• Vitamin A: plays an essential role in maintaining the integrity of the epithelial and mucosal surfaces and their secretions. These systems constitute a primary nonspecific host defense mechanism. Vitamin A has been shown to stimulate and/or enhance numerous immune processes, including induction of cell-mediated cytotoxicity against tumors, natural killer cell activity, lymphocyte blastogenesis, mononuclear phagocytosis, and antibody response. • Carotenes: have demonstrated a number of immune-enhancing effects. In addition to being converted into vitamin A, carotenes function as antioxidants. Because the thymus gland is so susceptible to damage by free radicals, beta-carotene may be more advantageous in enhancing the immune system than retinol. • Vitamin C: ascorbic acid plays an important role in immune enhancement. Although vitamin C has been shown to be antiviral and antibacterial, its main effect is by improvement in host resistance. Many immunostimulatory effects have been demonstrated, including enhancing lymphoproliferative response to mitogens and lymphotrophic activity and increasing interferon levels, antibody responses, immunoglobulin levels, secretion of thymic hormones, and integrity of ground substance. Vitamin C also has direct biochemical effects similar to those of interferon. • Vitamin E: enhances both humoral immunity and cell-mediated immunity. A vitamin E deficiency results in lymphoid atrophy and decreases of lymphoproliferative response to mitogens, splenic plaque-forming colonies, antibody response, and monocyte function. Vitamin E supplementation (30-150 IU) has been shown to increase lymphoproliferative response to mitogens; prevent free radical–induced thymus atrophy; enhance helper T-cell activity; and increase splenic plaque-forming colonies, serum immunoglobulins, antibody response, peripheral mononuclear phagocytosis, and reticuloendothelial system activity. • Iron: iron deficiency is a commonly encountered isolated nutritional deficiency that causes immune dysfunction in large numbers of patients. Marginal iron deficiency, even at levels that do not lower hemoglobin values, can influence the immune system. Lymphoid tissue atrophy, decreased lymphoproliferative response to mitogens, defective macrophage and neutrophil function, and decreased T-cell/B-cell ratios are common experimental and clinical findings. • Zinc: zinc serves a vital role in many immune system reactions. It promotes the binding of complement to immune complex, acts as a protectant against iron-catalyzed damage by free radicals, acts synergistically with vitamin A, is required for lymphocyte transformation, acts independently on lymphocytes as a mitogen, and is a necessary cofactor in activating serum thymic factor. In vitro, zinc inhibits the growth of several viruses, including rhinoviruses, picornaviruses, togaviruses, herpes simplex virus, and vaccinia virus. • Selenium: in its vital role in glutathione peroxidase, selenium affects all components of the immune system, including the development and expression of all white blood cells (WBCs). Selenium deficiency results in depression of immune function, whereas selenium supplementation results in augmentation and/or restoration of immune functions. Selenium deficiency has been found to inhibit resistance to infection through impairment of WBCs and thymus function, whereas selenium supplementation (100-200 μg/day) has been shown to stimulate WBC and thymus function.
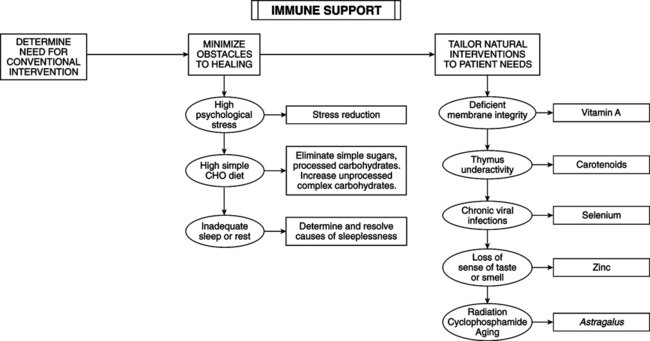
Immune Support
THERAPEUTIC CONSIDERATIONS
Lifestyle
Nutrients
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Immune Support