Infectious Processes
Dawn F. Rondeau
Key Questions
• What factors influence the transmission of infectious agents?
• What conditions compromise host defenses against microorganisms?
• What are opportunistic infections, and when do they develop?
![]()
http://evolve.elsevier.com/Copstead/
Infectious diseases can be caused by bacteria, viruses, fungi, and animal- or insect-borne parasites that enter the body by penetrating natural barriers. Viruses are the single most common cause of infectious diseases worldwide.1 Although treatments are available for many of these diseases, development of resistant strains complicates successful treatment in some cases.
A variety of pathogens inhabit different environments such as hospitals, the food supply, water, animals, and humans. For example, many hospitalized patients are at risk for the development of sepsis, an overwhelming infection that may lead to shock, multiple organ failure, and death. The methods for preserving the food supply have an impact on transmission of infections, as do the location, density, and sanitary practices of a population. Globalization of the world’s population, with the associated rapidity and extent of air travel, has major implications for the worldwide spread of infectious agents before the infected individual becomes symptomatic or identifiable.
Infection with pathogenic microorganisms has become a tool of war and terrorism in the world. Whether it is anthrax spores sent through the mail or the threat of smallpox being introduced into an unimmunized population, methods of preventing infection have a key role in the defense of humanity.
Medications that inhibit the immune response in populations such as transplant or cancer patients, and the use of immunomodulators for treatment of diseases like rheumatoid arthritis, increase the likelihood of opportunistic infections. Excessive use of antibiotics in humans and domesticated animals has contributed to the emergence of treatment-resistant infections. Health care professionals have a vital role in the prevention, early detection, and management of infections.
Epidemiologic Concepts
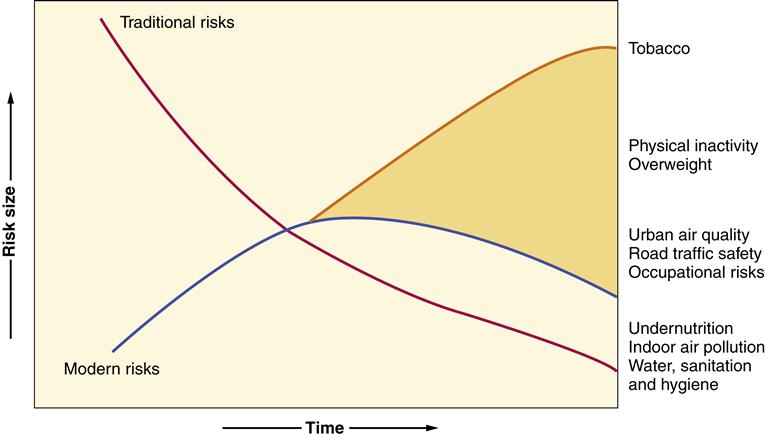
Epidemiology is the study of the causes, distribution, and control of disease in populations. Epidemiology evaluates where, when, and to whom a health event happens and quantifies the risk associated with a particular event.2 The risk to a population for development of disease varies with the population. For example, in a low-income population the risks are related to poor water supply, poor sanitation, and inadequate nutrition. In affluent populations the risks of decreased physical activity, increased body fat, and poor urban air quality are more important3 (Figure 8-1). Epidemiology is discussed in more detail in Chapter 1.
One of the first attempts to identify the cause of an infection and develop a method to prevent it was conducted by Benjamin Jesty in England in the mid-1700s. He noticed that milkmaids who developed cowpox from working with cows did not develop smallpox disease. He deduced that there was a connection between cowpox and smallpox. He exposed his wife and children to cowpox to protect them from smallpox and provided an example of the successful use of epidemiological principles and inoculation to prevent disease.4
Jesty also performed basic statistical analyses of the numbers of people who developed infections and the numbers who did not, using the concepts of prevalence and incidence. The prevalence of a disease is the number of people who have that disease during a year (e.g., the number of people living with human immunodeficiency virus [HIV] infection). The number of people who develop a new infection in a year is the incidence. The number of new cases within a given population is the incidence rate (e.g., 10 cases per 1000 persons).5 A variety of other statistics can be used for surveillance, monitoring, and investigation of outbreaks.6
An infectious disease that has a fairly constant presence in a community and changes little from year to year, such as the sexually transmitted disease Chlamydia, is classified as endemic. A significant increase in new infections in a certain population, such as a measles outbreak at a university, is termed an epidemic. An epidemic that has spread to a large geographic area is a pandemic. The bubonic plague, which caused 100 million deaths worldwide in the 1300s, was a pandemic.
