Chapter 47 Inhibitors of Bacterial Ribosomal Actions
| Abbreviations | |
|---|---|
| AIDS | Acquired immunodeficiency syndrome |
| CSF | Cerebrospinal fluid |
| GI | Gastrointestinal |
| IM | Intramuscular |
| IV | Intravenous |
| MIC | Minimal inhibitory concentration |
| MLSB | Macrolide-lincosamide-streptogramin B |
| mRNA | Messenger ribonucleic acid |
| MRSA | Methicillin-resistant Staphylococcus aureus |
| tRNA | Transfer ribonucleic acid |
| VRE | Vancomycin-resistant enterococci |
Therapeutic Overview
The ribosome-binding sites for macrolides such as erythromycin, azithromycin, clarithromycin, and clindamycin are on the same 50S subunit (S represents the sedimentation parameter), but the structures of the drugs and the spectrum of activities differ considerably. Erythromycin, one of the first macrolides developed, is relatively safe and widely used, especially for the treatment of infections in children (Box 47-1). Because of the success of macrolides in the treatment of pulmonary infections, these drugs continue to be used in the treatment of respiratory tract infections in adults. The primary differences among erythromycin, clarithromycin, and azithromycin are related to relative activities against certain bacterial species such as Mycobacterium, gastrointestinal (GI) tolerability, and pharmacokinetics. Clindamycin displays antimicrobial activity somewhat similar to that
of erythromycin. However, the two differ structurally, and clindamycin displays extensive anaerobic activity while having no activity for atypical respiratory pathogens.
The tetracyclines and synthetic glycylcycline analogs bind to the 30S ribosomal subunit and are effective against aerobic and anaerobic gram-positive and gram-negative organisms. Given their wide spectrum of activity, these agents remain widely used for treatment of bacterial, chlamydial, rickettsial, and mycoplasmal infections, although the development of bacterial resistance has reduced their efficacy against some pathogens (Box 47-2).
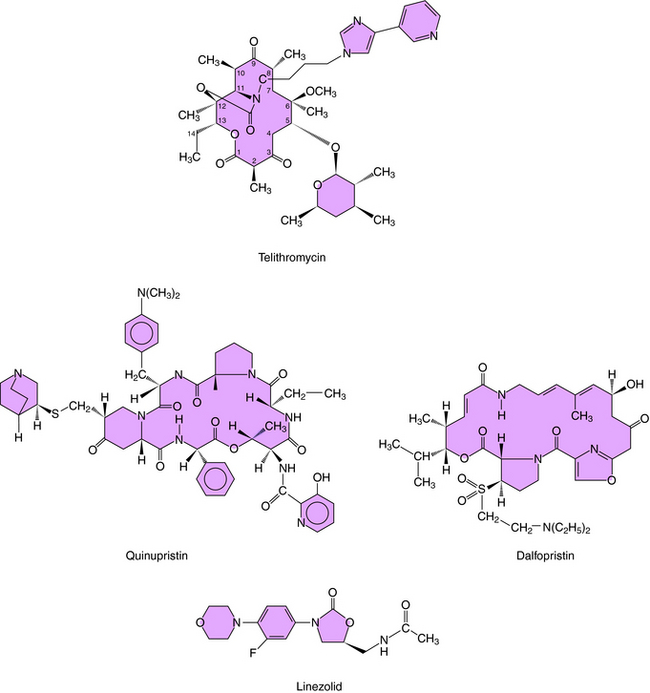
The streptogramins and oxazolidinones are newer classes of antibiotics that were developed primarily for the treatment of gram-positive organisms and often have activity against organisms that are resistant to β-lactams and glycopeptides. Both classes inhibit protein synthesis, but their structures and mechanisms of action differ.
| Therapeutic Overview |
|---|
| Aminoglycosides |
| Inhibit gram-negative aerobes |
| Narrow therapeutic index |
| Renal and otic toxicities can be serious |
| Pharmacokinetics are important considerations |
| Plasmid-mediated resistance is a problem |
| Macrolides |
| Inhibit Mycoplasma, Chlamydia, Legionella |
| Inhibit gram-positive organisms |
| Clindamycin |
| Inhibits gram-positive cocci and anaerobic species |
| Active against clostridium difficile-associated diarrhea and colitis |
| Chloramphenicol |
| Kills major meningitis pathogens |
| Serious toxicity |
| Ketolides |
| Inhibit respiratory pathogens |
| Active against penicillin and macrolide-resistant S. pneumoniae |
| Tetracyclines |
| Inhibit broad spectrum of organisms |
| Streptogramins |
| Inhibit gram-positive organisms |
| Active against VRE |
| Oxazolidinones |
| Inhibit gram-positive organisms |
| Active against VRE |
These drugs represent important agents for the treatment of multidrug-resistant gram-positive infections, but prudent use will be important to prevent the development of resistance to these agents.
Mechanisms of Action
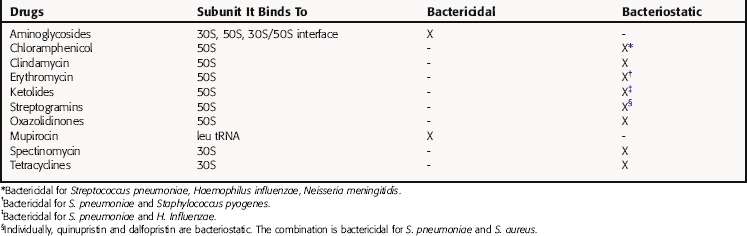
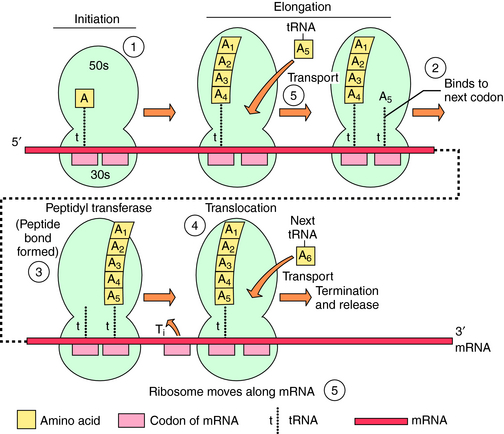
The bacterial ribosomal subunit to which each of these drugs binds and the bactericidal or bacteriostatic response of susceptible bacteria to the drugs are in Table 47-1. The principal steps in bacterial ribosomal synthesis of proteins, as carried out by the 70S ribosomes and relevant RNAs, and the points at which the drugs act, are depicted in Figure 47-1.
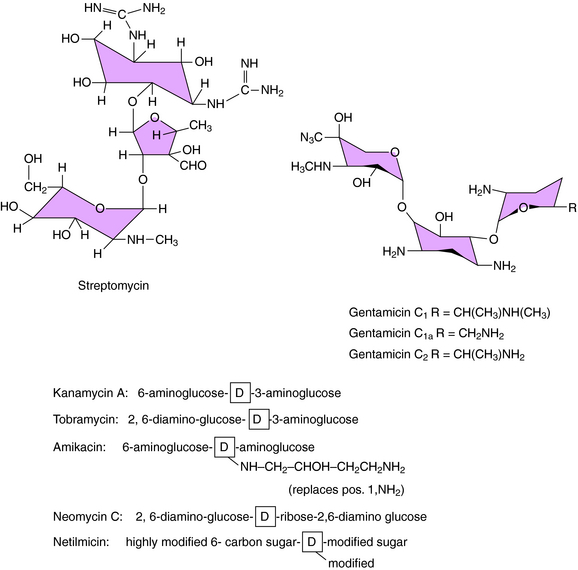
Aminoglycosides consist of amino sugars linked through glycosidic bonds to an aminocyclitol. The structures of streptomycin, gentamicin, and other clinically important aminoglycosides are shown in Figure 47-2. The particular amino sugars and specific locations of the amino groups distinguish the compounds and are important for their antimicrobial effects and toxicity. Gentamicin consists of a mixture of three species with little differences in activities.
