Fig. 31.1
Frozen section of a renal angiomyolipoma mimicking oncocytic renal cell neoplasms. Original magnification × 200
An incisional biopsy of a renal lesion may be submitted for intraoperative consultation when the diagnosis may result in changes in the treatment procedure (e.g., partial nephrectomy for a benign condition vs. radical nephrectomy for a RCC). In this setting, the entire biopsy specimen should be embedded for frozen section assessment (FSA) , and multiple levels should be prepared if the diagnosis is in doubt.
During radical nephrectomy, there are usually no immediate management issues at stake. If the surgeon requests an intraoperative consultation, gross examination is often all that is necessary. If the macroscopic findings are equivocal (e.g., cystic RCC vs. complex benign cyst with secondary hemorrhage and fibrosis; see below), it is best to defer the diagnosis to permanent sections instead of performing multiple FSAs to seek for a definitive diagnosis. On frozen section, it can be very difficult to render a definitive histologic diagnosis for a renal neoplasm with prominent clear cells (Fig. 31.2) or papillary growth pattern. Similarly, renal oncocytomas often show characteristic gross findings (i.e., well circumscribed, unencapsulated, mahogany brown, and no necrosis). However, the gross diagnosis of oncocytoma should be provisional. Even when a FSA is performed, clear cell RCC with prominent granular cells and eosinophilic variant of chromophobe RCC can have prominent oncocytic features mimicking oncocytoma.
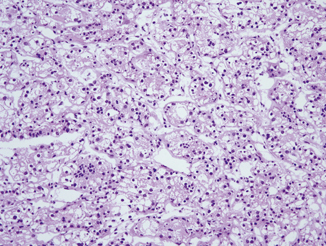
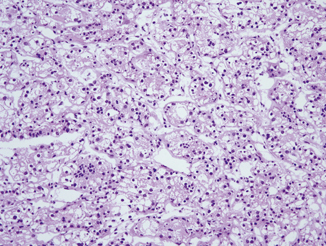
Fig. 31.2
Frozen section of a clear cell renal cell carcinoma which can be mistaken for a chromophobe renal cell carcinoma. Original magnification × 100
FSA during radical nephrectomy can be justified in certain situations, including a possibility that the neoplasm is a high-grade urothelial carcinoma forming a mass and thus mimicking a RCC; it is important to make this distinction because the surgeon will proceed with converting the surgical procedure to a nephroureterectomy if a diagnosis of urothelial carcinoma is rendered. Even though the value of an extended lymphadenectomy remains controversial, some surgeons may choose to perform an extended lymph node dissection when the RCC is of high grade or if there are other poor prognostic features, such as a sarcomatoid component. For a RCC, if grading is requested, the surgeon should be informed that there is a possibility of undergrading because of tumor heterogeneity as well as the limitations of FSA that make it difficult to precisely determine the nuclear size and/or presence of prominent nucleoli. Multiple selective sections from different areas of the tumor may be helpful in this setting.
Assessment of Cystic Renal Masses
Up to 15 % of renal tumors are predominantly cystic. Cystic change can easily be recognized on imaging and is often graded using the Bosniak classification that helps to determine malignant risk of renal cysts on the basis of their appearance and enhancement on computed tomography [1]. Treatment varies, and the surgeon may request a FSA to guide the extent of resection particularly when renal parenchymal sparing is of critical importance.
The specimen submitted for FSA is often a wedge biopsy of the cyst wall. The entire specimen should be embedded for FSA. The differential diagnosis includes a simple cyst with superimposing hemorrhage and/or infection, cystic nephroma/mixed stromal and epithelial tumor of the kidney, and RCC with marked cystic change .
Assessment of Surgical Margins During Partial Nephrectomy
Partial nephrectomy recently has become the preferred treatment for all stages of T1a RCCs and some T1b tumors [2, 3]. It provides not only adequate long-term oncologic outcomes, when comparing with radical nephrectomy [2, 4], but also preservation of renal function. This procedure is particularly indicated for patients with: (1) a solitary kidney; (2) bilateral kidney disease; (3) a genetic predisposition to multiple synchronous or metachronous tumors such as von Hippel–Lindau disease, tuberous sclerosis, hereditary papillary renal carcinoma syndrome, and Birt–Hogg–Dubé syndrome; and (4) benign renal tumor such as angiomyolipoma, cystic nephroma, or mixed epithelial and stromal tumor of the kidney.
The partial nephrectomy specimen is often submitted for evaluation of its surgical margins. Two types of specimens are submitted for FSA to assess surgical margins: an entire partial nephrectomy specimen and a biopsy of the tumor bed. In general, a 1-cm margin of normal tissue is optimal for RCC, but narrower yet negative margins do not appear to affect patient outcomes. It has also been shown that positive surgical margins in partial nephrectomy specimens may not be clinically significant, and patients with positive margin do not commonly seem to develop long-term recurrence [5, 6]. Benign neoplasms can be excised with very narrow margins. In a recent study by one of the authors comparing partial nephrectomy cases with ( n = 293) versus without ( n = 140) intraoperative consultation, the FSA was shown to significantly reduce the incidence of positive margins from 17.0 to 4.3 % ( P< 0.001) yet failed to affect recurrence-free survival overall [7]. Nonetheless, this study suggested the usefulness of FSA in select patients because FSA was associated with improved survival in those who had pT1 or exophytic tumors and underwent laparoscopic partial nephrectomy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


