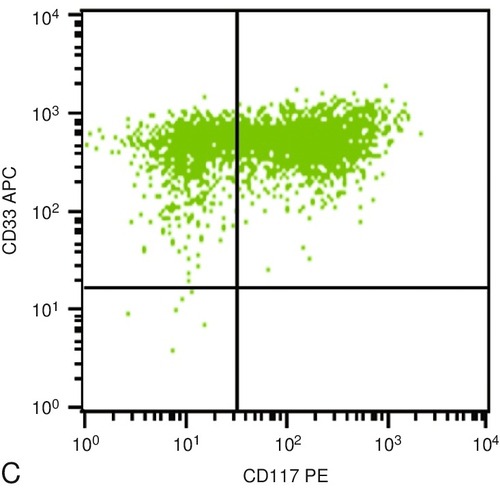
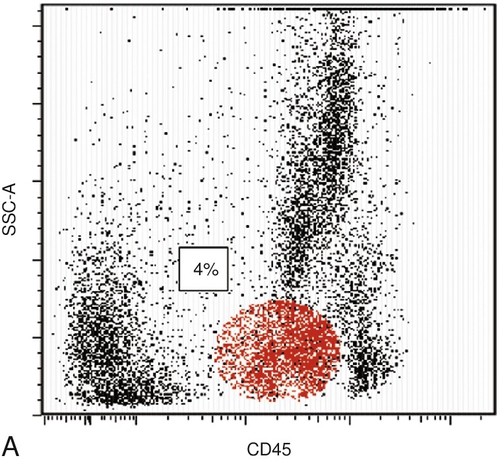
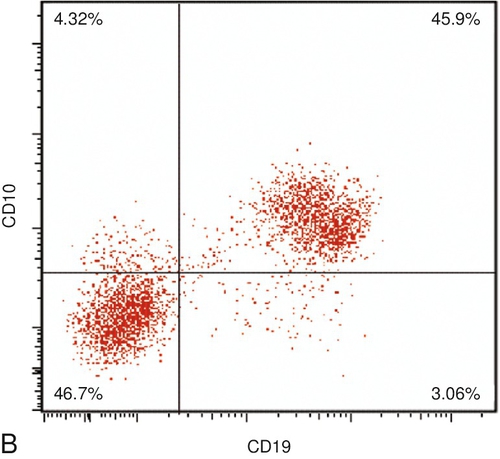
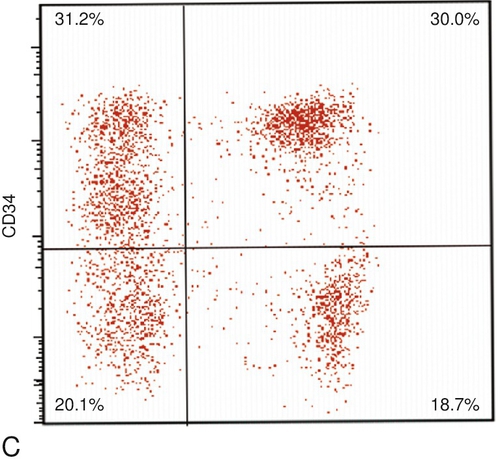
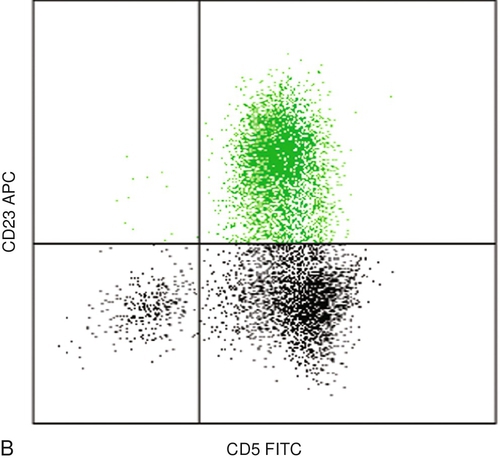
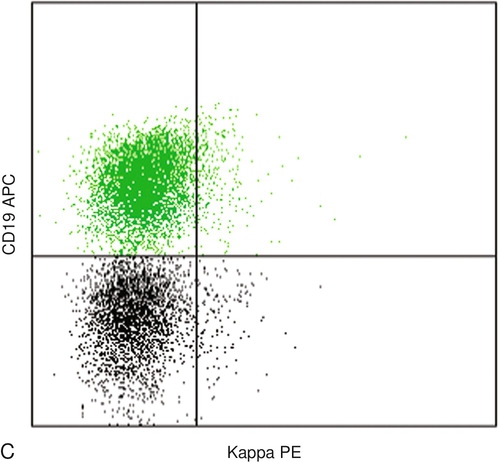
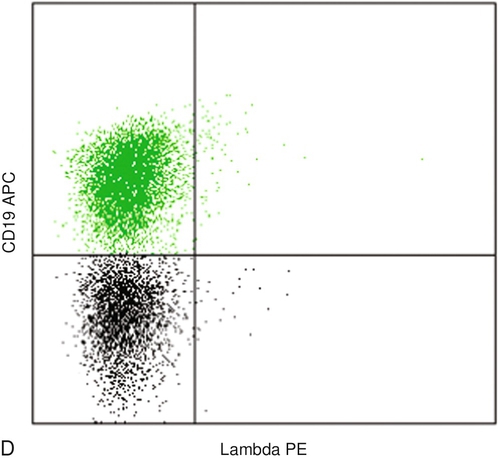
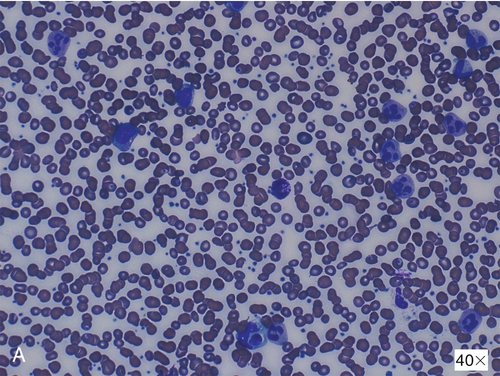
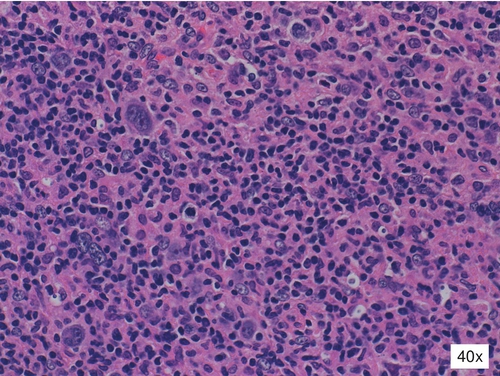
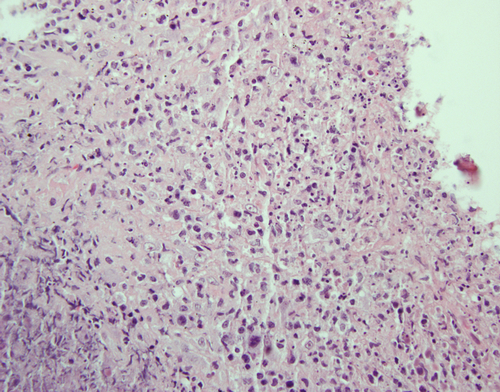
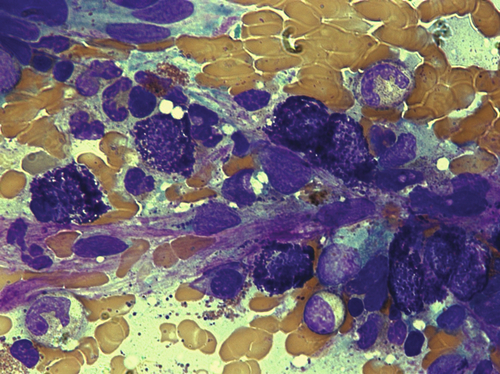
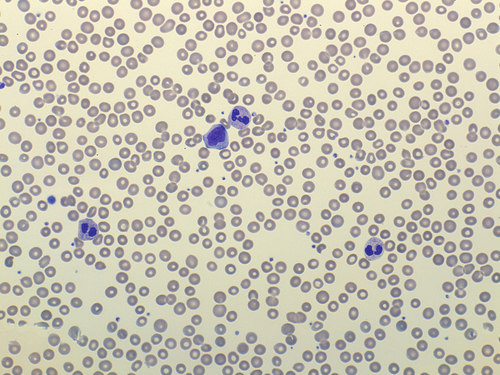
Chapter 11 Adriana I. Colovai; Mark D. Ewalt; Paul R. Hosking 1. A peripheral blood sample obtained from a 78-year-old woman with a white blood cell (WBC) count of 266 × 109/L (reference range, 4.4 to 11.3 × 109/L) was submitted for flow cytometric analysis. In the dot plots shown in Figure 11-1, the cells of interest are highlighted in green. Which one of the following is the most likely diagnosis based on these findings? A. Acute monoblastic leukemia. B. Acute myelomonocytic leukemia. C. Acute myeloid leukemia (AML) without maturation. D. Acute promyelocytic leukemia (APL). E. Acute T-cell leukemia. 2. A bone marrow aspirate sample obtained from a 3-year-old girl with a history of acute B-lymphoblastic leukemia (B-ALL) was submitted for flow cytometry and cytogenetic analysis as part of the end-of-treatment evaluation. Cytogenetic analysis indicated no abnormalities in the current bone marrow aspirate. The flow cytometry panel shown in Figure 11-2 illustrates the results obtained from the same specimen. CD45 dim/low side scatter cells (SSCs), which include hematopoietic precursors, represent 4% of all nucleated cells and are shown in red. Which one of the following is true based on these results? B. There is no clear evidence of B-ALL. However, the findings are suggestive of myelodysplasia with an excess of blasts. C. There is no clear evidence of B-ALL. Normal lymphoid and myeloid precursors in a regenerating marrow are observed. D. There is no clear evidence of B-ALL. However, the flow cytometry findings are suggestive of a mature B-cell neoplasm. 3. A peripheral blood sample from a 33-year-old woman with lymphocytosis and severe anemia was sent for flow cytometric analysis. The dot plots shown in Figure 11-3 illustrate the cell surface profile of the lymphocytes, with the cells of interest represented in green. Which one of the following is the most likely diagnosis? A. Chronic lymphocytic leukemia. B. Mantle cell lymphoma (MCL). C. Acute B-ALL. D. Normal B cells. E. Follicular lymphoma (FL). 4. Which one of the following best describes compensation in flow cytometric analysis? A. Adjustment of forward and side scatter signals. B. Adjustment of the instrument noise using nonfluorescent particles. C. Adjustment for signals from fluorochromes other than the specific fluorochrome in a single detector. D. Adjustment of the excitation and emission spectra of different fluorochromes. E. Excitation of a primary fluorochrome that transfers energy to a secondary fluorochrome. 5a. A 62-year-old man presents to his primary care physician with 2 months of fatigue and a 5-lb weight loss. His physician orders a complete blood count with differential, and his peripheral blood smear is shown in Figure 11-4, A. Which one of the following genetic/karyotypic abnormalities is diagnostic of the disease from which this patient most likely suffers? B. Translocation t(9;22)(q34;q11.2). C. Trisomy 8. D. Translocation t(9;14)(p13;q32). E. Deletion 5q. 5b. The patient is treated with targeted therapy for the genetic alteration noted above and enters clinical remission. After 5 years, the patient begins to feel fatigued again and notes abdominal fullness. When he returns to his primary care physician, he is found to have splenomegaly, and a complete blood cell count shows hemoglobin 10 g/dL (reference range, 13.3 to 15.2 g/dL), platelets 99 × 109/L (reference range, 165 to 415 × 109/L), and WBC count 53 × 109/L (reference range, 3.5 to 9.1 × 109/L) with 18% myeloblasts. Which one of the following is the patient’s diagnosis at this time (Figure 11-4, B)? A. AML with recurrent genetic abnormalities. B. AML, therapy-related (t-AML). C. Chronic myelogenous leukemia, accelerated phase (CML, AP). D. Myelodysplastic syndrome (MDS), refractory anemia with excess blasts II (MDS/RAEB-II). E. Blastic plasmacytoid dendritic cell neoplasm (BPDC). 5c. Which one of the following factors is most important in this patient’s prognosis? B. Degree of bone marrow fibrosis. C. Presence of cytogenetic abnormalities. D. Response to targeted therapy. E. Transfusion dependence. 6a. The differential blood count results shown in Table 11-1 are from a 44-year-old man with HIV. Flow cytometric analysis of the same blood sample showed that CD4 + T cells represent 2% of all lymphocytes. Which one of the following is the CD4 + T-cell count of this patient? B. 740 × 106/L. C. 90 × 106/L. D. There is insufficient information to determine the CD4 + T-cell count. 6b. Flow cytometric analysis of this patient’s peripheral blood identified a subpopulation of CD3 + CD4 − CD8 − T cells, which accounted for 10% of the lymphocytes. Which one of the following do these cells most likely represent? B. Helper T cells showing HIV-induced downregulation of CD4 expression. C. Gamma/delta T cells. D. Immature T cells. A 4-year-old girl presents to the emergency department with multiple bruises on her limbs and recent weight loss of 4 lb. When asked, the patient’s mother reports that the child has been progressively fatigued and seems to be weak. The patient’s past medical history is significant for hemophagocytic lymphohistiocytosis, for which she was treated with etoposide, corticosteroids, cyclosporine, and intrathecal methotrexate. She then received a bone marrow transplantation. Her current complete blood cell count shows anemia, thrombocytopenia, and marked lymphocytosis with 88% blasts. The peripheral smear is shown in Figure 11-5, A. Use this scenario to answer the following three questions. 7a. Which one of the following statements regarding the phenotypic characteristics of acute leukemia is true? A. Terminal deoxynucleotidyl transferase (TdT) can be positive in a subset of AMLs. B. If the lesional cells express CD13, they must be of the myeloid lineage. C. CD19 expression is almost never observed in AML. D. CD117 is commonly seen in ALL. E. It is not uncommon to see the absence of CD19 on B-cell lymphoblastic leukemias. 7b. Flow cytometry demonstrates that the patient’s neoplastic cells are of B-cell lineage. Results of the fluorescence in situ hybridization (FISH) studies are shown (Figure 11-5, B). Which one of the following is true? A. The patient’s lesional cells will likely be CD10 positive. B. This particular cytogenetic finding is predictive of a good prognosis. C. Administration of methotrexate is a recognized risk factor for the development of this child’s disease. D. This genetic defect causes promyelocytic differentiation in AML. E. FISH is required to identify this cytogenetic abnormality. 7c. Which one of the following statements regarding the molecular characteristics of B-ALL is true? B. The BCR/ABL translocation that can occur in B-ALL is molecularly identical to the translocation seen in chronic myeloid leukemia (CML). C. A karyotype characterized by fewer than 40 chromosomes confers a favorable prognosis. D. The presence of the BCR/ABL translocation confers a distinctly poor prognosis. E. A translocation between chromosomes 12 and 21 is prognostically unfavorable. 8. A 74-year-old woman with a new diagnosis of leukemia undergoes molecular testing to assess her prognosis. Which one of the following alterations associated with the blast morphology seen in Figure 11-6 has the worst prognosis? A. Core-binding factor β-subunit myosin heavy-chain 11 (CBFB-MYH11) fusion. B. CEBPA (CCAAT/enhancer-binding protein) mutation. C. FLT3 mutation D. NPM1 mutation. E. RUNX1-RUNX1T1 fusion. 9. A 68-year-old man is diagnosed with leukemia. His peripheral blood and bone marrow aspirates smears are shown in Figure 11-7, A and B, respectively. Which one of the following good prognostic cytogenetic abnormalities is most likely present in this patient? B. t(8;21). C. t(9;11). D. t(15;17). E. inv(16). 10. A 4-month-old infant girl is noted by her parents to be lethargic with abdominal distention. Physical examination by her physician reveals hepatomegaly and splenomegaly, and a complete blood cell count shows anemia (hemoglobin, 9.2 g/dL; reference range, 10.0 to 14.0 g/dL) and thrombocytopenia (76 × 109/L; reference range, 150 to 450 × 109/L). Bone marrow examination is performed and reveals 24% blasts. A representative blast is shown in Figure 11-8. Which one of the following genetic abnormalities does this patient most likely have? B. t(8;21). C. t(15;17). D. inv(16). E. + 21. 11. A 7-year-old boy is taken to the pediatrician’s office by his parents with swollen lymph nodes in his neck and axillae and persistent fever over the past several weeks. In addition, the child complains that he often wakes during the night to find his pillow soaking wet from sweat. A section from an excisional biopsy of a lymph node is shown in Figure 11-9. No B-cell markers are positive when immunohistochemistry is performed. Which one of the following statements is true? B. Immunohistochemistry for CD30 is expected to be negative. C. This disease is almost always driven by Epstein-Barr virus (EBV). D. IgH (immunoglobulin heavy locus) is almost always rearranged in this disease. E. The cells in this disease typically express epithelial membrane antigen (EMA). 12. A 42-year-old Jamaican woman presents to her physician with a persistent nonproductive cough, recent 8-lb weight loss, and night sweats. Her pulse and respiratory rate are elevated, and her oxygen saturation is measured at 86%. She is sent to the emergency department for evaluation. A chest radiograph demonstrates diffuse granular opacities consistent with Pneumocystis jiroveci pneumonia (PCP). A complete blood cell count with differential shows a WBC count of 23 × 109/L (reference range, 6.0 to 11.0 × 109/L) and absolute lymphocytosis with “many atypical cells.” She is found to have splenomegaly and scattered nodules on her lower posterior trunk. The patient’s family history reveals that her mother “can’t use her legs at all.” The patient’s peripheral smear is shown in Figure 11-10. Which one of the following statements is true? A. The patient will likely have an elevated calcium level when serum chemistries are evaluated. B. With aggressive treatment and bone marrow transplantation, the patient’s prognosis is good. C. The patient’s disease is related to a chronic parasitic infection that is endemic in the Caribbean islands. D. The atypical cells will most likely be CD16 and CD56 positive. E. The patient is immunocompromised because her bone marrow is likely replaced by neoplastic cells. 13. A 16-year-old boy is taken to the emergency department with abdominal pain that has worsened over the past week. He complains of abdominal tenderness and reveals that he has not had a bowel movement for the past 4 days. The patient is sent for a computed tomography (CT) scan of the abdomen, which shows a large abdominal mass and dilated loops of bowel suggestive of obstruction. He is scheduled for exploratory laparotomy, and his preoperative peripheral smear is shown in Figure 11-11. Which one of the following is true regarding the patient’s diagnosis? A. This disease is almost always associated with EBV in the Western world. B. Phenotypic analysis will likely show that these cells are CD10 negative. C. A histologic hallmark of this disease is the absence of tingible body macrophages. D. Despite aggressive treatment with chemotherapy, the long-term prognosis is poor. E. This disease usually involves the fusion of one of several genes to chromosome 8. 