Invasive Ductal Carcinoma (Adenocarcinomas of No Special Type)
Key Facts
Terminology
Invasive ductal carcinoma includes carcinomas not classified as a special histologic type
Synonymous with “no special type” or “not otherwise specified” carcinoma
Etiology/Pathogenesis
Heterogeneous with regard to pathologic features, prognosis, and clinical outcome
˜ 75% of invasive breast cancers
4 types based on ER, PR, HER2, & proliferation
Luminal A, luminal B, HER2, and basal types
˜ 1 in 8 women will develop breast cancer during her lifetime
Median age at diagnosis: 61 years
< 15% diagnosed before age 44
Clinical Issues
For women < 40, 85% detected as a palpable mass and 15% by screening
For women > 40, 60% detected by screening and 40% as a palpable mass
Image Findings
Masses, calcifications, and architectural distortion
Top Differential Diagnoses
Special histologic types
Ductal carcinoma in situ
Sclerosing lesions
Microglandular adenosis
Epithelial displacement
Other types of malignant tumors
Metastatic tumors to the breast
TERMINOLOGY
Abbreviations
Invasive ductal carcinoma (IDC)
Synonyms
Infiltrating ductal carcinoma
Not otherwise specified (NOS) carcinoma
No special type (NST) carcinoma
Definitions
IDC includes all adenocarcinomas of the breast that are not classified as a special histologic type
ETIOLOGY/PATHOGENESIS
Classification
IDC is a heterogeneous group of adenocarcinomas with regard to pathologic features, prognosis, and clinical outcome
Termed “ductal” because associated ductal carcinoma in situ expands and unfolds lobular units; thus resembles ducts more than lobules
In contrast, lobular carcinoma in situ expands but usually does not distort lobules; the type of associated invasive carcinoma was termed “lobular” carcinoma
All carcinomas are thought to arise from terminal duct lobular unit
Terms “ductal” and “lobular” do not indicate cell or structure of origin
˜ 75% of invasive breast cancers
Remaining (˜ 25%) are defined as special histologic types based on morphologic features
For small screen-detected cancers, ˜ 60% are of special histologic type
Therefore, most studies of “breast cancer” are primarily of IDC
IDC can be divided into 4 major types: Luminal A, luminal B, HER2, and basal-like
Gene expression profiling demonstrates that each type shares global expression patterns
Same cancer types can be defined based on expression of ER, PR, HER2, and proliferation
Subtypes defined by profiling and IHC overlap by 80-85%
Although groups originally defined by expression profiling, convenient to use the same names to describe the very similar groups of cancers as defined by IHC
Here, basal-like carcinoma and triple negative breast carcinoma are described as 1 group
Classification by IHC has the advantage of organizing cancers according to therapeutic targets and likely response to chemotherapy
Some HER2 carcinomas defined by expression profiling do not overexpress HER2
Not yet clear if expression profiling adds sufficient additional information to warrant its use for routine classification
CLINICAL ISSUES
Epidemiology
Incidence
In USA, 1 woman in 8 (˜ 12%) will develop breast cancer in her lifetime
Highest incidence is for white women, and lowest incidence is for Native-American women
African-American women have a lower incidence compared to white women but higher mortality rates
Hispanic women have both lower incidence and lower mortality rates
Age
Median at diagnosis: 61 years
< 15% of cases diagnosed before age 44
Gender
All females are at high risk for breast cancer
Only 1 of 100 breast cancer cases occur in men
Presentation
Patients most commonly present with a palpable mass or abnormality on screening
For women < 40, 85% of carcinomas are detected as a palpable mass and 15% on breast imaging
Imaging may occur in this age group due to family history or as part of a work-up for a clinical finding (e.g., nipple discharge, pain, or skin changes)
For women > 40, 60% of carcinomas are detected by screening and 40% as a palpable mass
Some cancers are not detected by mammography
Obscured by dense breast tissue
Present in unusual location and missed by routine views
Become apparent between screenings due to rapid growth (“interval” cancer)
> 85% of palpable cancers are detected by the patient, the remainder by physician examination
Self breast examination has not been shown to decrease death rate from breast cancer
Suggests that cancers that are capable of metastasizing will have done so by the time they become palpable
Palpable cancers are typically larger (2-3 cm) than screen-detected (1-2 cm) cancers
Palpable cancers have a less favorable prognosis compared to nonpalpable cancers of the same size