The study of infectious diseases requires the evaluation of many factors to determine the association of a disease with its cause. The United States Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO) have pivotal roles in identifying diseases, tracking their natural history, and defining protocols for their control and prevention. An example of how these organizations can control disease is the virtual eradication of smallpox. The World Health Organization, with the cooperation of other health organizations such as the Centers for Disease Control and Prevention, mandated immunizations for all those susceptible to the disease that were living in or traveling to areas where smallpox was prevalent. This immunization program, coupled with the lack of a viral host other than humans, led to the eradication of smallpox, except in the laboratory. Only the fear of the reintroduction of the virus into the population in a bioterrorism attack or biological warfare may mandate the continued immunization of susceptible populations such as health care workers, emergency personnel, and the military.
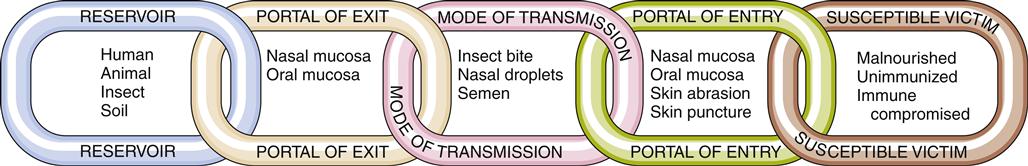
Transmission of Infection
The transmission of infection or disease requires an unbroken chain of events to enable one host to infect another7 (Figure 8-2). Disease-causing organisms (pathogens) must live and reproduce in a reservoir. The reservoir may be a human, as in the influenza virus; an animal, as in rabies; an insect, as in West Nile virus; or soil, as in enterobiasis (pinworm infestation).
The pathogen must have a portal of exit and a mode of transmission from the reservoir to a susceptible host. The portal of exit is usually closest to the breeding site of the organism. For example, Neisseria gonorrhoeae, the organism that is responsible for gonorrhea, usually resides in the urethra of an infected male and in the vaginal canal of an infected female. The microorganism is transmitted to others by sexual contact.
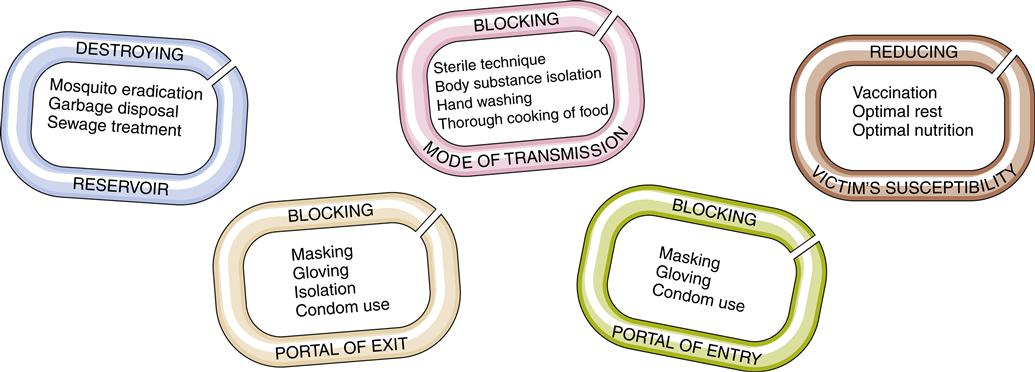
Control of disease acquisition depends on breaking the chain of transmission in one or more places8 (Figure 8-3). A pathogen can be vulnerable in one or more links of the transmission chain. The goal of epidemiology is to identify these vulnerabilities and exploit them to stop disease transmission.
The ability of a pathogen to cause disease is influenced by the ability to communicate the infection, in other words the ability to spread and cause the disease. The ability to invade and multiply within the host is termed infectivity. Some pathogens have a greater ability to spread and multiply in the host, increasing their infectivity. This difference in the mechanism of action can make one pathogen much better at causing disease (pathogenicity) and some can cause very severe disease (virulence). The ability to cause disease is also influenced by the access to a host. For example, respiratory diseases caused only by exposure to droplets are much more easily transmitted than a disease that requires direct contact. Some pathogens produce toxins or endotoxins that can markedly increase the toxigenicity of the organism.9
Transmission of infection is defined as any mechanism by which an infectious agent is spread through the environment to another person.7 These mechanisms can be either direct or indirect. There are three direct transmissions. The most common transmission occurs through the exchange of body fluids (droplets) from kissing or sexual intercourse. In this type of transmission droplets are spread from an infected host to the conjunctiva or mucous membranes of a second host. The second type of direct transmission occurs from the bite of an animal (e.g., rabies) or from soil (e.g., systemic mycosis) transmitting the inoculant. The third type of direct transmission occurs through the placenta when diseases such as HIV are transmitted directly to the fetus.6
Indirect transmissions occur as vehicle-borne, vector-borne, or airborne transfers. A vehicle-borne transfer occurs when an infectious agent is transported to the host. The vehicle could be food, water, clothing, plasma, or tissues. The agent does not require any development or multiplication and is delivered without change with the vehicle. Airborne transmission occurs with aerosols including suspensions of particles (smaller than the size of droplets), which can be carried great distances from the source for transmission. Examples are outbreaks of measles and legionnaires disease. Vector-borne transmission can occur as a mechanical or biological transfer. The mechanical transfer occurs when an insect carries an infectious agent on its feet or proboscis (Figure 8-4). In this transfer the agent does not require multiplication or development before transfer. This is in contrast to biological vector-borne transport. In this type of transmission the agent propagates and there is cyclic development before the arthropod can transmit the disease.6
The human body also contains a variety of microorganisms that colonize the body and are called normal flora. These flora occur naturally and have a role in defense by occupying space, competing for nutrients, stimulating cross-protective antibodies, and reducing or containing the growth of potentially disease-causing bacteria or fungi. These organisms can become pathogens and cause disease if the host defenses are altered, as in the case of patients receiving chemotherapy. For example, Staphylococcus epidermidis is commonly present on the skin. With an injury to the skin, or injection through the skin, this normal bacterial flora can be introduced to a different space in the body and then become an infectious agent.10
Destroying nonhuman reservoirs and vectors of the pathogen can break the chain of transmission. For example, controlling the number of mosquitoes with insecticides and other biological means is a method used to curb the spread of malaria and West Nile virus. Immunization of domesticated animals against rabies eliminates one reservoir of potential rabies transmission. Distribution of clean needles in the intravenous drug user community is aimed at removing a common transmission vector (contaminated needles) for HIV, the causative pathogen responsible for acquired immunodeficiency syndrome (AIDS).
Blocking the portal of exit can also block transmission of the pathogen. Having patients with tuberculosis wear face masks while they move through the hospital and implementing respiratory isolation techniques to stop transmission are interventions aimed at blocking the portal of exit. Standard precautions are infection-control guidelines designed to block the pathogen’s portal of exit, route of transmission, and portal of entry.2 Hand washing is one of the most effective ways to break the chain of transmission by blocking an important mode of transmission—contaminated hands. Many factors influence the risk of exposure to foreign materials and the occurrence of infection (Table 8-1).
TABLE 8-1
| INNATE IMMUNITY | ADAPTIVE (ACQUIRED) IMMUNITY | ||
| CHARACTERISTICS | BARRIERS | INFLAMMATORY RESPONSE | |
| Level of defense | First line of defense against infection and tissue injury | Second line of defense; occurs as response to tissue injury or infection | Third line of defense; initiated when innate immune system signals cells of adaptive immunity |
| Timing of defense | Constant | Immediate response | Delay between primary exposure to antigen and maximum response; immediate against secondary exposure to antigen |
| Specificity | Broadly specific | Broadly specific | Response is very specific toward “antigen” |
| Cells | Epithelial cells | Mast cells, granulocytes (neutrophils, eosinophils, basophils), monocytes/macrophages, natural killer (NK) cells, platelets, endothelial cells | T lymphocytes, B lymphocytes, macrophages, dendritic cells |
| Memory | No memory involved | No memory involved | Specific immunologic memory by T and B lymphocytes |
| Peptides | Defensins, cathelicidins, collectins, lactoferrin, bacterial toxins | Complement, clotting factors, kinins | Antibodies, complement |
| Protection | Protection includes anatomic barriers (i.e., skin and mucous membranes), cellular components, and secretory molecules or cytokines (e.g., lysozymes, low pH of stomach and urine, and ciliary activity) | Protection includes vascular responses, cellular components (e.g., mast cells, neutrophils, macrophages), secretory molecules or cytokines, and activation of plasma protein systems | Protection includes activated T and B lymphocytes, cytokines, and antibodies |
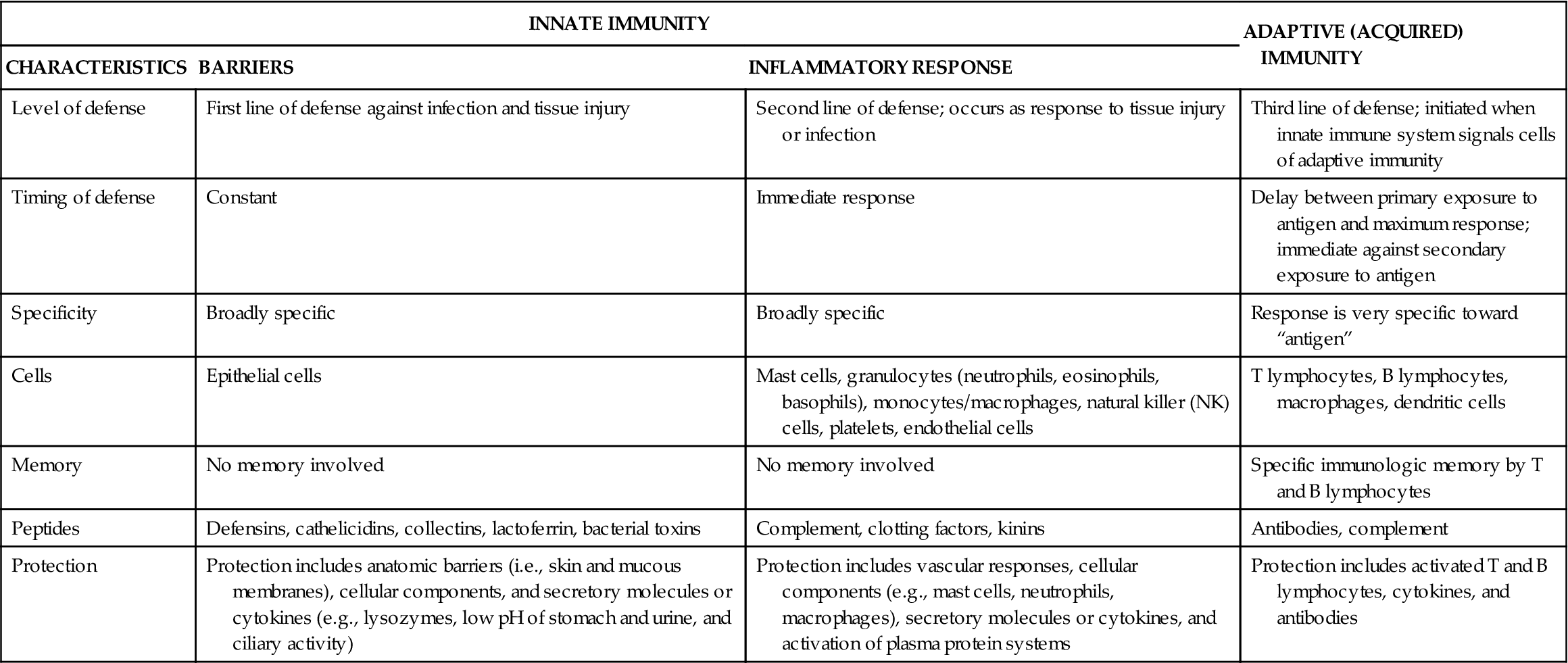
From McCance K, Huether S: Pathophysiology: the biologic basis for disease in adults & children, ed 6, St Louis, 2010, Mosby.