14. A 32-year-old woman develops multiple enlarged cervical lymph nodes and presents to her physician. He decides to send her for an excisional biopsy of one of the nodes, as shown in Figure 11-12. Which one of the following infections is most often linked to this patient’s adenopathy? B. EBV. C. Hepatitis C virus (HCV) D. Human herpesvirus 8 (HHV-8). E. Human T-lymphotropic virus 1 (HTLV-1). A 63-year-old woman with hypertension and hyperlipidemia presents to her primary care physician for a routine checkup. She feels well and has well-controlled blood pressure and lipid levels; however, a complete blood cell count shows mild leukocytosis (WBC count, 13.0 × 109/L; reference range, 3.54 to 9.06 × 109/L) with atypical lymphocytosis (60% neutrophils, 5% lymphocytes, 30% atypical lymphocytes, 3% monocytes, and 2% eosinophils; reference ranges, 40% to 70% neutrophils, 20% to 50% lymphocytes, 2% to 8% monocytes, 0% to 6% eosinophils, 1% to 2% basophils). Her physician chooses to send a sample for flow cytometry evaluation. Representative flow cytometry results are shown in Figure 11-13. Use this scenario to answer the following four questions. 15a. Which one of the following is the most appropriate diagnosis for this patient? A. B-cell prolymphocytic leukemia (B-PLL). B. Chronic lymphocytic leukemia (CLL). C. Hairy cell leukemia (HCL). D. Monoclonal B-cell lymphocytosis (MBL). E. Reactive lymphocytosis (RL). 15b. The patient receives appropriate therapy and follow-up for her diagnosis but returns over the following year with increasing leukocytosis (WBC count ≥ 52 × 109/L for 4 months; reference range, 3.54 to 9.06 × 109/L) and increasing atypical lymphocytosis (11% neutrophils, 12% lymphocytes, 74% atypical lymphocytes, 2% monocytes, and 1% eosinophils; reference ranges, 40% to 70% neutrophils, 20% to 50% lymphocytes, 2% to 8% monocytes, 0% to 6% eosinophils, 1% to 2% basophils). Flow cytometry shows the same immunoprofile noted previously. A peripheral blood smear at this time is shown (Figure 11-13, D). Which one of the following is the most appropriate diagnosis for this patient at this time? B. CLL. C. HCL. D. Large granular lymphocytic leukemia (LGL leukemia). E. MBL. 15c. Which one of the following factors is associated with the best prognosis in this disease? B. Deletion 13q. C. Deletion 17p. D. Germline IGHV (immunoglobulin heavy variable cluster) gene. E. ZAP-70 (ζ-chain [T-cell receptor]-associated kinase 70) expression. 15d. Several years later, this patient’s disease progresses again and she is noted to have several enlarged lymph nodes. Eight months after this development, the patient dies. Which one of the following is the most likely diagnosis for this patient’s transformed disease? B. Classic Hodgkin’s lymphoma (CHL). C. Diffuse large B-cell lymphoma (DLBCL). D. LGL leukemia. E. Small lymphocytic lymphoma (SLL). 16a. A 62-year-old man presents to his primary care physician with 2 months of fatigue and a 5-lb weight loss. His physician orders a complete blood cell count with differential and a bone marrow biopsy. His peripheral blood smear and bone marrow aspirate are shown in Figure 11-14. Which one of the following genetic/karyotypic abnormalities is diagnostic of the disease from which this patient most likely suffers? B. Translocation t(9;22)(q34;q11.2). C. Trisomy 8. D. Translocation t(9;14)(p13;q32). E. Deletion 5q. 16b. The patient is treated with targeted therapy for the genetic alteration noted previously and enters clinical remission. After 5 years, the patient begins to feel fatigued again and notes abdominal fullness. When he returns to his primary care physician, he is found to have splenomegaly and a complete cell blood count shows anemia (10.2 g/dL; reference range, 13.3 to 16.2 g/dL), thrombocytopenia (99 × 109/L; reference range, 165 to 415 × 109/L), and leukocytosis (53 × 109/L; reference range, 3.54 to 9.06 × 109/L), with a marked left shift (18% myeloblasts). Which one of the following is the patient’s diagnosis at this time? A. AML with recurrent genetic abnormalities. B. t-AML. C. CML, AP. D. MDS/RAEB-II. E. BPDC. 16c. Which one of the following factors is most important in this patient’s prognosis? B. Degree of bone marrow fibrosis. C. Presence of cytogenetic abnormalities. D. Response to targeted therapy. E. Transfusion dependence. 17. A 64-year-old man presents to his primary care physician with a rash that developed over the past several months. The rash is a generalized erythroderma that is intensely and persistently pruritic. Physical examination reveals hepatosplenomegaly and diffuse lymphadenopathy. The patient is sent for routine blood work, and he is referred to a dermatologist for further evaluation. An image from the patient’s peripheral blood smear is shown in Figure 11-15. Which one of the following statements is true? A. A biopsy of this patient’s rash will show epidermal involvement by the lesional cells. B. The lesional cells will have an NK phenotype. C. Peripheral blood involvement of cutaneous lesions of this type is a strong indication that the bone marrow will also be involved. D. Prognosis is affected by the degree of lymph node and/or peripheral blood involvement by the lesional cells. E. With aggressive treatment, this patient has an excellent prognosis. 18. Blood is taken from a healthy patient and flow cytometry is performed on the sample shown in Figure 11-16. Which one of the following statements is true? A. Chloroacetate esterase (CAE) positivity is specific for the cells that are found in gate A. B. The cells in gate B will be negative when stained with naphthyl acetate esterase staining. C. The cells in gate C will stain positive with Sudan Black B. D. Myeloperoxidase staining is nearly 100% specific for the cells that are found in gate A. E. The cells in gate C will be reactive when treated with nitroblue-tetrazolium (NBT). 19. A 72-year-old woman sees her primary care doctor because she noticed a lump in her right axilla. She also complains of night sweats and fatigue over a period of 1 to 2 months. The mass is excised, and the biopsy specimen is shown in Figure 11-17. Which one of the following statements is true? A. Necrosis is an uncommon feature in lymph node biopsy of a patient with this disease. B. CD10- or bcl6-positivity is prognostically unfavorable. C. The bone marrow is almost always involved when this disease is diagnosed. D. A gene normally expressed in germinal centers is the most common cytogenetic abnormality. E. The proliferation index (assessed by Ki-67 positivity) is almost universally greater than 90%. 20. A 23-year-old man is taken by ambulance to the trauma center with third-degree burns covering 30% of his body. His peripheral smear is shown in Figure 11-18. Which one of the following statements is true regarding the patient’s neutrophilic inclusions? A. These inclusions are rarely seen in conjunction with toxic granulation. B. These inclusions demonstrate piled-up fragments of mitochondrial remnants on electron microscopy. C. These inclusions will be destroyed by treatment with ribonuclease. D. These inclusions are a sign of a relatively slow turnover of neutrophils compared with systemic demands. E. These inclusions are more likely to be identified evenly distributed through the cell as opposed to on the periphery. 21. A 6-year-old girl from South Africa presents to the emergency department with altered mental status. Neurologic examination reveals focal deficits including right limb paralysis. Skin examination reveals petechiae on the patient’s truck and several bruises on the patient’s limbs, in addition to café-au-lait spots. She is noted to be short for her age, and truncal dissymmetry suggestive of scoliosis is observed. Laboratory testing is performed, and her complete blood count with differential is shown in Table 11-2. Which one of the following is true about the patient’s most likely diagnosis? B. Patients with this disease will have positive chromosome breakage studies. C. Most patients with this condition never experience aplastic anemia. D. Patients with this disorder are no more likely to develop a hematopoietic malignancy. E. A single gene is implicated in this disease. 22. A 68-year-old man sees his primary doctor after noticing a “lump in his armpit.” On examination, he is found to have diffuse adenopathy. The patient is sent for laboratory testing and a CT scan of the head/neck and chest. You are the pathologist covering the hematology laboratory and are asked to review the patient’s peripheral smear (Figure 11-19). Which one of the following statements is true regarding the patient’s condition? A. The patient’s flow cytometry will likely show a T-cell phenotype for the abnormal cells seen. B. Lymph node versus bone marrow grade discordance (high versus low) suggests a slightly better prognosis than high-grade concordance. C. The patient’s disease is associated with a translocation involving a cell cycle regulator gene. D. Bone marrow involvement is commonly found in this patient’s disease and is typically characterized by a diffuse pattern of infiltration. E. The expression of CD10 is stronger in higher-grade lesions of this type. 23. A 68-year-old man goes to see his primary care doctor to be evaluated for progressive weakness and decreased exercise tolerance. Review of systems reveals that he is not eating as much as he normally does and that he feels full after eating only a small portion of the food on his plate. Physical examination shows splenomegaly, petechial bruises, and purpura on his lower limbs bilaterally. The patient is sent to have blood work and imaging studies. He is found to be pancytopenic. A bone marrow biopsy is subsequently performed. His peripheral smear and bone marrow biopsy are shown in Figure 11-20. Which one of the following statements is true? A. Cytogenetic studies play no role in prognosis in this disease. B. The villi that are seen on the lesional cells are characteristically polar. C. Marrow fibrosis is not a common feature in this disease. D. Monocytosis is a common feature in this disease. E. Diffuse adenopathy is usually present in patients with this disease. 24. A 5-week-old newborn boy is taken to the emergency department with yellow skin and eyes and increasing somnolence. He has had intermittent fever over the past several days. On physical examination, the baby is found to have hepatosplenomegaly. A complete blood cell count shows profound anemia and thrombocytopenia. In addition, his serum aspartate aminotransferase (AST), alanine aminotransferase (ALT), and total and direct bilirubin are all found to be elevated. Further history reveals that the infant’s parents are first cousins. The patient undergoes a bone marrow biopsy, and the Giemsa-Wright–stained aspirate is shown in Figure 11-21. Which one of the following statements is true? A. The main immunologic defect in this disease involves CD4 + lymphocytes. B. Hypoferritinemia is characteristic in this disease. C. Hemophagocytosis is necessary and sufficient to make this diagnosis. D. High levels of soluble CD25 (sCD25) are highly specific for this disease. E. The quantity of CD16 +/CD56 + cells is characteristically reduced in this disease. 25. A 40-year-old man presents to his physician with fevers and weight loss. Physical examination reveals cervical lymphadenopathy; the lymph node biopsy is shown in Figure 11-22. Which one of the following immunoprofiles is most consistent with the large cells in the above lymph node infiltrate and has the best overall prognosis? A. CD15 + CD20 − CD30 + CD45 − PAX5 + LMP1 + . B. CD15 − CD20 + CD30 + CD45 + PAX5 + LMP1 + . C. CD15 − CD20 + CD30 − CD45 + PAX5 + LMP1 − . D. CD15 − CD20 − CD30 + CD45 + PAX5 + LMP1 + . E. CD15 − CD20 + CD30 − CD45 − PAX5 − LMP1 − . 26. A 19-year-old Japanese immigrant presents to her physician with unilateral posterior cervical lymphadenopathy that she initially noticed about 2 weeks before, along with intermittent fevers, chills, and myalgias. An autoimmune workup is negative. The lymph node is excised, and the hematoxylin and eosin (H&E)-stained slide is shown in Figure 11-23. Which one of the following statements is true? A. An abundance of plasma cells is expected to be identified in this biopsy. B. The absence of neutrophils is characteristic of this disease. C. This patient’s clinical course will likely be characterized by lifelong intermittent disease. D. Human herpesvirus-6 (HHV-6) is the causative agent in this disease. E. CD4+ cells are the predominant cells in affected lymph nodes. 27. A 68-year-old man comes to his primary care physician for a routine checkup. The patient complains of a generalized pruritic rash and recent weight loss. In addition, he says that he often has hot flashes associated with facial redness. Physical examination reveals that a wheal develops when the affected skin is scratched with the wooden end of a cotton swab. Mild splenomegaly is noted; however, no lymphadenopathy or hepatomegaly is appreciated. Blood work reveals leukocytosis with eosinophila, mild anemia, and mild thrombocytosis. The patient is sent for a bone marrow biopsy; a Giemsa-Wright–stained slide of the aspirate is shown in Figure 11-24. Which one of the following statements is true? A. These findings are not associated with hematopoietic disease. B. CD117 positivity in the cells seen in the patient’s bone marrow biopsy is evidence of neoplasia. C. Elevated histamine levels are highly specific for the patient’s condition. D. Fibrosis is an uncommon feature in the bone marrow when this disease is identified. E. The patient’s serum tryptase level will likely be elevated. 28. You are the clinical hematopathologist in the core laboratory facility, and you receive the preoperative complete blood cell count and accompanying peripheral blood smear shown in Figure 11-25. The patient is a 16-year-old deaf boy who is accompanied by his adoptive parents. He was initially found to have proteinuria at the age of 12 years, and his renal function has steadily declined over the past several years. He is now scheduled for a dialysis catheter placement. Which one of the following statements is true? B. The patient has a defect in microtubule polymerization. C. When electron microscopy is performed, the inclusions seen within the cytoplasm of the neutrophils are enriched in degenerated organelles. D. The gene implicated in this patient’s condition is implicated in numerous similar diseases. E. This patient has a lysosomal storage disease. 29a. Which one of the following combinations of factors is most important in predicting the prognosis in this patient? A. Age, bone marrow blast percentage, cytopenias, FLT3 status. B. Age, bone marrow blast percentage, cytopenias, karyotype. C. Age, bone marrow blast percentage, FLT3 status, karyotype. D. Age, cytopenias, FLT3 status, karyotype. E. Bone marrow blast percentage, cytopenias, FLT3 status, karyotype. 29b. Which one of the following genetic changes is associated with the best prognosis in this patient? B. del(5q). C. del(7q). D. + 8. E. i(17q). 29c. The patient is followed for 3 years and treated according to standard of care. At this point, she has required escalating intensity of intervention. A repeat bone marrow biopsy is performed; the aspirate is shown in Figure 11-26, C and D. Which one of the following is the most appropriate diagnosis for this patient at this point? A. Refractory anemia with excess blasts II (RAEB-2). B. Refractory anemia with ringed sideroblasts (RARS). C. Refractory cytopenia with multilineage dysplasia (RCMD). D. Refractory cytopenia with unilineage dysplasia. E. Refractory neutropenia (RN). 30a. A 72-year-old white man presents to his primary care doctor with complaints of increasing shortness of breath and fatigue. Further questioning reveals that the patient has been experiencing worsening pain in his mid and lower back. Laboratory workup demonstrates normocytic anemia, thrombocytopenia, and neutropenia. A bone marrow biopsy and immunohistochemical and in situ hybridization studies are shown in Figure 11-27. Which one of the following statements regarding the patient’s biopsy is likely to be true? A. Expression of CD56 by the lesional cells in the bone marrow biopsy favors a reactive condition. B. A perivascular distribution of suspicious cells is the histologic hallmark of neoplasia in this setting. C. Fibrosis is an uncommon feature in bone marrow biopsies in patients with this disease. D. Sampling error in bone marrow biopsies can be problematic in this disease because the infiltrate is often patchy. E. Cytoplasmic staining for immunoglobulin M (IgM) will likely be positive. 30b. Which one of the following is true regarding this patient’s disease? A. Primary amyloidosis occurs in a minority of cases and is usually associated with κ light chains. B. In the United States, this disease is most commonly seen in African American men. C. The presence of clonal plasma cells comprising less than 10% of nucleated marrow elements rules out this diagnosis. D. Decreased β2-microglobulin is prognostically unfavorable. E. The absence of a paraprotein on serum protein electrophoresis indicates the patient likely has a nonsecretory form of the disease. 30c. Which one of the following statements is true regarding the cytogenetics of this patient’s disease? B. Cases with a hyperdiploid genotype characteristically contain gains in even-numbered chromosomes. C. The t(11;14) induces constitutive tyrosine kinase activity and unregulated cell proliferation. D. Cytogenetics is of limited use in providing clinically prognostic information. E. 17p13 deletion is prognostically unfavorable, with a median survival of about 1 year. A 73-year-old woman presents to her physician with persistent headaches and dizziness. Her physical examination is notable for hypertension and splenomegaly. Her complete blood cell count is abnormal and a bone marrow biopsy is performed. A representative section of the bone marrow biopsy is shown in Figure 11-28, A. Use this scenario to answer the following three questions. 31a. Which one of the following sets of factors is most important to establish a definitive diagnosis for this patient? A. Age, bone marrow cell counts, bone marrow fibrosis, clinical presentation. B. Bone marrow cell counts, bone marrow fibrosis, duration of illness, mutation testing. C. Bone marrow fibrosis, duration of illness, mutation testing, peripheral blood counts. D. Bone marrow cell counts, duration of illness, mutation testing, peripheral blood counts. E. Age, bone marrow cell counts, mutation testing, peripheral blood counts. 31b. The patient also has a complete blood cell count performed, which is notable for elevated hemoglobin (hemoglobin, 17.3 g/dL; reference range, 12.0 to 15.8 g/dL) and elevated platelet count (platelets, 600 × 109/L; reference range, 165 to 415 × 109/L). Her smear is shown in Figure 11-28, B. Another peripheral blood sample is sent for genetic analysis. Which one of the following genetic alterations is most likely to be present? B. FGFR1 translocation. C. JAK2 mutation. D. MPL mutation. E. PDGFRA translocation. 31c. The patient is managed conservatively and after 14 years, her hemoglobin and platelet counts drop and she is able to discontinue therapy. In addition, her peripheral blood smear is notable for 3% blasts and 2% nucleated red blood cells. Which one of the following is the most likely cause of this change? A. Development of pure red cell aplasia. B. Leukemic transformation. C. Progression to spent phase. D. Therapy-induced remission. E. Transformation to MDS. 32. A 6-year-old previously healthy boy acutely develops fever and headache. Within 2 days, he starts to feel fatigued and presents to his pediatrician. A complete blood cell count is notable for anemia (hemoglobin, 8.4 g/dL; reference range, 12.0 to 14.0 g/dL). In the following days, the patient develops a lacy malar rash and remains fatigued. A repeat complete blood cell count 2 weeks later reveals persistent anemia. He undergoes a bone marrow biopsy; the aspirate is shown in Figure 11-29. Which one of the following is the most likely cause of this patient’s illness? B. EBV. C. HHV-6. D. HHV-8. E. Parvovirus B19. 33. A 2-year-old boy with developmental delay and epilepsy presents to his primary care doctor for a checkup. The physician orders a complete blood cell count with differential, and the technologists note the neutrophils shown (Figure 11-30). Which one of the following is the most likely diagnosis in this patient? B. May-Hegglin anomaly. C. MDS. D. Myelokathexis. E. Pelger-Huët anomaly. 34. A 37-year-old African-American man presents with worsening bilateral cervical lymphadenopathy. He had been in his normal state of health until noticing the swollen lymph nodes. He feels well otherwise, and his review of systems is negative. An excisional biopsy is performed; representative sections stained with H&E, CD68, S100, and CD1a are shown in Figure 11-31. Which one of the following statements is true? A. An acid-fast bacillus causes this disease. B. Central nervous system involvement has not been reported for this disease. C. Plasmacytosis is infrequent in this disease. D. Expression of CD1a is concerning for malignancy. E. Hemophagocytosis is characteristic of this disease. 35. A 36-month-old girl is taken to the emergency department after falling on her arm. According to the patient’s parents, she tripped over the household cat and tumbled. She is appropriately sedated and evaluated. A humerus fracture and evidence of osteoporosis are seen on radiographic examination. On further examination, the patient is found to have marked splenomegaly and, to a lesser extent, hepatomegaly. Additionally, her height is less than the fifth percentile for her age and sex. Blood work demonstrates anemia and thrombocytopenia. A hematologist is also called, who recommends a bone marrow examination. Both of the patient’s parents are of Ashkenazi Jewish descent. A Wright-Giemsa–stained aspirate from the patient’s bone marrow is shown in Figure 11-32. Which one of the following statements is true? A. The patient has a histiocytic neoplasm. B. The histiocyte in the figure has accumulated heavy metal. C. Histiocytes with this morphology are diagnostic of this patient’s disease. D. This patient likely has a de novo mutation. E. Enzyme replacement therapy is available for this disease. 36. A 68-year-old man presents to his primary care physician complaining of a 20-lb unintentional weight loss, fevers, and feeling bloated. Physical examination reveals hepatosplenomegaly and prominent left groin lymphadenopathy. A complete blood cell count shows marked lymphocytosis, and a diagnostic excisional lymph node biopsy is performed on one of the inguinal nodes. The node is sent for permanent section and flow cytometry. Representative H&E sections of the lymph node and flow cytometry scatterplots are shown in Figure 11-33. Which one of the following is the most common cytogenetic change accounting for the diagnostic immunostain shown in image I? B. t(8;14)(q24;q32). C. t(9;22)(q34;q11.2). D. t(11;14)(q13;q32). E. t(14;18)(q32;q21). 37. A 63-year-old woman with a strong family history of breast cancer presents to her primary care physician with prominent axillary lymphadenopathy. She is referred for excisional biopsy, and frozen section results are negative for carcinoma. A portion of the lymph node is sent for flow cytometry, and the remaining tissue is sent for permanent section. Representative H&E sections of the lymph node and flow cytometry scatterplots are shown in Figure 11-34. Which one of the following is the most likely diagnosis in this patient? B. Mantle cell lymphoma. C. Marginal zone lymphoma. D. Reactive lymph node. E. SLL. 38. A 34-year-old man presents to his primary care physician with “lumps” in his right groin that have persisted for 4 months. Right inguinal lymphadenopathy without hepatosplenomegaly is noted on physical examination. Test results for sexually transmitted diseases are negative, and the patient undergoes an excisional biopsy. Representative sections of the lymph node are shown in Figure 11-35. The large cells show the following phenotype with immunohistochemical staining: CD15 −, CD20 +, CD30 −, and CD45 +. Which one of the following is the most likely diagnosis in this patient? A. Lymphocyte-depleted Hodgkin lymphoma. B. Lymphocyte-rich Hodgkin lymphoma (LRCHL). C. Mixed-cellularity Hodgkin lymphoma. D. Nodular lymphocyte-predominant Hodgkin lymphoma (NLPHL). E. Nodular sclerosis Hodgkin lymphoma (NSCHL). 39. The bone marrow biopsy specimen shown in Figure 11-36 is from a 68-year-old man with mild anemia (hemoglobin, 12 g/dL; reference range, 10.5 to 13.5 g/dL) with normal leukocyte (5.2 × 109/L; reference range, 6.0 to 11.0 × 109/L) and platelet counts (538 × 109/L, reference range, 130 to 400 × 109/L). Which one of the following is part of the major criteria for the diagnosis of primary myelofibrosis (PMF)? B. Bone marrow fibrosis. C. Increased blast count. D. JAK2 V617F mutation. E. Splenomegaly. A previously healthy 14-month-old boy presents to his primary care doctor with 5 days of fever and lethargy. His vital signs were notable for a body temperature of 102.2°F and heart rate of 140 beats/min. Results of his laboratory testing are shown in Table 11-3. Several members of the patient’s family have had a similar illness, and the family’s pedigree is shown in Figure 11-37. Use this scenario to answer the following two questions. Table 11-3
Hematology
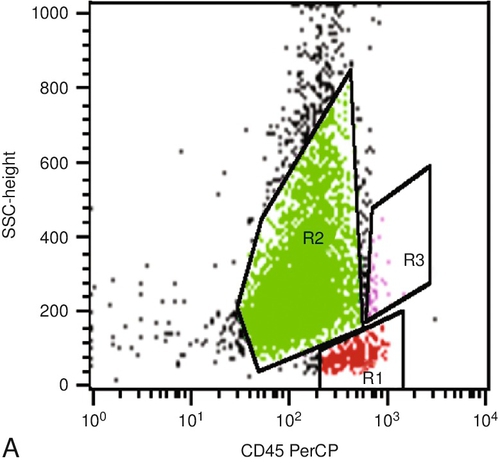
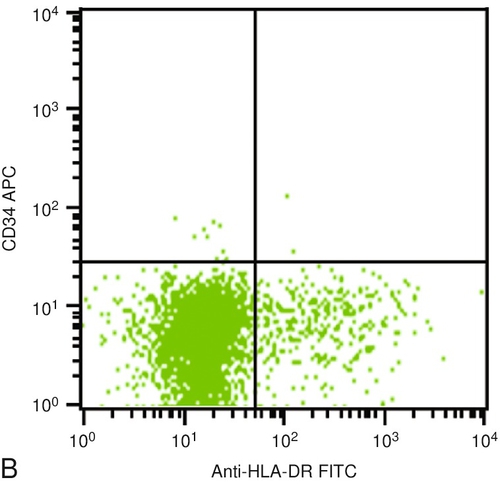
White Blood Cells, Lymph Nodes, and Flow Cytometry
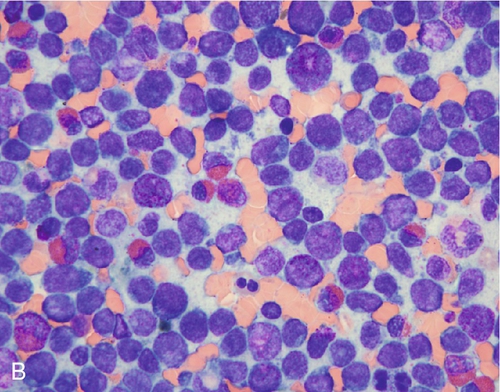
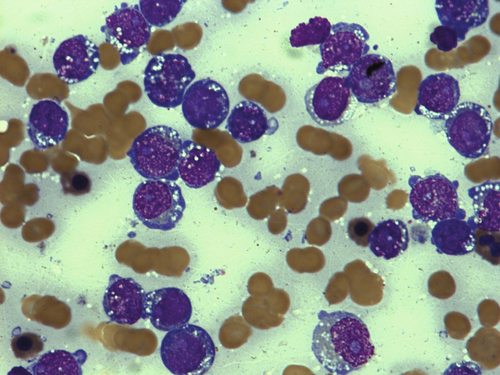
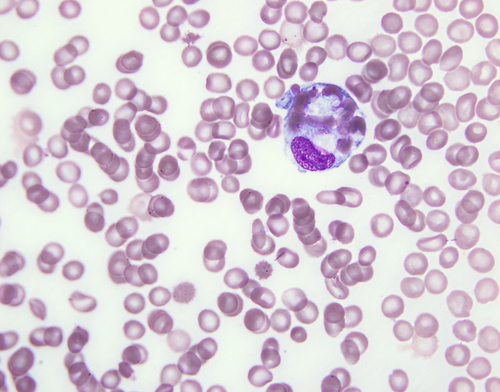
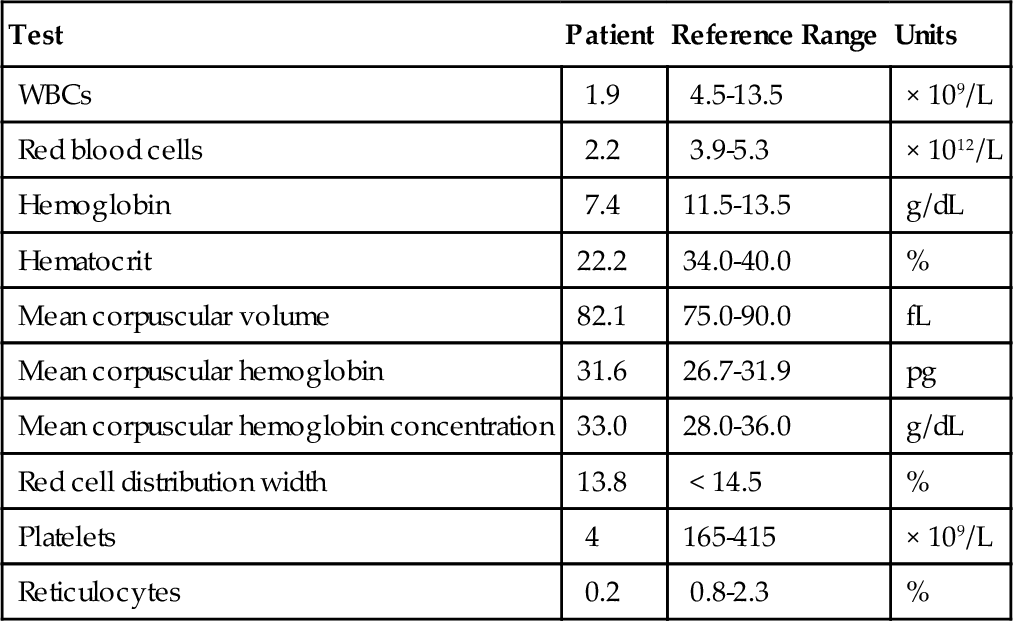
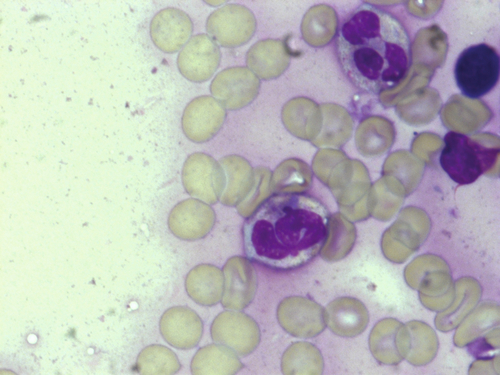
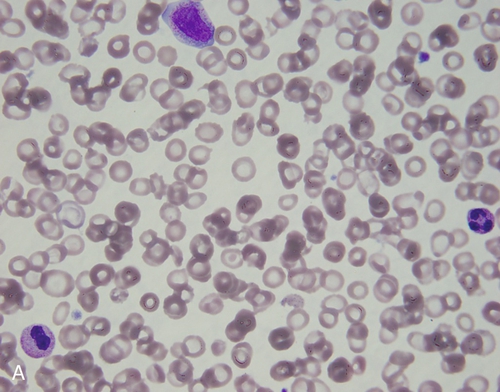
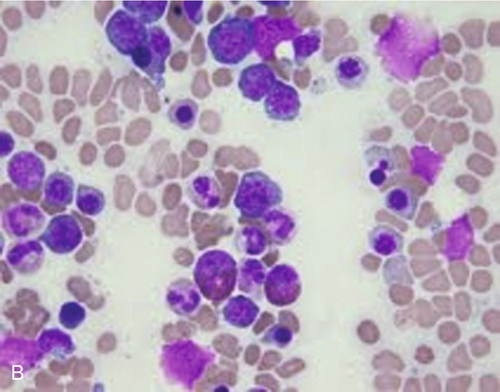
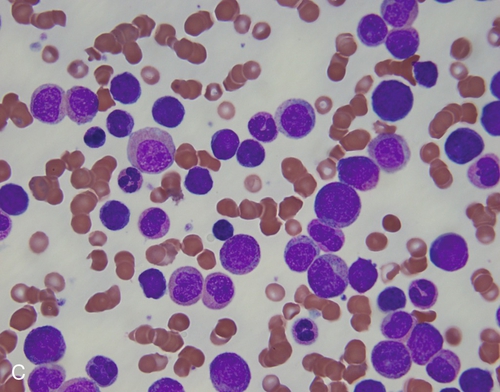
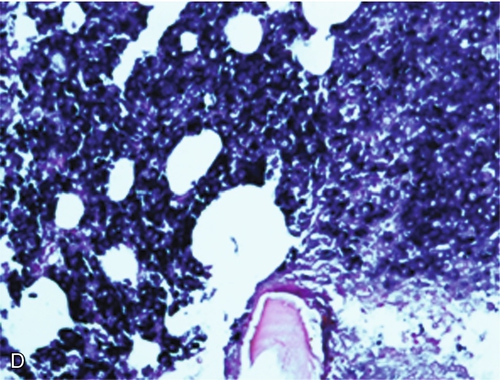
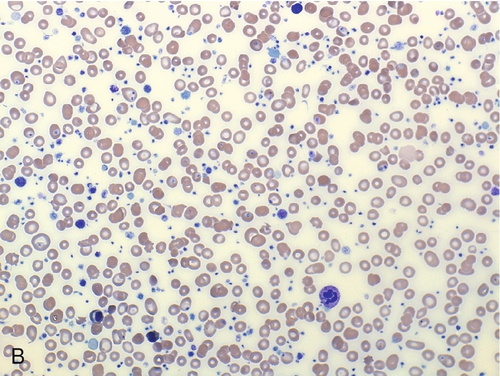
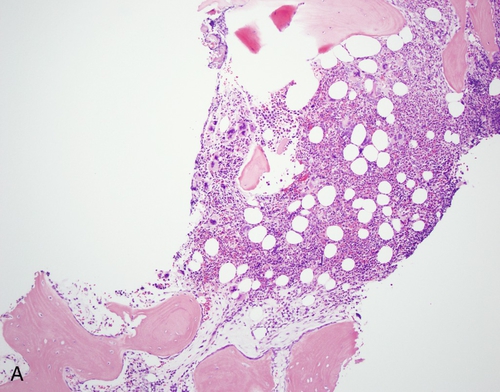
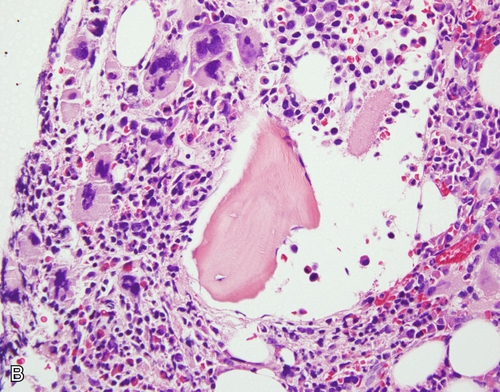
A 78-year-old woman presents to her physician with increasing fatigue. A complete blood cell count is ordered and is notable for pancytopenia. The peripheral smear is shown in Figure 11-26, A). In response to these findings, a bone marrow biopsy is performed; the aspirate smear is shown in Figure 11-26, B. Use this scenario to answer the following three questions.
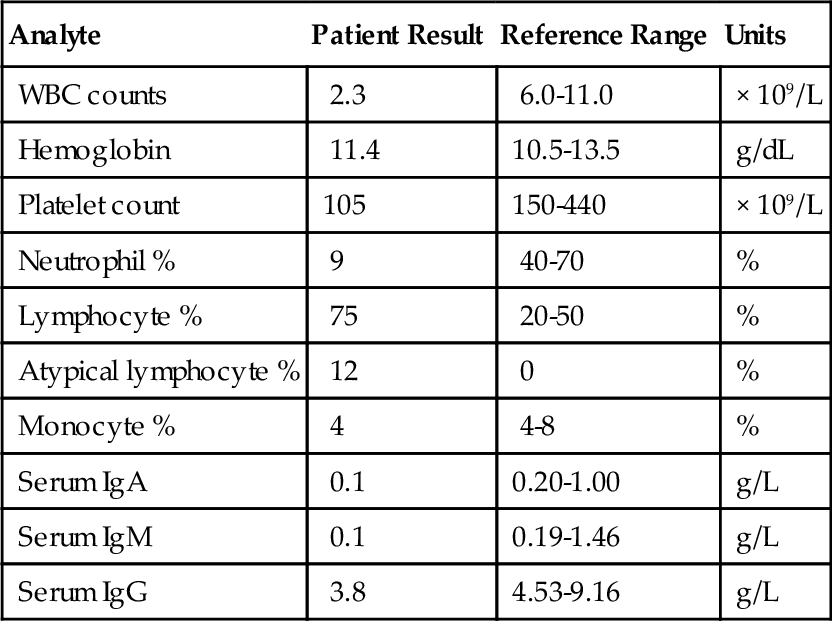
Analyte
Patient Result
Reference Range
Units
WBC counts
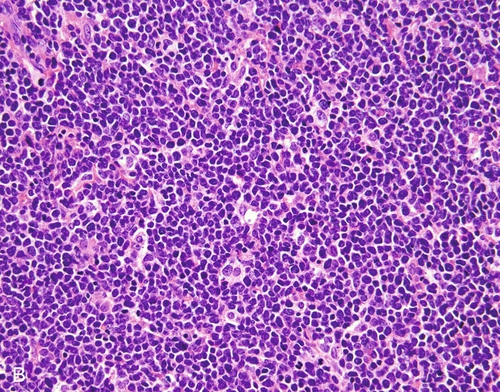
2.3
6.0-11.0
× 109/L
Hemoglobin
11.4
10.5-13.5
g/dL
Platelet count
105
150-440
× 109/L
Neutrophil %
9
40-70
%
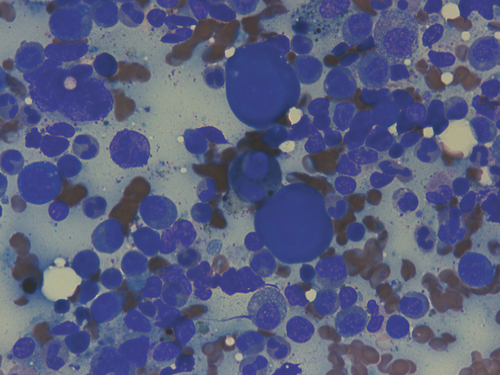
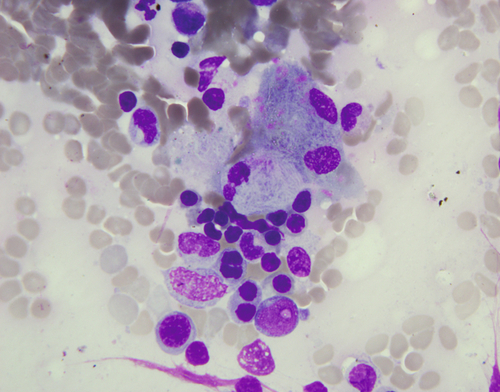
Lymphocyte %
75
20-50
%
Atypical lymphocyte %
12
0
%
Monocyte %
4
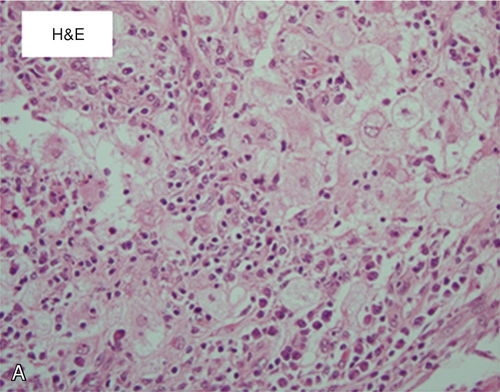
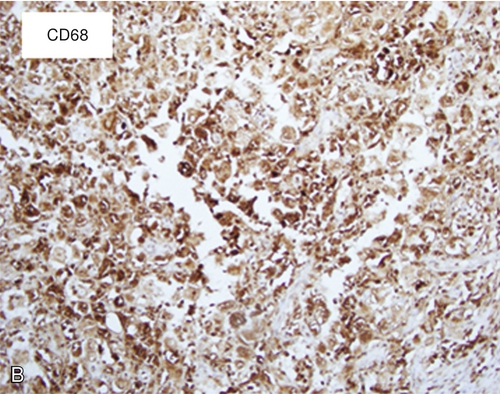
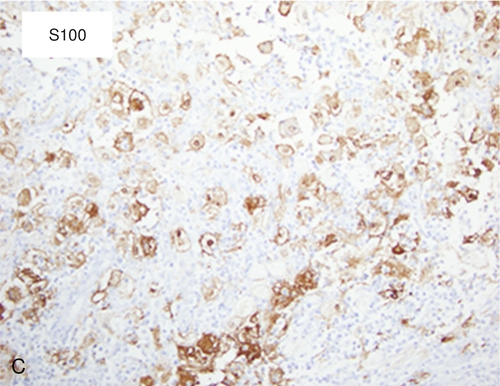
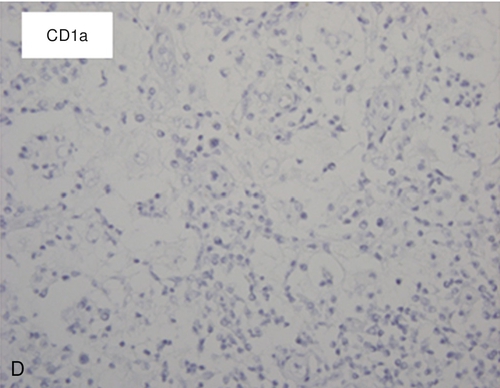
4-8
%
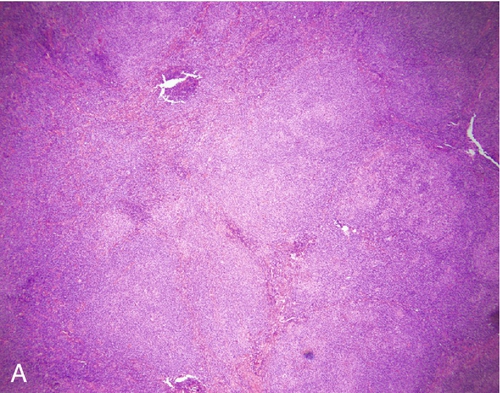
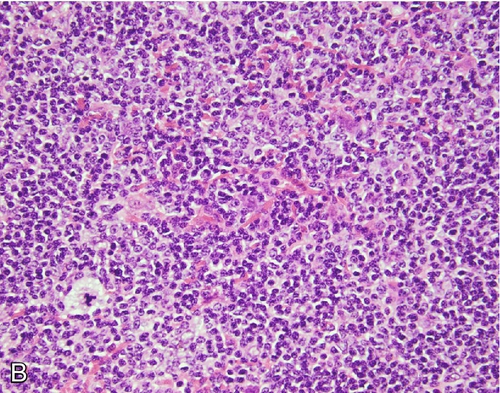
Serum IgA
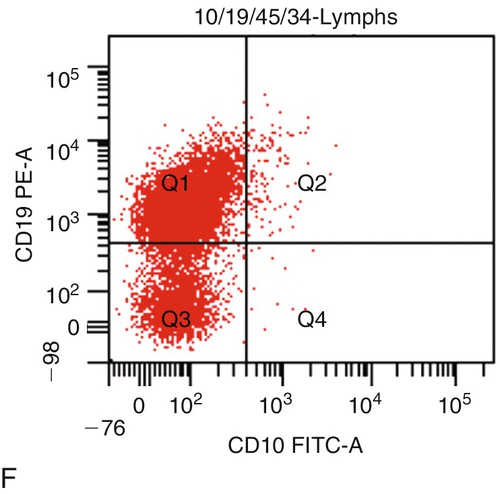
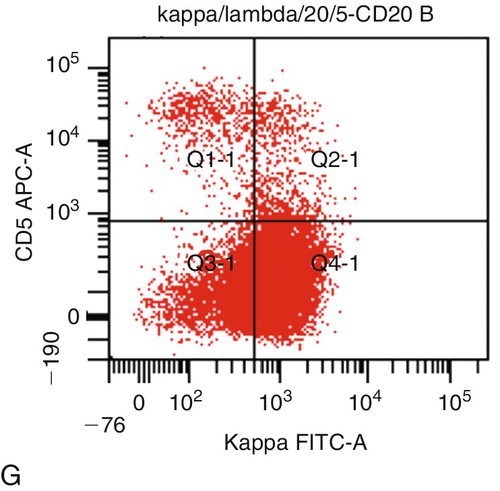
0.1
0.20-1.00
g/L
Serum IgM
0.1
0.19-1.46
g/L
Serum IgG
3.8
4.53-9.16
g/L
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Hematology: White Blood Cells, Lymph Nodes, and Flow Cytometry
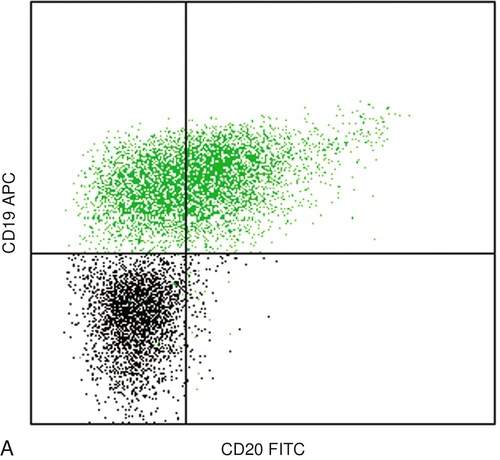
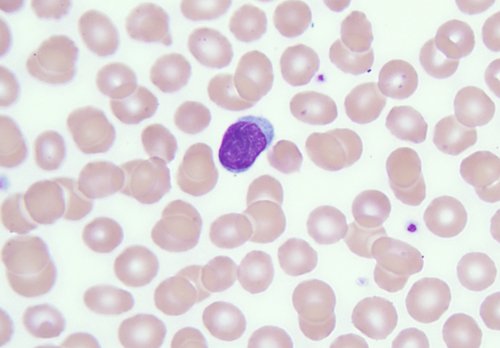
Figure 11-1 Flow cytometric analysis of a peripheral blood sample.
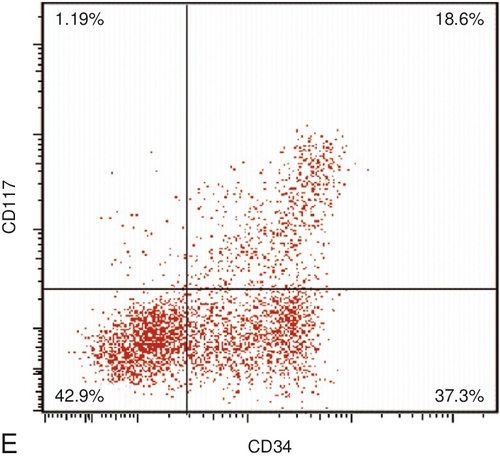
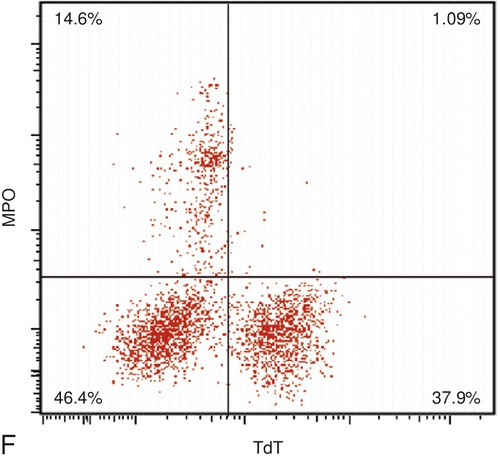
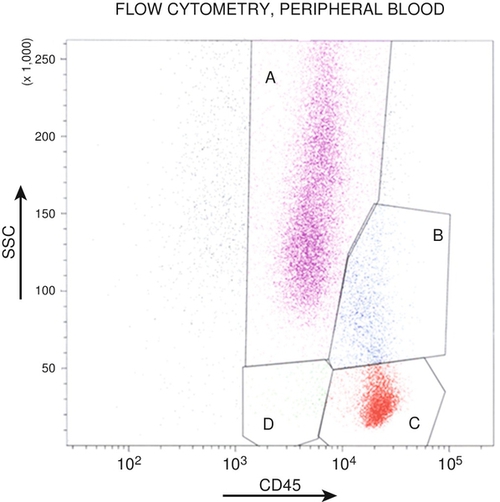
Figure 11-2 Flow cytometric analysis of a bone marrow aspirate sample.
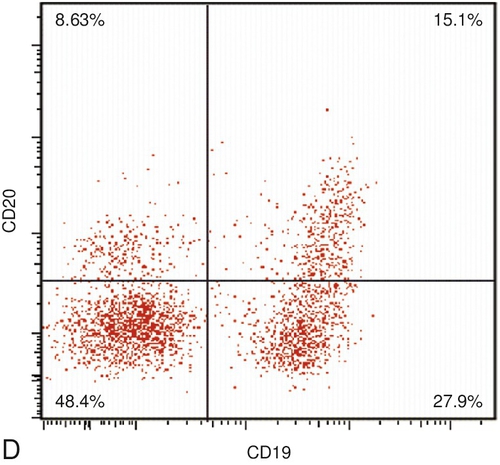
Figure 11-3 Flow cytometric analysis of a peripheral blood sample.
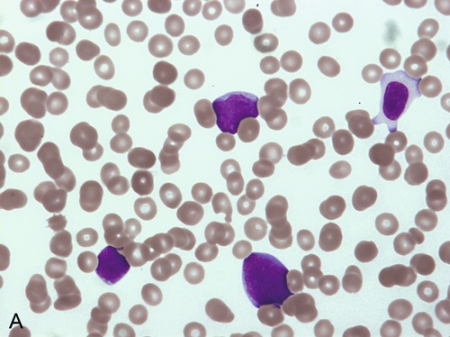
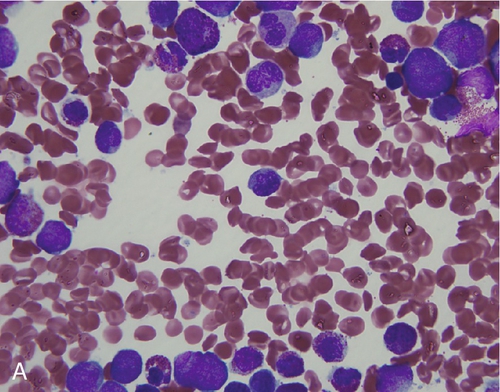
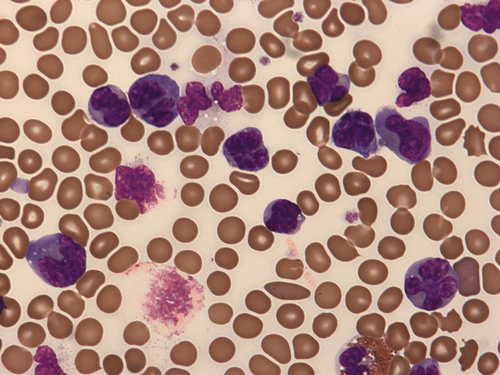
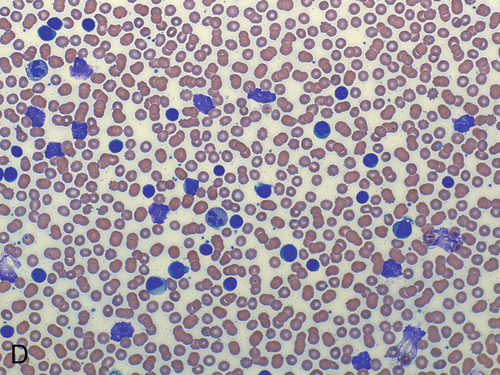
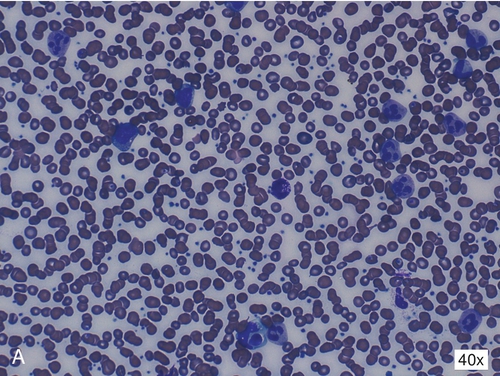
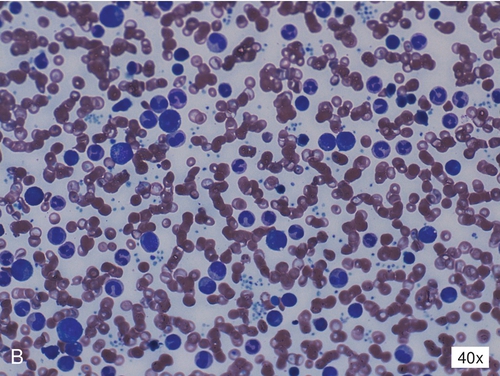
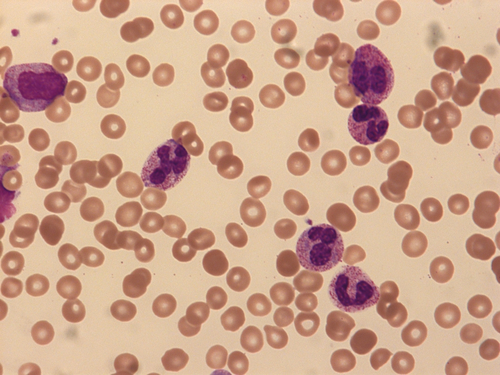
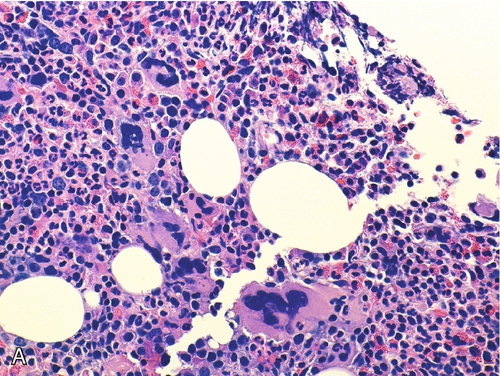
Figure 11-4 A and B, The patient’s peripheral blood smear.