Uncommon presentations of breast cancer are nipple discharge, Paget disease, pain, or metastasis
Treatment
Most patients will be treated with multiple modalities
Surgery: Controls local disease and may be curative for localized cancers
Radiation therapy: Reduces local recurrences and has a small effect on survival
Endocrine therapy: Improves survival for patients with hormone-sensitive cancers
Chemotherapy: Improves survival in subsets of patients with sensitive cancers; general correlation with higher proliferative rates
HER2-targeted therapy improves survival for carcinomas with overexpression
Prognosis
Wide range of probable survival for IDC depending upon prognostic and predictive factors
Stage: Based on size, chest wall or skin involvement, and lymph node involvement
Grade: Modified Bloom-Richardson grade should be provided for all breast carcinomas
Subtype: Includes ER, PR, HER2, and proliferation
Lymph-vascular invasion
Response to therapy: May be evaluated if neoadjuvant therapy is used
Gene expression profiling can also be used to determine prognosis in ER-positive IDC
Several different profiles are commercially available
Profiles are largely driven by genes related to proliferation
Outcome is highly dependent on treatment
Reduction in the death rate from cancer is attributed to both improved detection of earlier cancers by screening and to systemic therapy
IMAGE FINDINGS
Mammographic Findings
Masses, calcifications, and architectural distortion correlated with IDC
Vast majority of IDCs form irregular masses due to infiltration into surrounding stroma
Only benign lesions that typically have this appearance are radial sclerosing lesions or inflammatory lesions (e.g., prior surgical sites or infections)
Less common for IDC to have circumscribed or lobulated borders
Basal-like/triple negative cancer most likely to have this appearance
Special histologic types of mucinous carcinoma and medullary carcinoma also have circumscribed borders
Calcifications are most commonly present in associated DCIS
IDCs detected as calcifications without a mass are typically very small (< 1 cm)
Calcifications are occasionally present in secretory material or necrosis in the IDC
Architectural distortion is uncommon finding
Carcinomas with this appearance are usually diffusely invasive with minimal stromal response
Invasive lobular carcinomas are most common carcinoma with this finding
Ultrasonographic Findings
Borders of invasive carcinomas by ultrasound usually correlate with the shape seen on mammography
Almost all carcinomas are hypoechoic as cancers consist of tumor cells and fibrous desmoplastic stroma
Very rarely, cancers can be hyperechoic due to infiltrative pattern into adipose tissue with minimal stromal response
Not very useful as a screening modality due to low specificity
Most helpful to further define lesions detected by mammography or MR
Size by ultrasound has best correlation with gross tumor size
MR Findings
Carcinomas are detected by MR due to quick uptake of contrast agents, resulting in rapid enhancement
Shape of masses on imaging does not correlate well with actual borders of lesion
MR overestimates size in a significant percentage of patients
MR is very sensitive (few cancers are occult by this modality) but not very specific
Not recommended for screening except for very high-risk populations
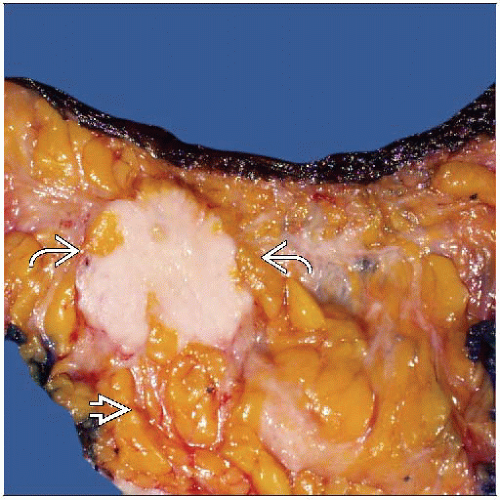
MACROSCOPIC FEATURES
General Features
Majority of IDCs are very hard by palpation
Often “gritty” when cut
Cut surface is typically gray-white
Carcinomas typically have irregular borders
Less common are carcinomas with circumscribed or lobulated borders
Size
Important prognostic factor and is used for AJCC T classification
Best determined by palpation rather than visual inspection
Cancers are often white (like adjacent fibrous breast stroma); can be difficult to see edges
Usually a palpable shelf between edge of tumor and normal breast tissue
Extent can be determined by pinching the mass between 2 fingers
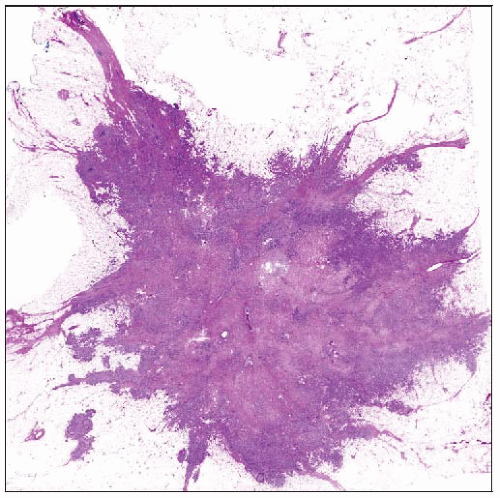
MICROSCOPIC PATHOLOGY
Histologic Features
Histologic appearances vary according to subtype
Subtypes are not considered “special histologic types,” as final classification depends on protein expression patterns rather than morphology
However, majority of cancers in each subtype have characteristic histologic features
Luminal A type
Majority grade 1 or 2
Generally, pattern of well-formed tubules, cribriform nests, or papillae
Nuclei are small to moderate in size with minute or absent nucleoli and minimal pleomorphism
Mitoses are absent or rare
Necrosis would be very unusual
Luminal B type
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree