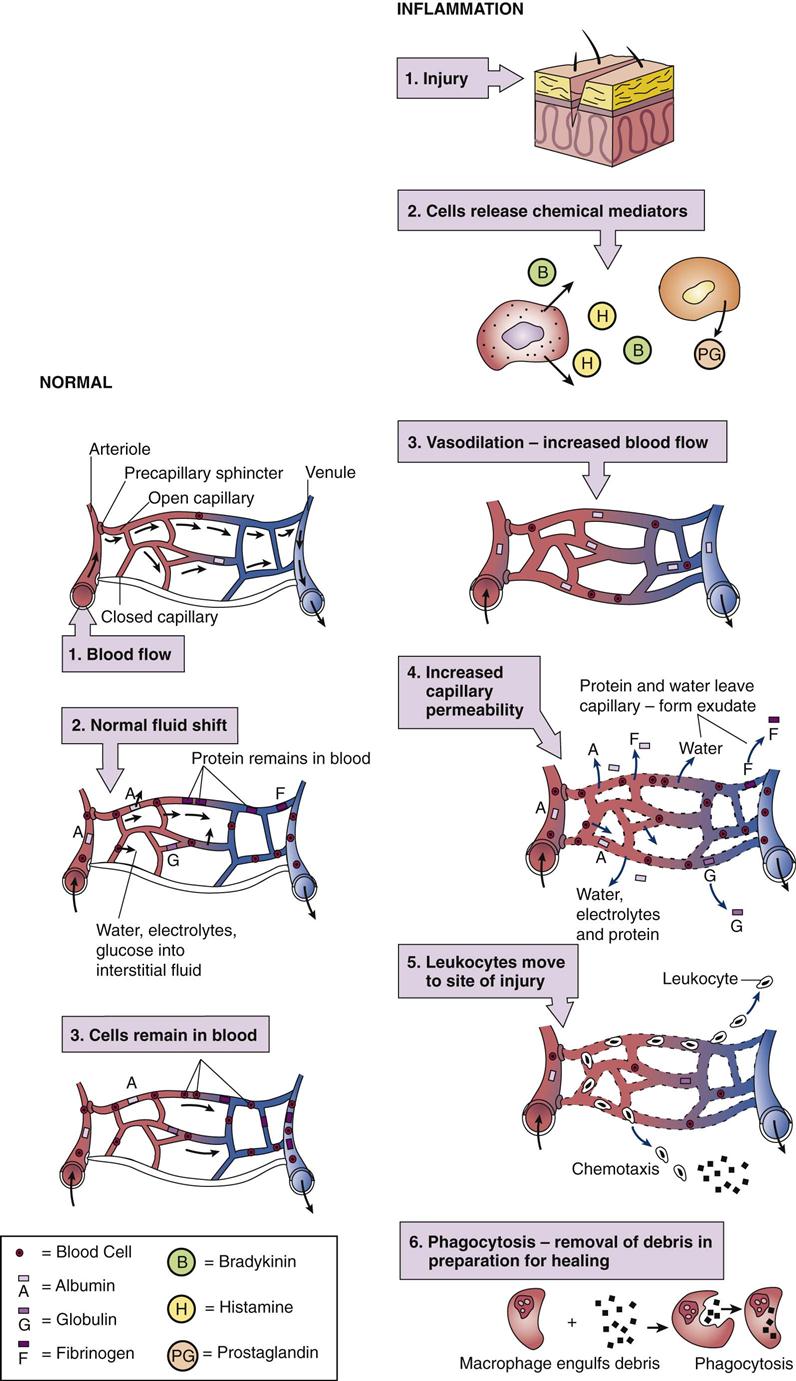
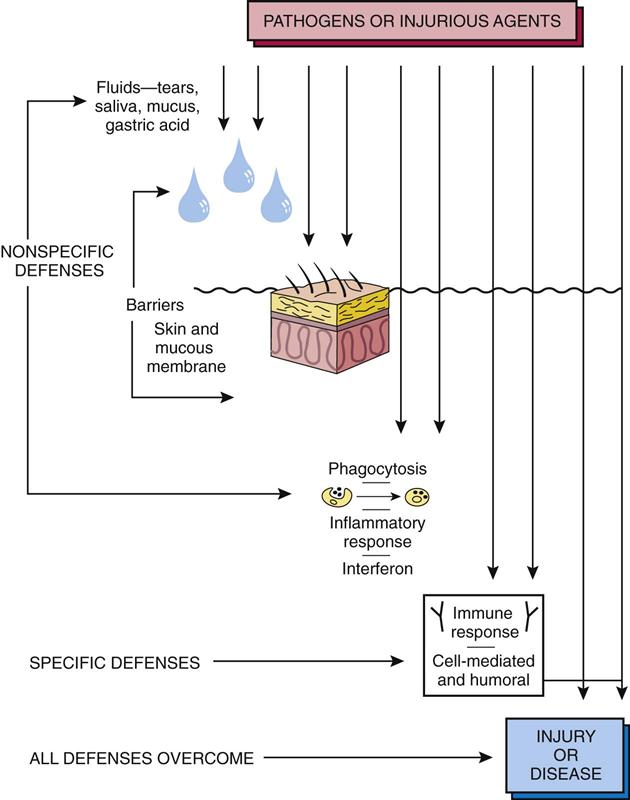
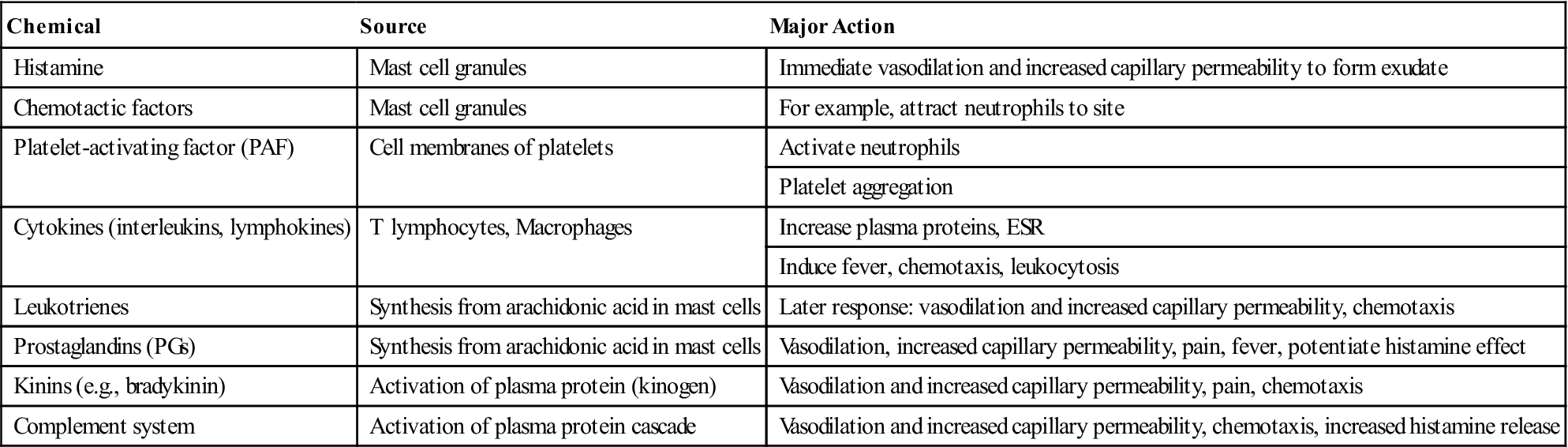
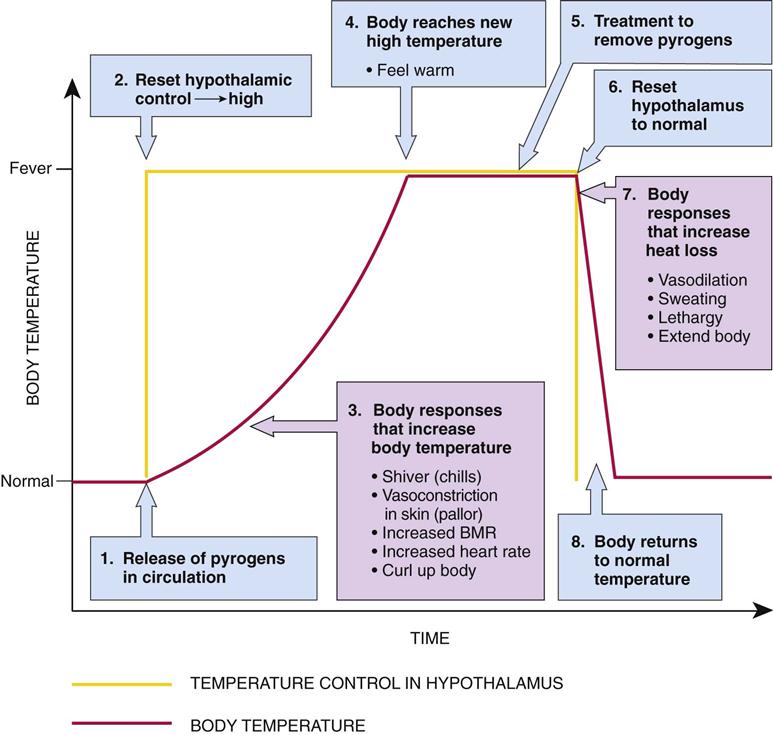
After studying this chapter, the student is expected to: 1. Explain the role of normal defenses in preventing disease. 2. Describe how changes in capillary exchange affect the tissues and the blood components. 3. Compare normal capillary exchange with exchange during the inflammatory response. 4. Describe the local and systemic effects of inflammation. 5. Explain the effects of chronic inflammation. 6. Discuss the modes of treatment of inflammation. 7. Describe the types of healing and the disadvantages of each. 8. List the factors, including a specific example for each, that hasten healing. 9. Identify the classifications of burns and describe the effects of burns. 10. Describe the possible complications occurring in the first few days after a burn. 11. Explain three reasons why the healing of a burn may be difficult. abscess adhesions angiogenesis anorexia chemical mediators chemotaxis collagen contracture diapedesis erythrocyte sedimentation rate (ESR) exudate fibrinogen fibrinous fibroblast glucocorticoids granulation tissue granuloma hematocrit hematopoiesis hydrostatic pressure hyperemia interferons intra-articular isoenzymes leukocyte leukocytosis macrophage malaise neutrophil osmotic pressure perforation permeability phagocytosis purulent pyrexia pyrogens regeneration replacement resolution scar serous stenosis ulcer vasodilation Defense mechanisms used by the body to protect itself from any injurious agent may be specific or nonspecific. One nonspecific or general defense mechanism is the mechanical barrier such as skin or mucous membrane (often called the first line of defense) that blocks entry of bacteria or harmful substances into the tissues (Fig. 5-1). Associated with these mechanical barriers are body secretions such as saliva or tears that contain enzymes or chemicals that inactivate or destroy potentially damaging material. The second line of defense includes the nonspecific processes of phagocytosis and inflammation. Phagocytosis is the process by which neutrophils (a leukocyte) and macrophages,” randomly engulf and destroy bacteria, cell debris, or foreign matter (see Fig. 5-2). Inflammation involves a sequence of events intended to limit the effects of injury or a dangerous agent in the body. Interferons are nonspecific agents that protect uninfected cells against viruses (see Chapter 6). The third line of defense is the specific defense mechanism in the body (see Chapter 7). It provides protection by stimulating the production of unique antibodies or sensitized lymphocytes following exposure to specific substances. In recent years much effort has been expended on research on the immune system in an effort to increase understanding of the process of the immune response and to create ways to strengthen this defense mechanism. Usually all capillaries are not open in a particular capillary bed unless the cells’ metabolic needs are not being met by the blood supply to the area, or an accumulation of wastes (byproduct of metabolism) occurs. Precapillary sphincters composed of smooth muscle restrict blood flow through some channels. Movement of fluid, electrolytes, oxygen, and nutrients out of the capillary at the arteriolar end is based on the net hydrostatic pressure. See Chapter 2 and Figure 2-1 for a detailed explanation of fluid shifts between body compartments. The net hydrostatic pressure is based on the difference between the hydrostatic pressure within the capillary (essentially arterial pressure) as compared with the hydrostatic pressure of the interstitial fluid in the tissues as well as the relative osmotic pressures in the blood and interstitial fluid (Fig. 5-2). Differences in concentrations of dissolved substances in the blood and interstitial fluid promote diffusion of electrolytes, glucose, oxygen, and other nutrients across the capillary membrane. Blood cells and plasma proteins (albumin, globulin, and fibrinogen) normally remain inside the capillary. At the venous end of the capillary hydrostatic pressure is decreased due to the previous movement of fluid into the interstitial fluid space, and osmotic pressure in the vessels is relatively high because plasma proteins remain within the capillaries. This arrangement facilitates the movement of fluid, carbon dioxide, and other wastes into the blood. Excess fluid and any proteins are recovered from the interstitial area by way of the lymphatic system and eventually returned to the general circulation. The inflammatory response is a protective mechanism and an important basic concept in pathophysiology. Inflammation is a normal defense mechanism in the body and is intended to localize and remove an injurious agent, whatever it may be. You have probably observed the inflammatory process resulting from a cut, an allergic reaction, an insect bite, an infection, or a small burn on your body. The general signs and symptoms of inflammation serve as a warning of a problem, which may be hidden within the body. Inflammation is not the same as infection, although infection is one cause of inflammation. With infection, microorganisms such as a bacteria, viruses, or fungi are always present at the site, causing the inflammation. This microbe can be identified and appropriate treatment instituted to reduce the infection, and the inflammation will subside. When inflammation is caused by an allergy or a burn, no microbes are present. Inflammation is the body’s nonspecific response to tissue injury, resulting in redness, swelling, warmth, and pain, and perhaps loss of function. Disorders are named using the ending -itis for inflammation. The root word is usually a body part or tissue; for example, pancreatitis, appendicitis, laryngitis, or ileitis. Inflammation is associated with many different types of tissue injury. Causes include direct physical damage such as cuts or sprains, caustic chemicals such as acids or drain cleaners, ischemia or infarction, allergic reactions, extremes of heat or cold, foreign bodies such as splinters or glass, and infection. An injury to capillaries and tissue cells will result in the following reactions: • Bradykinin is released from the insured cells. • Bradykinin activates pain receptors. • Sensation of pain stimulates mast cells and basophils to release histamine. • Bradykinin and histamine cause capillary dilation. • This results in an increase of blood flow and increased capillary permeability. • Break in skin allows bacteria to enter the tissue. • This results in the migration of neutrophils and monocytes to the site of injury. • Neutrophils phagocytize bacteria. • Macrophages leave the bloodstream and phagocytose microbes. The inflammatory process is basically the same regardless of the cause. The timing varies with the specific cause. Inflammation may develop immediately and last only a short time; it may have a delayed onset (e.g., a sunburn), or it may be more severe and prolonged. The severity of the inflammation varies with the specific cause and duration of exposure. When tissue injury occurs, the damaged mast cells and platelets release chemical mediators including histamine, serotonin, prostaglandins, and leukotrienes into the interstitial fluid and blood (Table 5-1). These chemicals affect blood vessels and nerves in the damaged area. Cytokines serve as communicators in the tissue fluids, sending messages to lymphocytes and macrophages, the immune system, or the hypothalamus to induce fever. TABLE 5-1 Chemical Mediators in the Inflammatory Response Chemical mediators such as histamine are released immediately from granules in mast cells and exert their effects at once. Other chemical mediators such as leukotrienes and prostaglandins must be synthesized from arachidonic acid in mast cells before release and, therefore, are responsible for the later effects, prolonging the inflammation. Many of these chemicals also intensify the effects of other chemicals in the response. Note that many anti-inflammatory drugs and antihistamines reduce the effects of some of these chemical mediators. Although nerve reflexes at the site of injury cause immediate transient vasoconstriction, the rapid release of chemical mediators results in local vasodilation (relaxation of smooth muscle causing an increase in the diameter of arterioles), which causes hyperemia, increased blood flow in the area. Capillary membrane permeability also increases, allowing plasma proteins to move into the interstitial space along with more fluid (see Fig. 5-2). The increased fluid dilutes any toxic material at the site, while the globulins serve as antibodies, and fibrinogen forms a fibrin mesh around the area in an attempt to localize the injurious agent. Any blood clotting will also provide a fibrin mesh to wall off the area. Vasodilation and increased capillary permeability make up the vascular response to injury. During the cellular response, leukocytes are attracted by chemotaxis to the area of inflammation as damaged cells release their contents. Several chemical mediators at the site of injury act as potent stimuli to attract leukocytes. Leukocytes and their functions are summarized in Table 5-2. First neutrophils (polymorphonuclear leukocytes [PMNs]) and later monocytes and macrophages collect along the capillary wall and then migrate out through wider separations in the wall into the interstitial area. This movement of cells is termed diapedesis. There the cells destroy and remove foreign material, microorganisms, and cell debris by phagocytosis, thus preparing the site for healing. When phagocytic cells die at the site, lysosomal enzymes are released and damage the nearby cells prolonging inflammation. If an immune response (see Chapter 7) or blood clotting occurs, these processes also enhance the inflammatory response. TABLE 5-2 Function of Cellular Elements in the Inflammatory Response As excessive fluid and protein collects in the interstitial compartment, blood flow in the area decreases as swelling leads to increased pressure on the capillary bed, and fluid shifts out of the capillary are reduced. Severely reduced blood flow can decrease the nutrients available to the undamaged cells in the area and prevent the removal of wastes. This may cause additional damage to the tissue. There are naturally occurring defense or control mechanisms in the form of enzymes that inactivate chemical mediators and prevent the unnecessary spread or prolongation of inflammation. The cardinal signs of inflammation are redness (rubor or erythema), heat, swelling, and pain: • Redness and warmth are caused by increased blood flow into the damaged area (Fig. 5-3). • Swelling or edema is caused by the shift of protein and fluid into the interstitial space. Exudate refers to a collection of interstitial fluid formed in the inflamed area. The characteristics of the exudate vary with the cause of the trauma: Other general manifestations of inflammation include mild fever, malaise (feeling unwell), fatigue, headache, and anorexia (loss of appetite). Fever or pyrexia (low grade or mild) is common if inflammation is extensive. If infection has caused the inflammation, fever can be severe, depending on the particular microorganism. However, high fever can be beneficial if it impairs the growth and reproduction of a pathogenic organism. Fever results from the release of pyrogens, or fever-producing substances (e.g., interleukin-1), from white blood cells (WBCs) or macrophages (Fig. 5-4). Pyrogens circulate in the blood and cause the body temperature control system (the thermostat) in the hypothalamus to be reset at a higher level. Heat production mechanisms such as shivering are activated to increase cell metabolism. Involuntary cutaneous vasoconstriction characterized by pallor and cool skin reduces heat loss from the body. Voluntary actions such as curling up or covering the body conserve heat. These mechanisms continue until the body temperature reaches the new, higher setting. Following removal of the cause, body temperature returns to normal by reversing the mechanisms. Refer to the normal values shown on the inside front cover of this book. Leukocytosis (increased white blood cells in the blood), elevated serum C-reactive protein (CRP), an elevated erythrocyte sedimentation rate or ESR, and increased plasma proteins and cell enzymes in the serum are nonspecific changes (Table 5-3); they do not indicate the particular cause or site of inflammation. They provide helpful screening and monitoring information when a problem is suspected or during treatment. In patients with leukocytosis, there is often an increase in immature neutrophils, commonly referred to as “a shift to the left.” A differential count (the proportion of each type of WBC) may be helpful in distinguishing viral from bacterial infection. Allergic reactions commonly produce eosinophilia. Examination of a peripheral blood smear may disclose significant numbers of abnormal cells, another clue as to the cause of a problem. Increased circulating plasma proteins (fibrinogen, prothrombin, and alpha-antitrypsin) result from an increase in protein synthesis by hepatocytes. TABLE 5-3 Changes in the Blood with Inflammation
Inflammation and Healing
Learning Objectives
Key Terms
Review of Body Defenses
Mechanical Barriers
Nonspecific Mechanisms
Specific Mechanisms
Review of Normal Capillary Exchange
Physiology of Inflammation
Definition
Causes
Steps of Inflammation
Acute Inflammation
Pathophysiology and General Characteristics
Chemical
Source
Major Action
Histamine
Mast cell granules
Immediate vasodilation and increased capillary permeability to form exudate
Chemotactic factors
Mast cell granules
For example, attract neutrophils to site
Platelet-activating factor (PAF)
Cell membranes of platelets
Activate neutrophils
Platelet aggregation
Cytokines (interleukins, lymphokines)
T lymphocytes, Macrophages
Increase plasma proteins, ESR
Induce fever, chemotaxis, leukocytosis
Leukotrienes
Synthesis from arachidonic acid in mast cells
Later response: vasodilation and increased capillary permeability, chemotaxis
Prostaglandins (PGs)
Synthesis from arachidonic acid in mast cells
Vasodilation, increased capillary permeability, pain, fever, potentiate histamine effect
Kinins (e.g., bradykinin)
Activation of plasma protein (kinogen)
Vasodilation and increased capillary permeability, pain, chemotaxis
Complement system
Activation of plasma protein cascade
Vasodilation and increased capillary permeability, chemotaxis, increased histamine release
Leukocytes
Activity
Neutrophils
Phagocytosis of microorganisms
Basophils
Release of histamine leading to inflammation
Eosinophils
Numbers are increased in allergic responses
Lymphocytes
Activity
T lymphocytes
Active in cell-mediated immune response
B lymphocytes
Produce antibodies
Monocytes
Phagocytosis
Macrophages
Active in phagocytosis. These are mature monocytes that have migrated into tissues from the blood.
Local Effects


Systemic Effects
Diagnostic Tests
Leukocytosis
Increased numbers of white blood cells, especially neutrophils
Differential count
Proportion of each type of white blood cell altered, depending on the cause
Plasma proteins
Increased fibrinogen and prothrombin
C-reactive protein
A protein not normally in the blood, but appears with acute inflammation and necrosis within 24-48 hours
Increased ESR
Elevated plasma proteins increase the rate at which red blood cells settle in a sample
Cell enzymes
Released from necrotic cells and enter tissue fluids and blood: may indicate the site of inflammation ![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Basicmedical Key
Fastest Basicmedical Insight Engine