• Intermittent bouts of diarrhea, low-grade fever, and right lower quadrant pain • Anorexia, weight loss, flatulence, and malaise • Abdominal tenderness, especially right lower quadrant, with signs of peritoneal irritation and an abdominal or pelvic mass • Radiographs show abnormality of terminal ileum • Bloody diarrhea with cramps in lower abdomen • Mild abdominal tenderness, weight loss, and fever • Rectal examination may show perianal irritation, fissures, hemorrhoids, fistulas, and abscesses • Crohn’s disease (CD): lesions are a granulomatous inflammatory reaction throughout entire thickness of bowel wall. In 40% of cases, granulomas are either poorly developed or totally absent. May involve buccal mucosa, esophagus, stomach, duodenum, jejunum, ileum, and colon. Crohn’s disease of small intestine is called “regional enteritis”; colon involvement is called “Crohn’s disease of the colon” or “granulomatous colitis” (only a portion of patients develop granulomatous lesions). • Ulcerative colitis (UC): Lesions are a nonspecific inflammatory response limited to colonic mucosa and submucosa. Well-developed granuloma formation does not occur. Common features shared by Crohn’s disease and ulcerative colitis: • Colon is frequently involved in Crohn’s and invariably involved in UC. • Although rare, patients with UC and total colon involvement may develop “backwash ileitis”; both conditions may cause changes in small intestine. • Patients with CD often have close relatives with UC and vice versa. • When no granuloma in CD of the colon, the two lesions may resemble each other clinically and pathologically. • Many epidemiologic similarities exist between CD and UC: age, race, sex, and geographic distribution. • Both conditions are associated with similar extraintestinal mani-festations. • The two conditions have etiologic parallels. • Both conditions are associated with increased frequency of colonic carcinoma. • Genetic predisposition: supported by ethnic distribution of incidence and multiple members of a family having CD or UC in 15%-40% of cases. • Infectious etiology: The idea that a transmissible agent is responsible for IBD is a hotly debated subject. Viruses (rotavirus, Epstein–Barr virus, cytomegalovirus, and an uncharacterized RNA intestinal cytopathic virus) and mycobacteria continue to be favored candidates. Gastrointestinal (GI) infections with Aeromonas bacteria (A. sobria and A. hydrophila) and Candida albicans can initiate and perpetuate colitis. Test all IBD patients for these infections at start of and during course of illness. Other candidates include pseudomonas-like organisms, enteric anaerobes, Chlamydia, and Yersinia enterocolitica. • Antibiotic exposure: before the 1950s, CD was found in selected groups with strong genetic component. Since then, a rapid increase has occurred in developed countries and countries that previously had virtually no reported cases. CD has spread like epidemic. Wherever antibiotics are used early and in large quantities, the incidence of CD is now quite high. An infectious agent may be a normal intestinal flora suddenly producing immunostimulatory toxins or becoming invasive by sublethal doses of antibiotics that induce flora to become stronger in virility and numbers and more capable of producing toxins. Immunologic derangements are found in IBD, but whether causal of IBD or secondary to it remains unclear. Current evidence indicates that derangements are secondary to disease process. — CD is increasing in cultures consuming a Western diet. It is virtually nonexistent in cultures consuming a primitive diet. People who have CD habitually eat more refined sugar and less raw fruit and vegetables and dietary fiber than do healthy people (122 g sugar daily vs. 65 g daily). Corn flakes have been linked to CD; they are high in refined carbohydrates and derived from common allergen (corn). — UC is not linked to refined carbohydrates. Food allergy is overlooked by conventional medicine. — Reduced intake of omega-3 oils and increased intake of omega-6 oils are linked to growing rise of CD in Japan. Genetics of the Japanese are relatively homogenous; therefore the increased incidence is from incorporation of Western foods. CD is strongly correlated with increased dietary total fat, animal fat, omega-6 fatty acids, animal protein, milk protein, and ratio of omega-6 to omega-3 fatty acids. CD is less correlated with total protein and not correlated with fish protein. CD is inversely correlated with vegetable protein. Increased animal protein is the strongest independent factor followed by increased ratio of omega-6 to omega-3 fatty acids. • Miscellaneous factors: Mental and emotional stress can promote exacerbation of IBD. Thus stress management techniques may prove useful for some patients. • Natural history of Crohn’s disease: Many patients undergo spontaneous remission, 20% at 1 year and 12% at 2 years. “Success” of placebo therapy rises dramatically. In patients having no history of steroid therapy, 41% remitted after 17 weeks; 23% of this group continued in remission after 2 years compared with 4% of group with history of steroid use. Once remission is achieved, 75% of patients continue in remission at the end of 1 year and up to 63% by 2 years, regardless of maintenance therapy used. The key is achieving remission, which, once attained, can be maintained by conservative nondrug therapy. • Eicosanoid metabolism: Prostaglandins are greatly increased in colonic mucosa, serum, and stools of IBD patients. Increased synthesis of lipoxygenase products, leukotrienes, and mono hydroxy-eicosatetraenoic acid by neutrophils amplifies inflammation and causes smooth muscle contraction. Release of lipoxygenase products is promoted by activation of alternative complement pathway. Sulfasalazine inhibits cyclooxygenase and neutrophil lipoxygenase and inhibits degranulation of mast cells. Corticosteroids inhibit phospholipase A2, blocking release of arachidonic acid from membrane phospholipids. Natural flavonoid quercetin interacts with these enzymes. Formation of inflammatory compounds is decreased by reducing dietary meat and dairy while increasing omega-3 fatty acids (small wild cold-water ocean fish), containing eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). Fish oil supplements (2.7-5.1 g total omega-3 oils daily) prevent or delay relapses in CD and UC. Flaxseed oil, which contains alpha-linolenic acid (LNA), the essential omega-3 fatty acid that the body can convert to EPA, also is of value. • Mucin defects in ulcerative colitis: Mucins are high-molecular-weight, carbohydrate-rich glycoproteins responsible for viscous/elastic characteristics of secreted mucus. Alterations in mucin composition and content in colonic mucosa is noted in UC. Factors include a dramatic decrease in mucous content of goblet cells (proportional to severity of disease) and decrease in major sulfomucin subfraction. These abnormalities are not found in CD. Mucin content of goblet cells returns to normal during remission but sulfomucin deficiency does not. Specific components of sulfomucin and the cause of its lower level are unknown. Mucin abnormalities are a major factor in increased risk of colon cancer in these patients. Many herbs effectively used to treat UC are demulcents, agents that soothe irritated mucous membranes and promote secretion of mucus. • Intestinal microflora (Textbook, “Bacterial Overgrowth of the Small Intestine” and “Comprehensive Digestive Stool Analysis”): include 400 distinct species. Fecal flora of patients with IBD contain higher numbers of gram-positive anaerobic coccoid rods and Bacteroides vulgatus, a gram-negative rod. These alterations in fecal flora are not from disease. Alterations in metabolic activity of bacteria are more important than alterations in number of bacteria. Specific bacterial cell components may promote lymphocyte cytotoxic activity against colonic epithelial cells. • Carrageenans: sulfated polymers of galactose and d-anhydrogalactose extracted from red seaweeds (Eucheuma spinosum or Chondrus crispus) have been used to induce IBD in animals. They are used by the food industry as stabilizing and suspending agents (ice cream, cottage cheese, milk chocolate, etc.) because of their ability to stabilize milk proteins. No correlation has been proven between human consumption of carrageenan and development of UC. Differences in intestinal bacterial flora probably are responsible for discrepancy: germ-free animals do not display carrageenan-induced damage. A bacterium linked to facilitating carrageenan-induced damage in animals is a strain of Bacteroides vulgatus found in much higher concentrations (six times as high) in fecal cultures of patients with IBD. Carrageenan is metabolized into nondamaging components in most human beings, but people with overgrowth of Bacteroides vulgatus may be at risk. Avoid carrageenan. • Aspirin and intestinal permeability: first-degree relatives of CD patients had a 110% increase in intestinal permeability after acetylsalicylic acid (ASA) compared with an increase of 57% in control subjects. Thirty-five percent were hyperresponders. Familial permeability defect is a significant predisposing factor for CD because leaky gut is linked to increased incidence of food allergy and absorption of intestinal toxins (Textbook, “Food Allergy”). • Endotoxemia and alternative complement pathway: endotoxemia is linked to CD and UC. Endotoxemia-induced activation of alternative complement pathway could explain extra-GI manifestations of IBD. Whole-gut irrigation significantly reduces endotoxin pool in the gut and has a beneficial antiendotoxinemia effect. Colonic irrigation may offer similar benefit. Colon irrigation during acute inflammatory flare is contraindicated. • Arthritis: the more common form is peripheral arthritis that affects knees, ankles, and wrists. Arthritis is more common in patients with colon involvement. Severity of symptoms is proportional to disease activity. Arthritis may primarily affect the spine, with low back pain and stiffness, and eventual limitation of motion. This EIL occurs mainly in men with HLA-B27 and resembles ankylosing spondylitis. It may antedate bowel symptoms by several years. A consistent underlying factor in progression of ankylosing spondylitis and IBD is likely. • Skin manifestations: seen in 15% of patients. Lesions include erythema nodosum, pyoderma gangrenosum, and aphthous ulcerations. Recurrent aphthous stomatitis occurs in 10% of patients. • Liver: serious liver disease (sclerosing cholangitis, chronic active hepatitis, cirrhosis) affects 3%-7% of patients with IBD from increased endotoxin load. Liver enzyme abnormalities indicate need for hepatoprotection from Glycyrrhiza glabra (licorice), Silybum marianum (milk thistle), catechin, and curcumin. • Other common EILs: thrombophlebitis; finger clubbing; ocular manifestations (episcleritis, iritis, and uveitis); nephrolithiasis; cholelithiasis; and, in children, failure to grow, thrive, andmature normally. Corticosteroids are known to do the following: • Stimulate protein catabolism • Decrease the absorption of calcium and phosphorus • Increase the urinary excretion of ascorbic acid, calcium, potassium, and zinc • Increase blood glucose, serum triglycerides, and serum choles-terol • Increase the requirements for vitamin B6, ascorbic acid, folate, and vitamin D
Inflammatory Bowel Disease
DIAGNOSTIC SUMMARY
GENERAL CONSIDERATIONS
Definition
Etiology
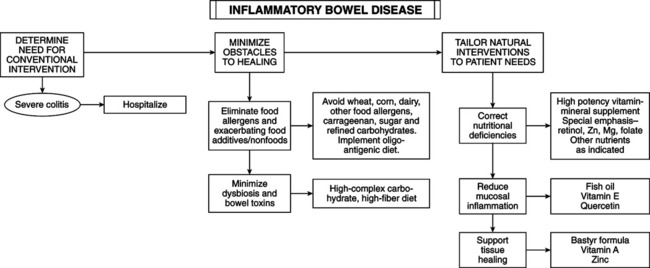
THERAPEUTIC CONSIDERATIONS
Control of Causative Factors
Extra-gastrointestinal Manifestations
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Basicmedical Key
Fastest Basicmedical Insight Engine
