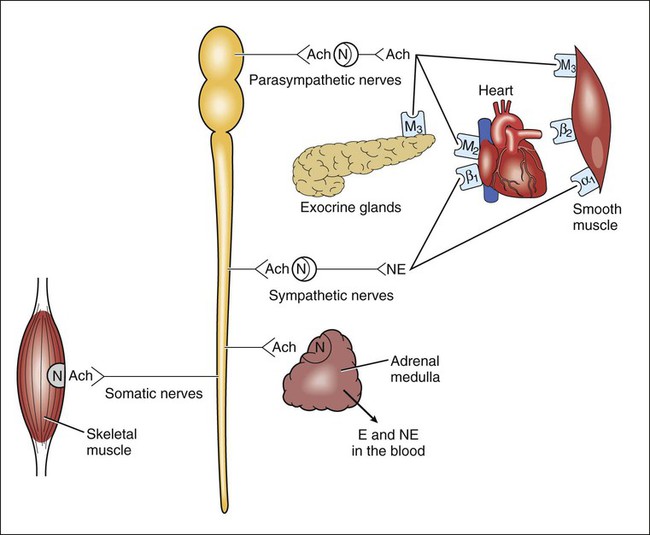
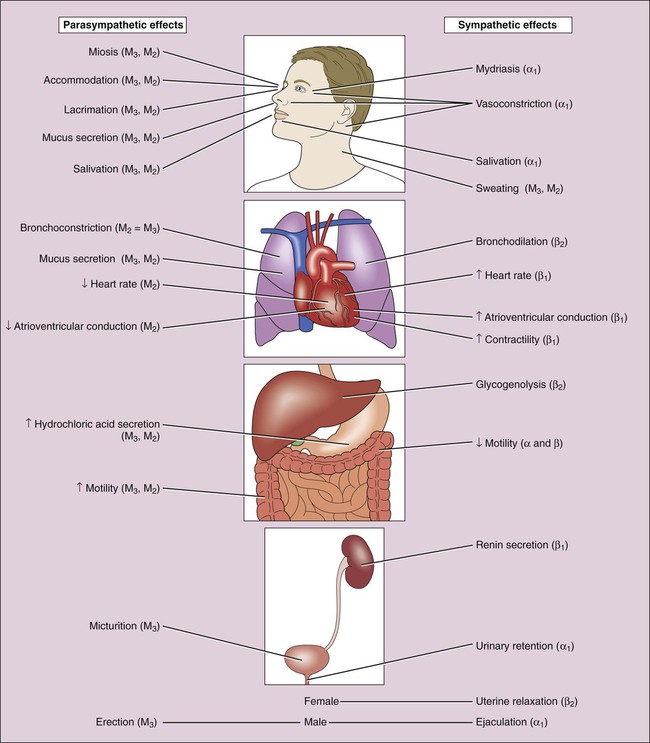
The origins, neurotransmitters, and receptors of the sympathetic and parasympathetic systems are shown in Figure 5-1. The sympathetic nervous system tends to discharge as a unit, producing a diffuse activation of target organs. Preganglionic, sympathetic neurons synapse with a large number of postganglionic neurons, which contributes to widespread activation of the organs during sympathetic stimulation. In addition, the release of epinephrine and norepinephrine from the adrenal medulla into the circulation enables the activation of target tissues throughout the body, including some tissues not directly innervated by sympathetic nerves. In contrast, the parasympathetic system can discretely activate specific target tissues. For example, it is possible for parasympathetic nerves to slow the heart rate without simultaneously stimulating gastrointestinal or bladder function. This is partly because of the low ratio of postganglionic fibers to preganglionic fibers in the parasympathetic system. As shown in Figure 5-2, the sympathetic and parasympathetic nervous systems often have opposing effects on organ function. Activation of the sympathetic system produces the “fight or flight” reaction in response to threatening situations. In this reaction, cardiovascular stimulation provides muscles with oxygen and fuels required to support vigorous physical activity, while activation of glycogenolysis and lipolysis releases the necessary energy substrates. The parasympathetic system is sometimes called the “rest and digest” system, because it slows the heart rate and promotes more vegetative functions, such as digestion, defecation, and micturition. Many parasympathetic effects (including pupillary constriction, bronchoconstriction, and stimulation of gut and bladder motility) are caused by smooth muscle contraction. The primary neurotransmitters found in the autonomic and somatic nervous systems are acetylcholine and norepinephrine (see Fig. 5-1). The terms adrenergic and cholinergic refer to neurons that release norepinephrine or acetylcholine, respectively. A number of other neurotransmitters have been identified in autonomic nerves of the ENS of the gastrointestinal tract, as well as in the genitourinary tract and certain blood vessels. The transmitters released by these neurons include neuropeptide Y, vasoactive intestinal polypeptide, enkephalin, substance P, serotonin (5-hydroxytryptamine), adenosine triphosphate, and nitric oxide. In some tissues, adenosine triphosphate released by these neurons is converted to adenosine, which can then activate adenosine receptors in a number of tissues (see Chapter 27). Nitric oxide is an important neurotransmitter that produces vasodilatation in many vascular beds and is also found in the ENS.
Introduction to Autonomic and Neuromuscular Pharmacology
Anatomy and Physiology of the Peripheral Nervous System
Autonomic Nervous System
Neurotransmitters and Receptors
Neurotransmitters
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree