Invasive Papillary Carcinoma
Key Facts
Terminology
Invasive papillary carcinoma (IPC)
Invasive carcinomas consisting predominantly of papillae with fibrovascular cores
“Papillary carcinoma” includes invasive papillary carcinoma, encapsulated papillary carcinoma, solid papillary carcinoma, papillary carcinoma in situ, and DCIS involving papilloma
Invasive papillary carcinoma is important to identify as risk of lymph node and distant metastases is higher than for other diagnoses
Clinical Issues
< 2% of breast carcinomas
More common in postmenopausal women (typically 65-70 years of age)
Outcome is generally better than for invasive carcinomas of no special type
Papillary carcinomas are generally ER positive and only rarely poorly differentiated
Only rare papillary carcinomas are HER2 positive
Lymph node metastases are present in about 1/3 of cases
Top Differential Diagnoses
Invasive micropapillary carcinoma
Outcome less favorable than IPC
Lymph node metastases are present in majority of cases
Solid papillary carcinoma
Most have outcomes similar to DCIS
Encapsulated (intracystic) papillary carcinoma
Most have outcomes similar to DCIS
TERMINOLOGY
Abbreviations
Invasive papillary carcinoma (IPC)
Definitions
Invasive carcinomas consisting predominantly of papillae with fibrovascular cores
“Papillary carcinoma” includes invasive papillary carcinoma, encapsulated papillary carcinoma, solid papillary carcinoma, papillary carcinoma in situ, and DCIS involving papilloma
These lesions are sometimes grouped together
Invasive papillary carcinoma is important to identify as risk of lymph node and distant metastases is higher than for other diagnoses
CLINICAL ISSUES
Epidemiology
Incidence
< 2% of breast carcinomas
Age
More common in postmenopausal women (typically 65-70 years of age)
Prognosis
Outcome is generally better than for invasive carcinomas of no special type
Papillary carcinomas are generally ER positive and only rarely poorly differentiated
Lymph node metastases are present in about 1/3 of cases
MACROSCOPIC FEATURES
Gross Appearance
IPC generally has appearance similar to cancers of no special type in having an irregular border
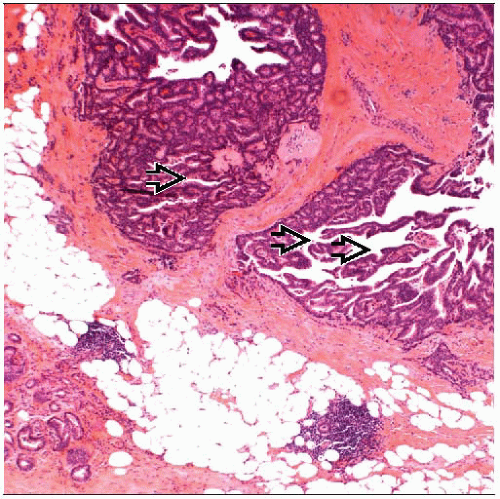
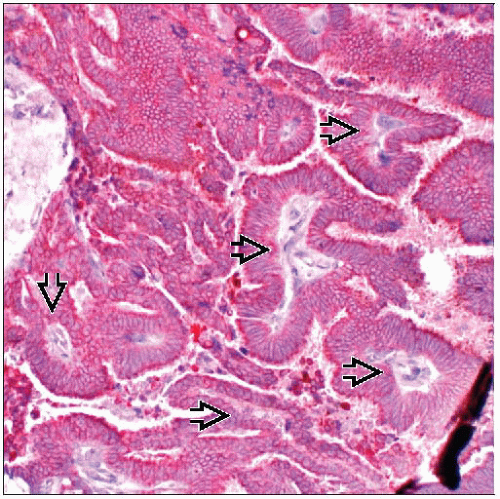
MICROSCOPIC PATHOLOGY
Histologic Features
Should have prominent pattern of papillae with fibrovascular cores
Papillae lack myoepithelial cells
IHC for muscle markers may be difficult to interpret as blood vessels may closely approximate basal portions of cells in fibrovascular cores
p63 is generally easier to interpret as blood vessels will be negative
Occasional tumor cells may be positive for p63
Fibrovascular cores are thin and delicate
Cells are monomorphic in appearance and columnar in shape
Nuclear grade is generally low or intermediate
Mitoses are usually infrequent
DCIS of papillary type may be associated with carcinoma
ANCILLARY TESTS
Immunohistochemistry
Estrogen and progesterone receptors
Majority of invasive papillary carcinomas are positive for hormone receptors
HER2
Only rare papillary carcinomas overexpress HER2
DIFFERENTIAL DIAGNOSIS
Invasive Micropapillary Carcinoma
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree