Figure 5–1 Neurotransmission in the autonomic and somatic nervous systems. The parasympathetic nervous system consists of cranial and sacral nerves with long preganglionic and short postganglionic fibers. The sympathetic nervous system consists of thoracic and lumbar nerves with short preganglionic and long postganglionic fibers. The sympathetic system includes the adrenal medulla, which releases norepinephrine and epinephrine into the blood. The somatic nervous system consists of motor neurons to the skeletal muscle. α = α-adrenoceptors; ACh = acetylcholine; β = β-adrenoceptors; E = epinephrine; N = nicotinic receptors; NE = norepinephrine; M = muscarinic receptors.
As shown in Figure 5–2, the sympathetic and parasympathetic nervous systems often have opposing effects on organ function. Activation of the sympathetic system produces the “fight or flight” response, which enables a person to respond to threatening situations. During this response, cardiovascular stimulation provides skeletal muscles with the oxygen and energy substrates required to support vigorous physical activity. Increases in glycogenolysis and lipolysis also help provide the required energy fuels. The parasympathetic system is sometimes called the “rest and digest” system, because it slows the heart rate and promotes more vegetative functions, such as digestion, defecation, and micturition. Many parasympathetic effects (including pupillary constriction, bronchoconstriction, and stimulation of gut and bladder motility) are caused by smooth muscle contraction.
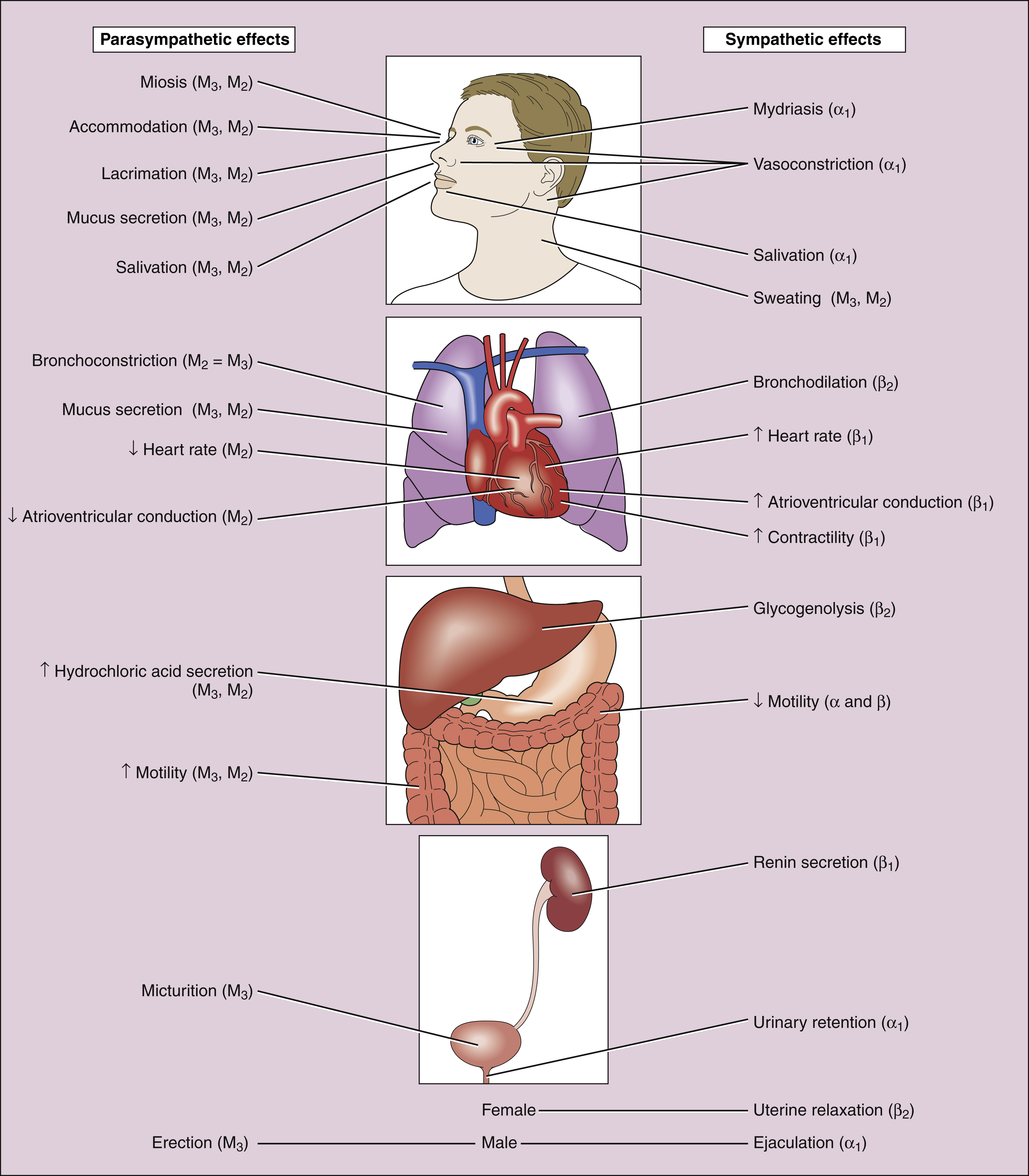
Figure 5–2 Autonomic nervous system effects on organs. All parasympathetic effects are mediated by muscarinic receptors. Sympathetic effects are mediated by α-adrenoceptors (a), β-adrenoceptors (β), or muscarinic receptors (M).
Somatic Nervous System
The somatic nervous system consists of the motor neurons to the skeletal muscle. These neurons have a single nerve fiber that releases acetylcholine at the neuromuscular junction.
Enteric Nervous System
The enteric nervous system (ENS) is sometimes called the third division of the autonomic nervous system. The ENS consists of a network of autonomic nerves that are located in the gut wall and regulate gastrointestinal motility and secretion. The ENS, which includes the submucosal, myenteric, and subserosal plexuses, receives innervation from the sympathetic and parasympathetic nervous systems. The ENS has afferent fibers and efferent fibers, and it integrates input received from autonomic nerves with localized reflexes to synchronize the waves of peristalsis (the propulsive contractions of gut muscle). Parasympathetic stimulation activates the ENS, whereas sympathetic stimulation inhibits the ENS. The ENS can function independently of autonomic innervation following autonomic denervation.
NEUROTRANSMITTERS AND RECEPTORS
Neurotransmitters
The primary neurotransmitters found in the autonomic and somatic nervous systems are acetylcholine and norepinephrine (see Fig. 5–1). The terms adrenergic and cholinergic refer to neurons that release norepinephrine or acetylcholine, respectively.
Acetylcholine is the transmitter at all autonomic ganglia, at parasympathetic neuroeffector junctions, and at somatic neuromuscular junctions. It is also the transmitter at a few sympathetic neuroeffector junctions, including the junctions of nerves in sweat glands and vasodilator fibers in skeletal muscle. The presence of acetylcholine in several types of autonomic and somatic synapses contributes to the lack of specificity of drugs acting on acetylcholine neurotransmission.
Although norepinephrine (noradrenaline) is the primary neurotransmitter at most sympathetic postganglionic neuroeffector junctions, epinephrine (adrenaline) is the principal catecholamine released from the adrenal medulla in response to activation of the sympathetic nervous system.
A number of other neurotransmitters have been identified in autonomic nerves of the ENS of the gastrointestinal tract, as well as in the genitourinary tract and certain blood vessels. The transmitters released by these neurons include neuropeptide Y, vasoactive intestinal polypeptide, enkephalin, substance P, serotonin (5-hydroxytryptamine), adenosine triphosphate, and nitric oxide. In some tissues, adenosine triphosphate released by these neurons is converted to adenosine, which can then activate adenosine receptors in a number of tissues (see Chapter 27). Nitric oxide is an important neurotransmitter that produces vasodilatation in a many vascular beds and is also found in the ENS.
Receptors for Acetylcholine, Norepinephrine, and Epinephrine
The acetylcholine receptors have been divided into two types, based on their selective activation by one of two plant alkaloids. Muscarinic (M) receptors, which are acetylcholine receptors activated by muscarine, are primarily located at parasympathetic neuroeffector junctions. Nicotinic receptors, which are acetylcholine receptors activated by nicotine, are found in all autonomic ganglia, at somatic neuromuscular junctions, and in the brain. Muscarinic receptors are subdivided based on molecular and pharmacologic criteria. Activation of the M3 receptor produces smooth muscle contraction (except sphincters) and gland secretion. Activation of the M2 receptor mediates cardiac slowing. The M1 receptor is primarily concerned with modulation of neurotransmission at central and peripheral sites. Activation of nicotinic receptors in autonomic ganglia excites neurotransmission, whereas activation of these receptors in skeletal muscle causes muscle contraction.
The receptors for norepinephrine and epinephrine at sympathetic neuroeffector junctions are called adrenoceptors, a term which is derived from adrenaline, another name for epinephrine. Two types of adrenoceptors, called α-adrenoceptors and β-adrenoceptors, are distinguished on the basis of their selective activation and blockade by adrenoceptor agonists and antagonists. These receptors have been further divided into several subtypes. The α1-adrenoceptors mediate smooth muscle contraction, whereas β2-adrenoceptors mediate smooth muscle relaxation. Activation of β1-adrenoceptors produces cardiac stimulation.
NEUROTRANSMISSION AND SITES OF DRUG ACTION
Cholinergic and adrenergic neurotransmission have many basic similarities. In both cases, the neurotransmitter is synthesized in nerve terminals, stored in membrane-bound vesicles, and released into the synapse in response to nerve stimulation. After the neurotransmitter activates postjunctional receptors to initiate a physiologic effect, neurotransmitter action is terminated either by metabolism or neuronal reuptake. Various drugs exert their effects at specific steps in the process.
Examples and sites of action for drugs that affect autonomic neurotransmission are shown in Figure 5–3, and the mechanisms of action are listed in Table 5–1.
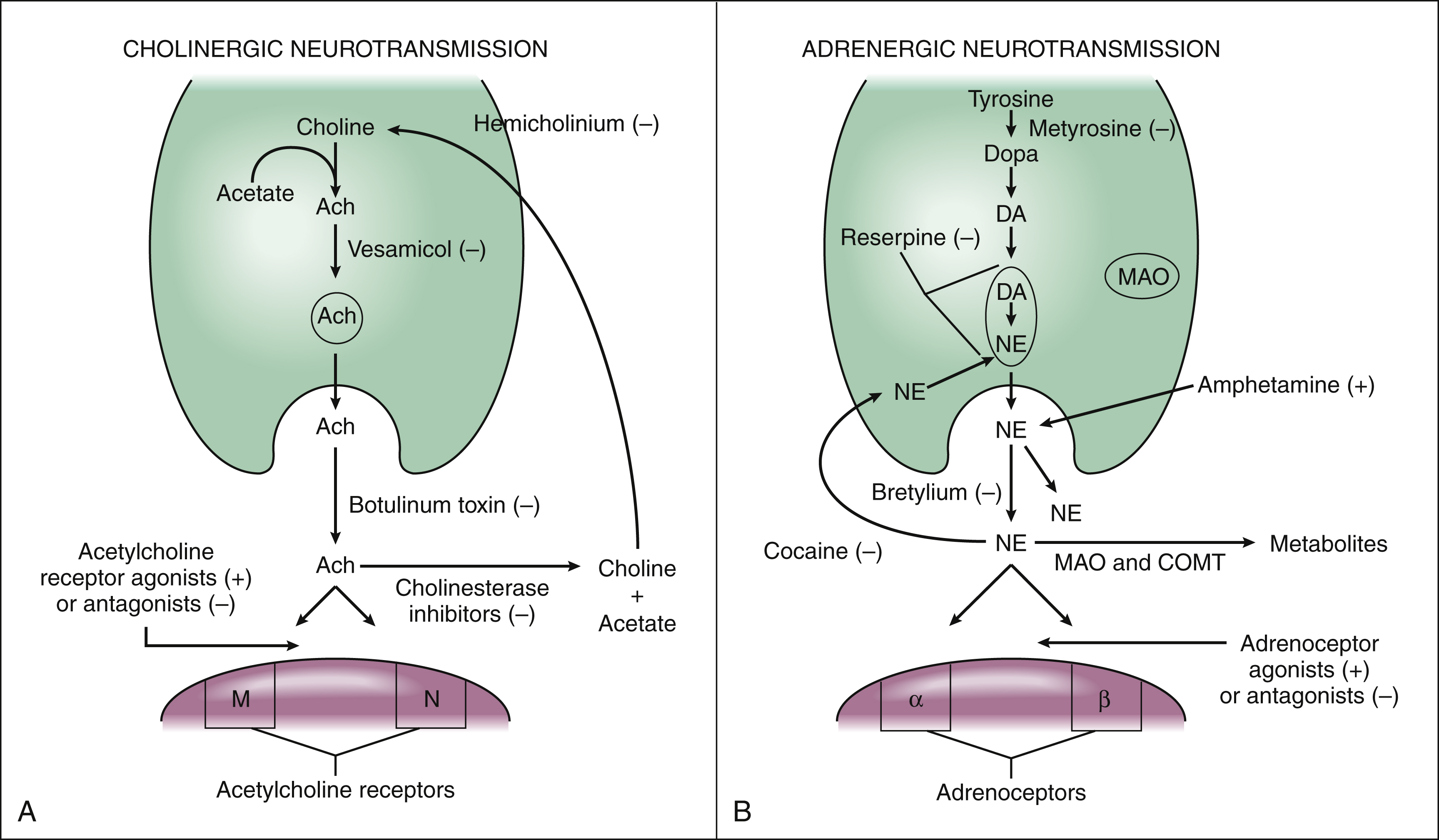
Figure 5–3 Cholinergic and adrenergic neurotransmission and sites of drug action. (A) Acetylcholine (ACh) is synthesized from choline and acetate, stored in neuronal vesicles, and released into the synapse by nerve stimulation. Hemicholinium blocks choline uptake by the neuron and inhibits ACh synthesis. Vesamicol blocks ACh storage, and botulinum toxin blocks ACh release. ACh breakdown is inhibited by cholinesterase inhibitors such as physostigmine. Postjunctional acetylcholine receptors are activated or blocked by acetylcholine receptor agonists or antagonists, respectively. (B) Norepinephrine (NE) is synthesized from tyrosine in a three-step reaction: tyrosine to dopa (dihydroxyphenylalanine), dopa to dopamine (DA), and dopamine to NE. The conversion of tyrosine to dopa is inhibited by metyrosine. The vesicular storage of DA and NE is blocked by reserpine, and the release of NE in response to nerve stimulation is blocked by bretylium. After activating postsynaptic receptors, NE is sequestered by neuronal reuptake, a process blocked by cocaine. Amphetamine indirectly increases the transport of NE into the synapse. Postsynaptic adrenoceptors are activated or blocked by adrenoceptor agonists or antagonists, respectively. α = α-adrenoceptors; β = β-adrenoceptors; COMT = catechol-O-methyltransferase; M = muscarinic receptors; MAO = monoamine oxidase; N = nicotinic receptors; (−) = inhibits; (+) = stimulates.