The aminoglycosides can cross the complex cell membrane structure of gram-negative bacteria (see Fig. 46-3) and are more effective against aerobic gram-negative than gram-positive bacteria.
Binding to the ribosome leads to inhibition of protein synthesis. This takes place on the ribosomes, where messenger RNA (mRNA) acts as a template for the addition of activated amino acids attached to tRNAs. The 70S ribosomal particles move along the mRNA template, adding the appropriate amino acid (see Fig. 47-1). Aminoglycosides bind to several ribosomal sites (see Table 47-1) of the 30S and 50S subunits of the bacterial ribosome. Streptomycin, the most thoroughly studied, binds to the 30S subunit, although this can be altered by mutation of particular amino acids. Binding of aminoglycosides interferes with protein synthesis in two ways:
Bacterial resistance to aminoglycosides results from:
Clinically, enzymatic modification of the aminoglycosides is the most important mechanism of resistance. Although resistance resulting from altered ribosomes does occur in enterococci, it is rarely seen in gram-negative bacteria and is relatively uncommon. Resistance as a consequence of the inadequate transport of drug across the cytoplasmic membrane is uncommon in aerobic or facultative species but is seen in strict anaerobes. Mutants with alterations in the electron transfer chain and in adenosine triphosphatase activity have been identified, but they are very rare. The resistance of some Pseudomonas species to aminoglycosides may be related to failure of the drug to distort the lipopolysaccharide of the outer membrane, thus not allowing drug to enter the bacterial cell.
Macrolides, Chloramphenicol, and Clindamycin
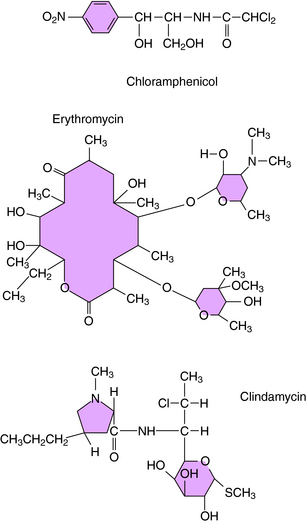
The macrolides (erythromycin, clarithromycin, azithromycin, and dirithromycin), chloramphenicol, and clindamycin are discussed as a group because these agents bind to the same site or sites on the ribosomal 50S subunit. They bind to bacterial 70S ribosomes but not to the 80S ribosomes of mammalian cells. Their structures are shown in Figure 47-3. Bacterial resistance is observed for all of these agents.
Erythromycin and the newer macrolides reversibly bind to 50S ribosomal subunits, causing dissociation of peptidyl-tRNA from the ribosome and interference with peptide elongation. Erythromycin inhibits the binding of chloramphenicol to 50S ribosomes, but chloramphenicol does not inhibit erythromycin binding. The activity of macrolides is primarily bacteriostatic; however, bactericidal activity is observed for certain organisms (see Table 47-1).
Bacterial resistance to macrolides occurs by several mechanisms, some of which also confer resistance to clindamycin and streptogramin type B. The most problematic forms of resistance arise either from alteration of ribosomal binding sites or drug efflux. Alteration of ribosomal binding sites occurs via a plasmid-encoded enzyme that methylates the 50S ribosomal subunit. Methylation likely causes a conformational change of the ribosomal target and decreased binding. This type of resistance is associated with the erm (erythromycin ribosome methylation) gene and is referred to as the macrolide-lincosamide-streptogramin B (MLSB) phenotype, because it confers resistance to macrolides, clindamycin, and streptogramin B. Both erythromycin and clindamycin induce this enzyme, but erythromycin has greater activity. This is clinically important, because an organism resistant to erythromycin and susceptible to clindamycin can become resistant to both drugs during therapy. This applies to the treatment of infections caused by methicillin-resistant Staphylococcus aureus (MRSA), which is often resistant to erythromycin but may appear susceptible to clindamycin. This form of resistance is present on plasmids that can pass from enterococci to streptococci and is encountered in strains of macrolide-resistant Streptococcus pneumoniae and Streptococcus pyogenes.
The ketolides are semisynthetic derivatives of erythromycin and are part of the MLSB family of antimicrobials. The currently approved ketolide is telithromycin; its structure is shown in Figure 47-4. Similar to the macrolides, ketolides inhibit protein synthesis at the 50S ribosomal subunit. However, ketolides demonstrate a higher binding affinity. Ketolides are primarily bacteriostatic but demonstrate bactericidal activity against some pathogens, including S. pneumoniae and H. influenzae.
Tetracyclines and Glycylcyclines
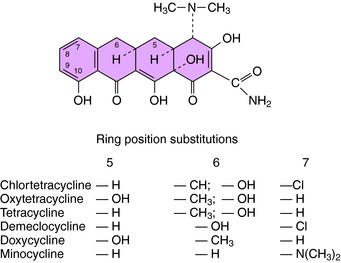
The structures of the tetracyclines are shown in Figure 47-5. These compounds bind to 30S ribosomes, thereby preventing attachment of the aminoacyl-tRNA to its acceptor site and preventing the addition of amino acids to the peptide chain being synthesized. Differences in the activities of individual tetracyclines are related to their solubility in lipid membranes of the bacteria. These drugs enter the cytoplasm of gram-positive bacteria by an energy-dependent process, but in gram-negative organisms, they pass through the outer membrane by diffusion through porins. Because minocycline and doxycycline are more lipophilic, they can enter gram-negative cells through the outer lipid membrane and through the porins. Once in the periplasmic space, the tetracyclines are transported across the inner cytoplasmic membrane by a protein-carrier system.
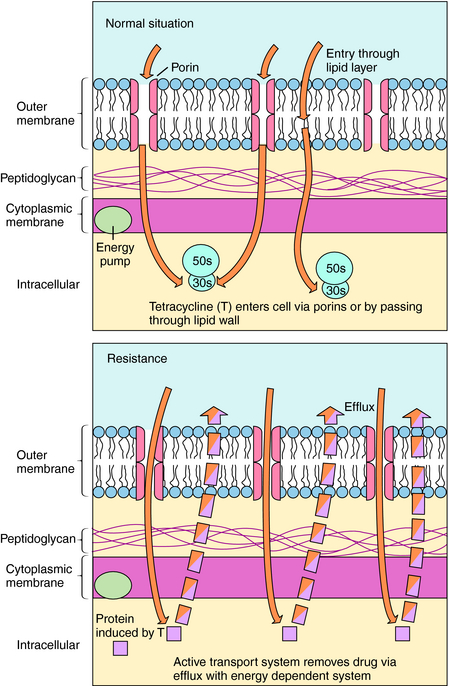
There are several mechanisms of resistance to tetracyclines. The most common, found in both gram-positive and gram-negative bacteria, is plasmid or transposon mediated and involves decreased intracellular accumulation and increased transport of the drug out of the bacterial cell (Fig. 47-6). Drug efflux occurs as a result of the action of a new protein, likely induced by the drug. A second mechanism involves alteration of outer membrane proteins resulting from mutations in chromosomal genes. In a third mechanism the ribosomal binding site is protected as a result of the presence of a plasmid-generated protein that binds to the ribosome. Resistance to one tetracycline usually implies resistance to all tetracyclines. However, some staphylococci and some Bacteroides species are resistant to tetracycline but susceptible to minocycline and doxycycline because of the lipophilicity of these latter agents.