Role of Host
The body’s defense system is responsible for identifying foreign materials and neutralizing or eliminating them without injuring its own tissues.6 Responses to a pathogen can be either innate or specific. Innate responses occur on the initial exposure to the antigen, whereas a specific response is slow to develop and more efficient on subsequent exposures. Immune responses can be modified by the characteristics of the host, including genetics, age, metabolism, anatomic, and physiologic and environmental factors6,11 (Table 8-2). Host immune systems are discussed in greater detail in Chapter 9.
TABLE 8-2
HOST CHARACTERISTICS INFLUENCING INFECTION
| Exposure | Host Health |
| Animals, humans, insects, parasites Environmental Water, toxins, pollutants, radiation, sewage Hygiene Toileting, hand washing, dental care, bathing Social Behaviors Illicit drug use, alcohol, smoking Risk taking: sexual, sports Travel Exposure to vectors in undeveloped countries | Intact immune system Absence of chronic disease such as diabetes Absence of genetic abnormality Nutritional Status Adequate intake of proteins, vitamins, and minerals Antibiotic Exposure Recent use, noncompletion of course Development of resistance or allergy |
Host Characteristics
Physical and Mechanical Barriers
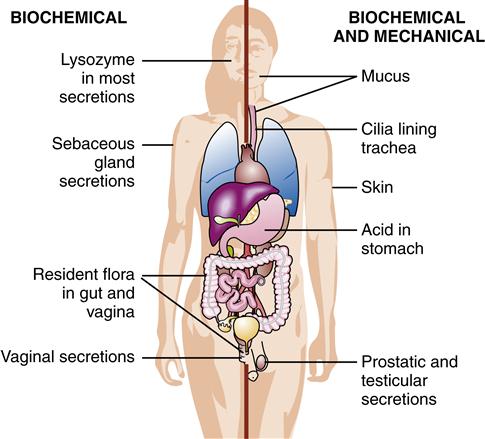
Intact physical barriers act as a blockade to foreign material entering the body (Figure 8-5). Epithelial cells of the skin and those that line the gastrointestinal, genitourinary, and respiratory tracts are tightly linked and provide an initial barrier to infection. Because the intestinal epithelial cell half-life is 30 hours, the constant shedding of the epidermis and mucosal membranes aids in the removal of any microorganisms that are attached to their surfaces.9 In addition, the high fat content of the skin inhibits the growth of bacteria and fungi. Changes in this barrier are sometimes the route for normal flora to become infectious.12
The mucous membrane linings of the gastrointestinal and genitourinary tracts provide a barrier separating the sterile internal body from the external environment. The lungs are protected with a layer of mucous lining. The sticky consistency of mucus traps microorganisms, and the cilia sweep the microorganisms from the body. The mucociliary system and alveolar macrophages are important for ridding the lungs of trapped microorganisms. Mechanisms such as coughing, sneezing, and urinating help to remove particles trapped on mucous membranes of the body.9
Biochemical barriers enhance the effectiveness of the mechanical barriers. The acidic environment of the skin, urine, and vagina inhibits bacterial growth. The secretion by the stomach of hydrochloric acid (with a pH of 1 to 2) results in the killing of microorganisms. Saliva, mucus, tears, and sweat contain antimicrobial chemicals such as lysozyme, an enzyme that destroys cell walls of gram-positive bacteria.9 Lactoferrin is a mucosal protein that keeps bacterial replication low by reducing the availability of free iron needed for bacterial growth. Sebaceous gland secretions act as antifungals. Immunoglobulins (immunoglobulin A [IgA], immunoglobulin G [IgG]) are present in many of the body’s secretions and prevent entry of bacteria and viruses through mucous membranes.13 (See Chapter 9 for a discussion about immunoglobulins.)
Removal or degradation of the body’s mechanical and biochemical barriers creates a setting in which infection is likely. For example, burn victims who have lost portions of their skin barrier are at high risk for infection. Cellular changes induced by smoking reduce the number of cilia in the respiratory tract. The normal action of cilia in the respiratory tract in removing foreign particles is blocked by endotracheal tubes. Hospitalized patients who have incisions or intravenous and urinary catheters are at risk for infection because their skin barrier has been breached. When a urinary catheter is in place, flushing of bacteria from the urinary tract opening (meatus) is bypassed.
Risk Factors
Nutritional status
The World Health Organization (WHO) reports that inadequate nutrition is a general risk factor for disease and is a particularly important factor in tuberculosis (TB) infection.14 Protein-energy malnutrition is associated with defects in cell-mediated immunity (specific), impaired intracellular destruction by neutrophils, reduced complement activity, and decreased levels of secretory IgA.15 At the time of an illness, nutrition is negatively affected by decreased appetite, malabsorption, diarrhea, diversion of nutrients for immune responses, and urinary nitrogen loss, further exacerbating a malnourished state. The presence of fever increases the metabolic rate, requiring more energy and micronutrients. Malnutrition exists because of the lack of available clean and safe food. Contributing factors include decreased financial resources, inadequate housing, potentially unsafe water supplies, and the lack of or accessibility to health care.
Micronutrients are also important in immune function. Vitamin A contributes to maintenance of the epithelium and vitamin E is an antioxidant that supports the development and function of T cells.16 Vitamin D supports innate and adaptive immunity and promotes immune protection against tuberculosis by increasing macrophage defenses.9 Decreased availability of zinc results in a reduction in neutrophil and natural killer cell function, complement activity, and lymphocyte activity. Iron deficiency is associated with decreased cell-mediated immunity and reductions in neutrophil action. Iron deficiency is one of the most common deficiencies worldwide.17
Age
Age is also a variable in the ability to resist infections. Viruses such as mumps, polio, or Epstein-Barr virus (EBV) cause less severe infection in infants, whereas others such as rotaviruses result in severe illness in infants. These age-related factors may reflect the availability of immune factors or the maturity of the immune system.12 T-cell function appears to be impaired in newborns, with the majority of the immune response provided by maternal IgG that crossed the placenta. As this immunity fades over approximately the first 6 months of life, these newborns are more at risk of serious infection. Those infants who are breast feeding will obtain secretory IgA, which does provide additional protection.13 Immunity tends to decline in the elderly, resulting in reduced antibody responses to new antigens. The immune system may become disregulated as evidenced by the increased frequency of autoimmune diseases with age.13
Chronic illness and immunosuppression
Chronic illnesses such as diabetes, cancer, heart disease, and renal failure are associated with an increased risk of infection. Deaths in patients with chronic illnesses are frequently directly related to an infectious process. Diabetes alters the host’s ability to resist infection. Phagocytosis is impaired with hyperglycemia, and detection of the pain of infection may be delayed because of neuropathies. The invasiveness of the microorganisms is increased when exposed to hyperglycemic environments. This increased risk of infectious disease in a population with chronic disease is multifactorial and includes the nature of their chronic disease, medications, treatments, exposure to health care settings, and the innate genetics of the individual.
Immunocompromised patients have an increased risk of severe, rapidly progressing infections that may be unresponsive to usual treatments. Infection with pathogens that are usually not pathogenic is an indicator that a person is immunocompromised. The immunocompromised status might be a result of genetic disorders (such as hypogammaglobulinemia) or may be acquired (such as in patients who have undergone a splenectomy). The prevalence of people with transplants and medication-induced immunosuppression is increasing. Antirejection medications such as corticosteroids, cyclosporine, and tacrolimus contribute to immunosuppression in transplant patients.18 People who take corticosteroids and immunomodulators to suppress inflammatory and autoimmune diseases are also at high risk of infection. Human immunodeficiency virus (HIV) disease is an important chronic condition that predisposes to a variety of other infections (see Chapter 12).
The physiologic response to chronic stress is thought to contribute to risk for infection. The neurohormonal alterations lead to changes in the levels of cortisol and other stress hormones that may affect immune responsiveness (see Chapter 2).
Role of Immunization
Immunization of a population is the most effective means to reduce morbidity and mortality from vaccine-preventable diseases such as hepatitis A, hepatitis B, influenza, and pneumococcal infections.18 There are two goals of immunization. The first is to confer immunity to a host by direct exposure to the altered pathogen. The second is to decrease the number of susceptible hosts in the population, thereby limiting the possibility of transmission of the disease. By this method, known as herd immunity, the disease can be controlled or eliminated without immunizing everyone, as long as a high enough percentage of the population is immunized. The number of susceptible hosts in the population decreases as immunization rates increase. When a critical percentage of the susceptible population is immunized, the chain of transmission is broken and the disease outbreak averted. If the percentage of adequately immunized individuals drops, epidemics may result.
Immunization with preformed antibodies to the infectious agent provides immediate immunity. Immunizations with killed vaccines such as influenza provide immunity without the risk of infection from the agent. This type of vaccination may require several doses spaced at intervals to allow for continued development of an antibody level sufficient to prevent disease.12 The increased prevalence of pertussis infection in recent years demonstrates the importance of continued monitoring of vaccine use. Historically, the last pertussis dose was given with the last tetanus dose of a teenaged child. Increasing occurrence rates precipitated a CDC recommendation for a booster dose for adults ages 19 to 64 years.18 The CDC provides updates and recommendations for immunizations for adults, children, and travelers (www.cdc.gov).
Role of Environment
Multiple environmental factors affect the prevalence and transmission of various infections and infestations. For example, parasitic infections are facilitated by hot and humid climates, overcrowded living conditions, the presence of insect vectors in bed linen or clothing, improper sewage disposal or treatment (such as the use of raw human sewage as fertilizer), the lack of clean water, and the consumption of contaminated raw or undercooked meat or vegetables.
Infections may be transmitted by inhalation of polluted dust or air. For example, the fungus Coccidioides immitis, which causes valley fever, is pandemic in the southwestern United States. Toxoplasmosis is caused by inhalation or ingestion of dirt, sand, or litter dust contaminated with cat feces that contain the causative protozoon Toxoplasma gondii. The plague is still a disease of concern in many countries. It is caused by the bacterium Yersinia pestis, which is carried by a rodent flea.19 There are multiple examples of foodborne illness such as Salmonella, with outbreaks related to improper processing, storage, or cooking of meats and raw produce.20
The risk factors for tuberculosis (TB) include crowded living conditions, poor nutrition, frequent contact with those who have TB, and extremes of age (i.e., infants and elderly). Those with reduced immune function attributable to HIV infection, medications, or other risks as previously listed are also at risk for TB.21
There are periodic outbreaks of diseases that occur related to travel, shipments of food products, and vaccination levels. Monitoring of travel from those countries with known endemic vaccine-preventable diseases is important to prevent global transmission. SARS (severe acute respiratory syndrome) was identified in 2003 in a businessman traveling from China to Vietnam. The diagnosis was made by WHO physician Dr. Carlo Urbani. This life-threatening disease required the skills of the WHO to identify it as a new and different disease. Unfortunately, Dr. Carlo Urbani died from this disease as did the original patient. This coronavirus, which is transmitted as a respiratory virus, is believed to have originated from small mammals in China and developed into a lethal disease. It is a tribute to the WHO and cooperating agencies that SARS was identified as a global health threat, and a travel advisory was issued.22,23