TABLE 5–1 Examples of Drugs Affecting Autonomic Neurotransmission
| Mechanism of Action | Drugs Affecting Acetylcholine Neurotransmission | Drugs Affecting Sympathetic Neurotransmission |
|---|---|---|
| Inhibit synthesis of neurotransmitter | Hemicholinium∗ | Metyrosine (alpha-methyl-para-tyrosine) |
| Prevent vesicular storage of neurotransmitter | Vesamicol∗ | Reserpine |
| Inhibit release of neurotransmitter | Botulinum toxin | Bretylium |
| Increase release of neurotransmitter | Black widow spider venom (α-latrotoxin)∗ | Amphetamine |
| Inhibit reuptake of neurotransmitter | — | Cocaine |
| Inhibit metabolism of neurotransmitter | Cholinesterase inhibitors (physostigmine) | Monoamine oxidase inhibitors (phenelzine) |
| Activate postsynaptic receptors | Acetylcholine, bethanechol, and pilocarpine | Albuterol, dobutamine, and epinephrine |
| Block postsynaptic receptors | Atropine and tubocurarine (block muscarinic and nicotinic receptors, respectively) | Phentolamine and propranolol (block α- and β-adrenoceptors, respectively) |
∗ These agents have no current medical use.
Cholinergic Neurotransmission
Acetylcholine is synthesized from choline and acetate in the neuronal cytoplasm by choline acetyltransferase, and then it is stored in vesicles. When parasympathetic nerve is stimulated, the action potential induces calcium influx into the neuron, and calcium mediates release of the neurotransmitter by a process called exocytosis. During exocytosis, the vesicle membrane and plasma membrane fuse, and the neurotransmitter is released into the synapse through an opening in the fused membranes. After acetylcholine activates postsynaptic acetylcholine receptors, it is rapidly hydrolyzed by the enzyme cholinesterase to form choline and acetate. Choline is recycled through the process of reuptake by the presynaptic neuron. This process is mediated by a membrane protein that transports choline into the neuron. Acetylcholine can also activate presynaptic autoreceptors, which inhibits further release of the neurotransmitter by the neuron.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


