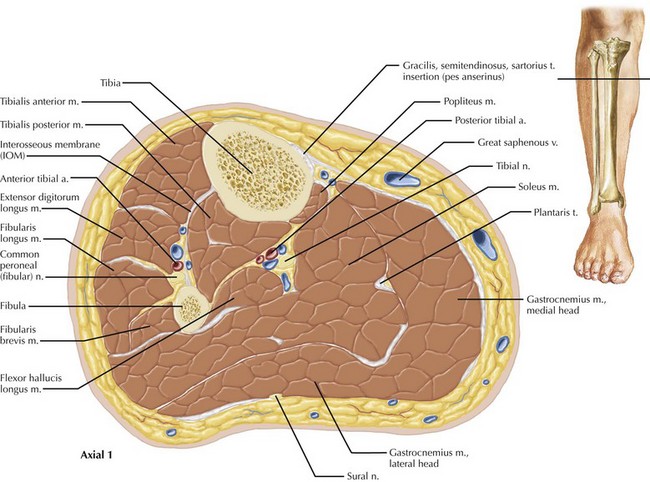
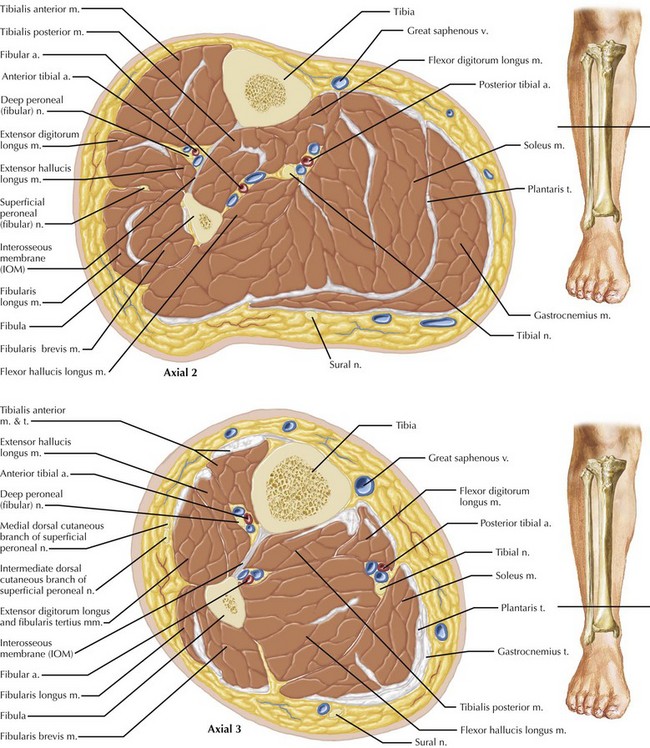
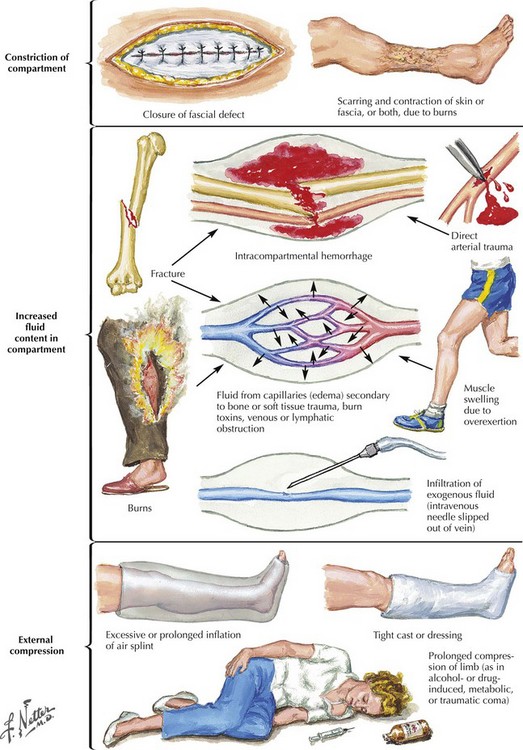
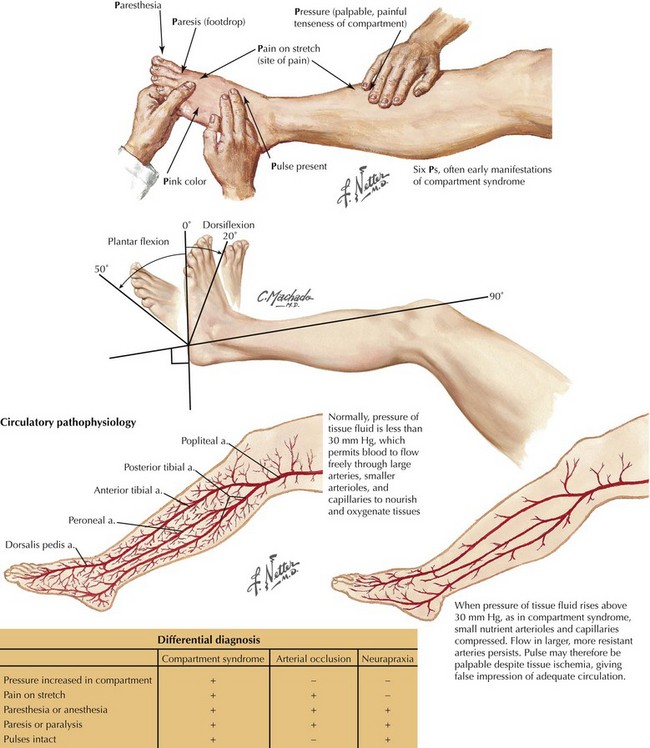
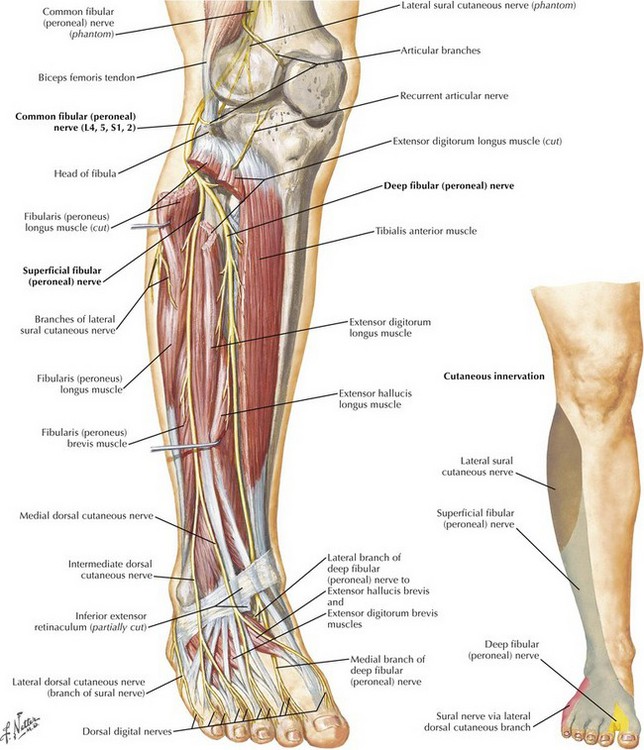
Chapter 42 The lower leg is divided into four compartments: anterior, lateral, superficial posterior, and deep posterior (Fig. 42-1). The anterior compartment is especially prone to ischemic injury because of its relative paucity of collateral arterial supply. Compared with the other compartments, especially the posterior compartments, the anterior compartment is also more firmly constrained. The spatial relationships among the nerve, vascular, muscular, and bony structures change from proximal to distal in the leg, an especially relevant consideration in performing complete lysis of the posterior compartments (Figs. 42-2 and 42-3). Compartment syndrome occurs when the compartmental pressure rises sufficiently to prevent adequate tissue perfusion. This condition can result from increased volume in the compartment caused by bleeding, infiltration of exogenous fluid, or reperfusion edema (Fig. 42-4). Increased compartment pressures can also result from external constraint on the compartment, such as with casts, braces, or bandages. A compartment pressure greater than 30 mm Hg is accepted as sufficiently elevated to cause compartment syndrome. This pressure is usually sufficient to restrict venous outflow from the compartment, thereby leading to further increases in compartment pressure. In the appropriate clinical setting, compartment syndrome should always be considered. Pain is the most prevalent symptom, but the patient may report diminished motor strength and altered or reduced sensation (Fig. 42-5). Pain with passive movement and palpation is extremely common, although the absence of pain in the extremity with compromised neurologic function can be misleading. Light touch sensation is often diminished before the development of motor weakness and can best be tested in the web space between the first and second toes. Touch sensation reflects the function of the deep peroneal nerve (Fig. 42-6).
Leg and Forearm Fasciotomy
Leg Fasciotomy
Etiology of Compartment Syndrome
Clinical Diagnosis and Decision Making
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Leg and Forearm Fasciotomy