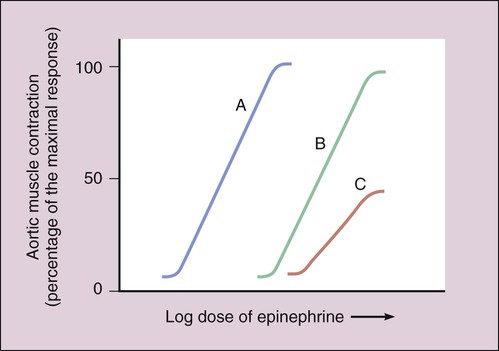
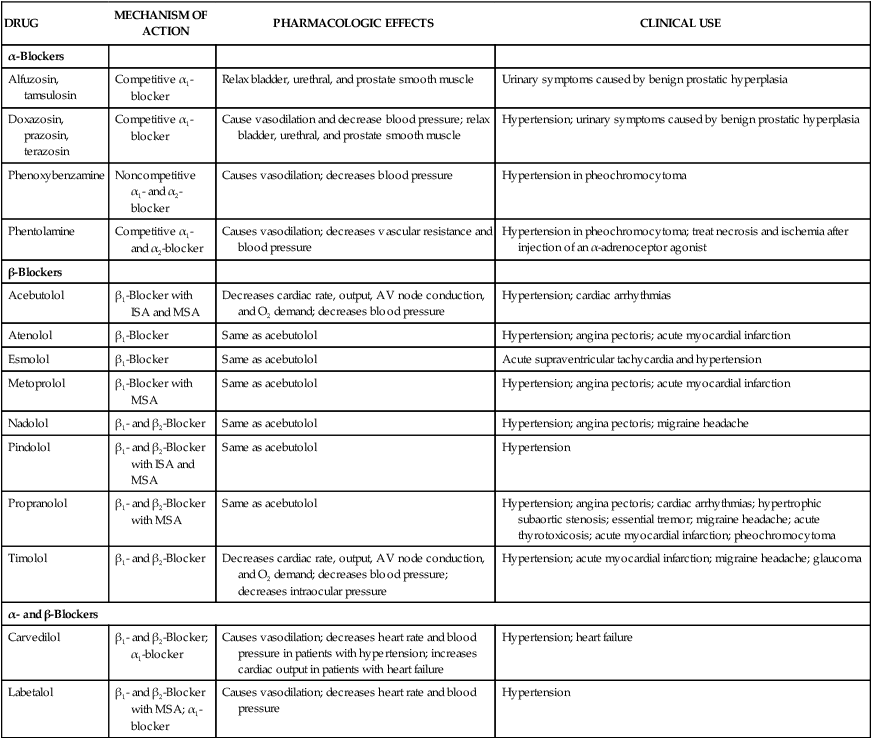
Excessive sympathetic nervous system activity contributes to a number of diseases, including common cardiovascular disorders such as hypertension, angina pectoris, and cardiac arrhythmias. Drugs that reduce sympathetic stimulation, sympatholytic drugs, are used in the management of cardiovascular diseases and other diseases such as glaucoma, migraine headache, and urinary obstruction. The adrenoceptor antagonists are the most important group of sympatholytic drugs used today. The sympathetic neuronal blocking agents discussed in Chapter 5 also have a sympatholytic effect but are largely obsolescent. Phenoxybenzamine is administered orally and undergoes nonenzymatic chemical transformation to an active metabolite that forms a long-lasting covalent bond with α-adrenoceptors, resulting in noncompetitive receptor blockade (Fig. 9-1). The drug exhibits a slow onset of action owing to the time required to form its active metabolite, but it has a long duration of action of 3 to 4 days because of its stable drug-receptor binding. Phenoxybenzamine decreases vascular resistance and lowers both supine and standing blood pressure. As shown in Table 9-1, phenoxybenzamine is used to treat hypertensive episodes in patients with pheochromocytoma, which is a tumor of the adrenal medulla that secretes huge amounts of catecholamines, causing extremely high blood pressure. In this setting, phenoxybenzamine is used to control hypertension until surgery can be performed to remove the tumor (Box 9-1). TABLE 9-1 Mechanisms, Pharmacologic Effects, and Clinical Uses of Selected Adrenoceptor Antagonists
Adrenoceptor Antagonists
Overview
α-Adrenoceptor Antagonists
Nonselective α-Blockers
Phenoxybenzamine
Pharmacokinetics and Mechanism of Action
Effects and Indications
DRUG
MECHANISM OF ACTION
PHARMACOLOGIC EFFECTS
CLINICAL USE
α-Blockers
Alfuzosin, tamsulosin
Competitive α1-blocker
Relax bladder, urethral, and prostate smooth muscle
Urinary symptoms caused by benign prostatic hyperplasia
Doxazosin, prazosin, terazosin
Competitive α1-blocker
Cause vasodilation and decrease blood pressure; relax bladder, urethral, and prostate smooth muscle
Hypertension; urinary symptoms caused by benign prostatic hyperplasia
Phenoxybenzamine
Noncompetitive α1– and α2-blocker
Causes vasodilation; decreases blood pressure
Hypertension in pheochromocytoma
Phentolamine
Competitive α1– and α2-blocker
Causes vasodilation; decreases vascular resistance and blood pressure
Hypertension in pheochromocytoma; treat necrosis and ischemia after injection of an α-adrenoceptor agonist
β-Blockers
Acebutolol
β1-Blocker with ISA and MSA
Decreases cardiac rate, output, AV node conduction, and O2 demand; decreases blood pressure
Hypertension; cardiac arrhythmias
Atenolol
β1-Blocker
Same as acebutolol
Hypertension; angina pectoris; acute myocardial infarction
Esmolol
β1-Blocker
Same as acebutolol
Acute supraventricular tachycardia and hypertension
Metoprolol
β1-Blocker with MSA
Same as acebutolol
Hypertension; angina pectoris; acute myocardial infarction
Nadolol
β1– and β2-Blocker
Same as acebutolol
Hypertension; angina pectoris; migraine headache
Pindolol
β1– and β2-Blocker with ISA and MSA
Same as acebutolol
Hypertension
Propranolol
β1– and β2-Blocker with MSA
Same as acebutolol
Hypertension; angina pectoris; cardiac arrhythmias; hypertrophic subaortic stenosis; essential tremor; migraine headache; acute thyrotoxicosis; acute myocardial infarction; pheochromocytoma
Timolol
β1– and β2-Blocker
Decreases cardiac rate, output, AV node conduction, and O2 demand; decreases blood pressure; decreases intraocular pressure
Hypertension; acute myocardial infarction; migraine headache; glaucoma
α- and β-Blockers
Carvedilol
β1– and β2-Blocker; α1-blocker
Causes vasodilation; decreases heart rate and blood pressure in patients with hypertension; increases cardiac output in patients with heart failure
Hypertension; heart failure
Labetalol
β1– and β2-Blocker with MSA; α1-blocker
Causes vasodilation; decreases heart rate and blood pressure
Hypertension
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Adrenoceptor Antagonists
Only gold members can continue reading. Log In or Register to continue