Chapter 14 Histamine and Antihistamines
| Abbreviations | |
|---|---|
| CNS | Central nervous system |
| Epi | Epinephrine |
| IgE | Immunoglobulin E |
Therapeutic Overview
Histamine is synthesized, stored, and released primarily by mast cells and has profound effects on many organs. It is an important mediator of immediate hypersensitivity reactions and acute inflammatory responses and is a primary stimulator of gastric acid secretion. It is also an important neurotransmitter in the central nervous system (CNS) (see Chapter 27).
H1 and H2 receptors have been most widely characterized and mediate well-defined responses in humans, as summarized in Table 14-1. Most responses are mediated by H1 receptors, such as bronchoconstriction, and are selectively antagonized by classical antihistamines, more accurately described as selective H1 receptor blocking drugs such as diphenhydramine. Antihistamines are widely used to treat allergic reactions, motion sickness, and emesis and as over-the-counter sleeping aids. H2-mediated responses such as gastric acid secretion are selectively antagonized by specific H2 receptor blocking drugs such as cimetidine. The H2 receptor antagonists are discussed extensively in Chapter 18; this chapter focuses on histamine and H1 receptor antagonists.
TABLE 14–1 Histamine Receptor Subtypes Mediating Selected Responses in Humans
| Subtype | Responses |
|---|---|
| H1 receptor only | Basilar, pulmonary, coronary artery constriction; increased permeability of postcapillary venules; contraction of bronchiolar smooth muscle; stimulation of vagal sensory nerve endings promoting bronchospasm and coughing; gastrointestinal smooth muscle relaxation and contraction; Epi release from adrenal medulla |
| H2 receptor only | Acid and pepsin secretion from oxyntic mucosa; facial cutaneous vasodilation; pulmonary and carotid artery relaxation; increased rate and force of cardiac contraction; relaxation of bronchial smooth muscle; inhibition of IgE-dependent degranulation of basophils |
| H1 and H2 (?) receptors | Decreased total peripheral resistance; increased forearm blood flow; increased cardiac atrial and ventricular automaticity; stimulation of cutaneous nerve endings causing pain and itching |
Clinical uses of histamine antagonists are summarized in the Therapeutic Overview Box.
| Therapeutic Overview |
|---|
| Histamine and Histamine Receptor Agonists |
| No significant clinical use |
| Antihistamines (H1 Receptor Antagonists) |
| Allergic reactions |
| Motion sickness |
| Insomnia |
| Nausea and vomiting |
| H2 Receptor Antagonists |
| Peptic ulcers and gastroesophageal reflux disease (see Chapter 18) |
Mechanisms of Action
Synthesis and Metabolism of Histamine
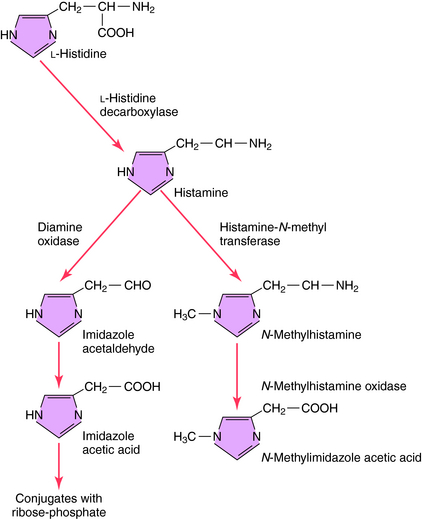
The synthesis and catabolism of histamine are depicted in Figure 14-1. Histamine is synthesized by decarboxylation of the amino acid L-histidine by histidine decarboxylase. Most histamine is stored in an inert form at its site of synthesis, and very little is freely diffusible. After synthesis and release from its storage sites, histamine acts at its targets and is rapidly metabolized through two primary pathways. Oxidative deamination leads to formation of imidazole acetic acid, while methylation, which predominates in the brain, leads to the formation of N-methylimidazole acetic acid. Both metabolites are inactive and subject to further biotransformation.
Storage and Release of Histamine by Mast Cells and Basophils
Histamine is stored and released primarily by mast cells. Although basophils and central neurons also use histamine, their role is not fully understood. Histamine is widely distributed, with the highest concentrations in the skin, lungs, and gastrointestinal tract mucosa, consistent with mast cell densities in these tissues.
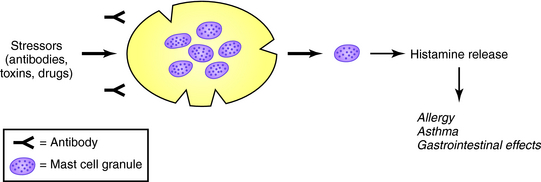
In mast cell granules, histamine exists as an ionic complex with a proteoglycan, chiefly heparin sulfate, but also chondroitin sulfate E. In basophils, histamine is also stored in granules as an ionic complex, predominantly with proteoglycans. The release of histamine and other mediators from mast cells and basophils is common during allergic reactions but also can be induced by drugs and endogenous compounds to produce pseudoallergic, anaphylactoid reactions as shown in Figure 14-2. The role of mast cells in immediate and delayed hypersensitivity reactions and nonallergic disorders explains the therapeutic utility of antihistamines and degranulation inhibitors.
A summary of agents that release histamine is presented in Table 14-2. Histamine concentrations of 0.2 to 1.0 ng/mL in humans produce mild signs and symptoms, including metallic taste, headache, and nasal congestion. Concentrations exceeding 1 ng/mL produce moderate effects, including skin reactions, cramping, diarrhea, flushing, tachycardia, cardiac dysrhythmias, and hypotension. Life-threatening hypotension, ventricular fibrillation, and bronchospasm leading to cardiopulmonary arrest can occur when concentrations approach 12 ng/mL.
TABLE 14–2 Common Causal Factors Involved in Anaphylactic and Anaphylactoid Reactions
| IgE-Mediated Anaphylaxis | Non–IgE-Mediated Anaphylactoid Reactions |
|---|---|
| Food | Drugs |
| Peanuts, seafood, eggs, milk products, grains | Anesthesia related: neuromuscular blocking agents, opioids, plasma expanders |
| Drugs | |
| Antibiotics: penicillins, cephalosporins, sulfonamides | |
| Dyes | |
| Venoms | Radiocontrast media, fluorescein |
| Hymenoptera, fire ants, snakes | |
| Other Idiopathic Reactions | |
| Foreign Proteins | |
| Nonhuman insulin, corticotropin, serum proteins, seminal proteins, vaccines, antivenoms | |
| Enzymes | |
| Chymopapain | |
| Other |