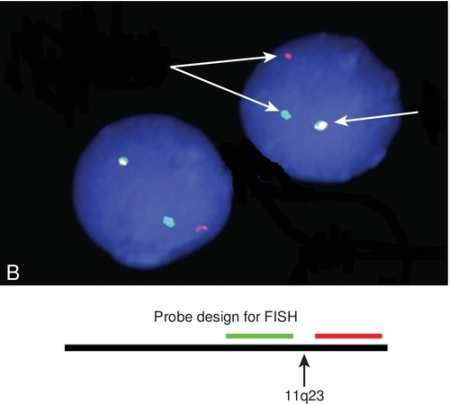
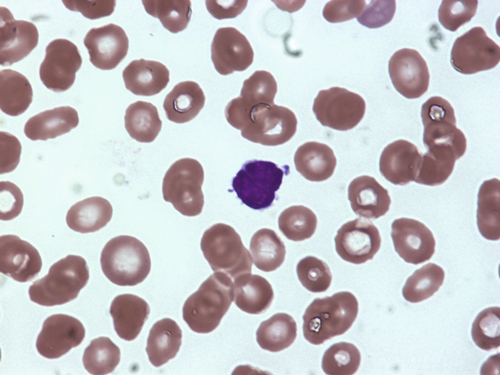
Figure 11-5 A, Peripheral blood smear demonstrating lesional cells. B, FISH using break-apart probes.
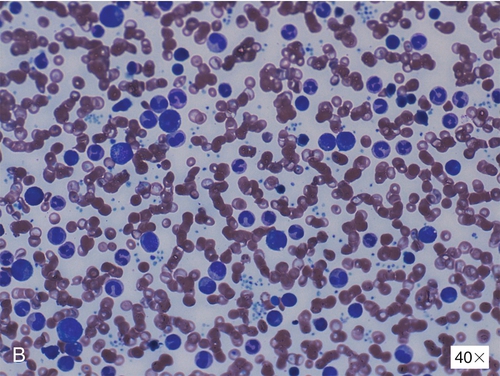
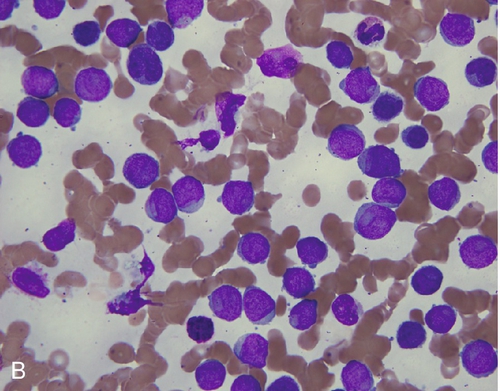
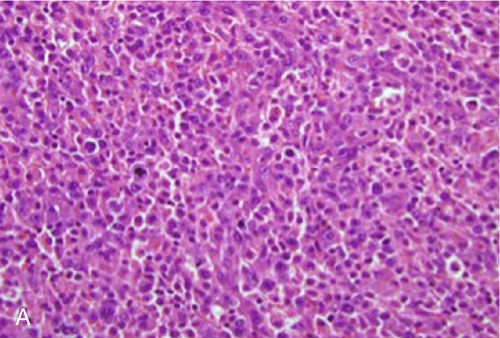
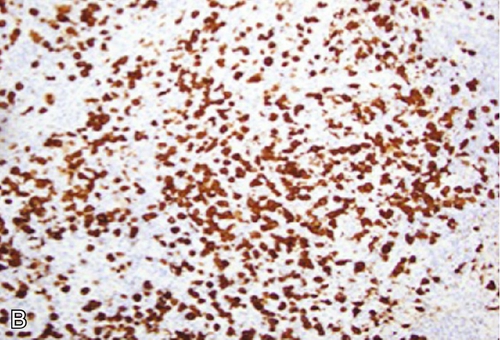
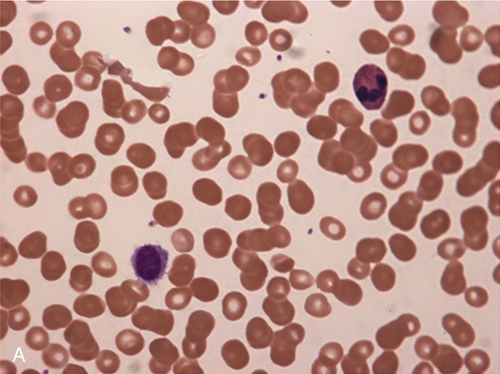
Figure 11-6 A, Wright-Giemsa–stained peripheral blood smear (× 100). B, Wright-Giemsa–stained bone marrow aspirate smear (× 100).
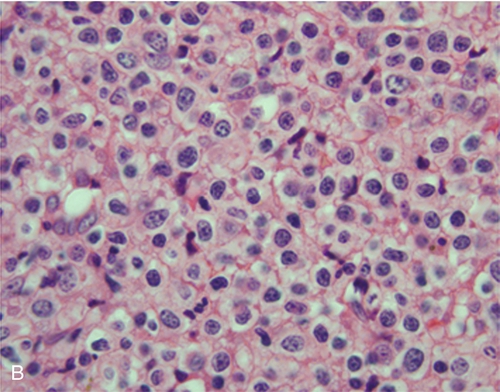
Figure 11-7 A, Wright-Giemsa–stained peripheral blood smear (× 100). B, Wright-Giemsa–stained bone marrow aspirate smear (× 100).
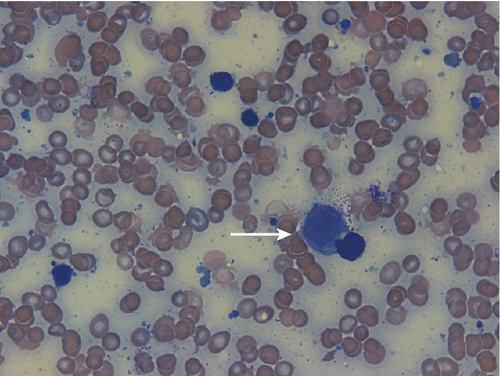
Figure 11-8 A bone marrow aspirate smear. The arrow indicates a representative blast cell identified in the differential count.
Figure 11-9 A and B, H&E-stained lymph node biopsy specimen with accompanying ALK immunohistochemistry.
Figure 11-10 Peripheral blood smear.
Figure 11-11 Peripheral blood smear.
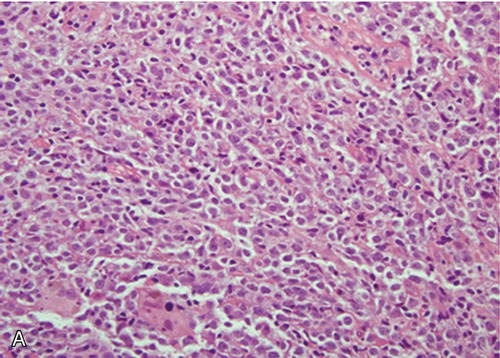
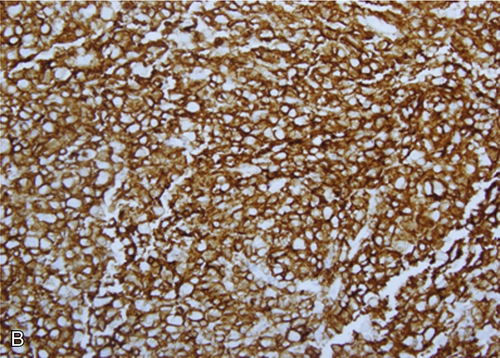
Figure 11-12 A, H&E-stained section of the patient’s lymph node (× 10). B, CD138 immunohistochemical stain of the same lymph node (× 10).
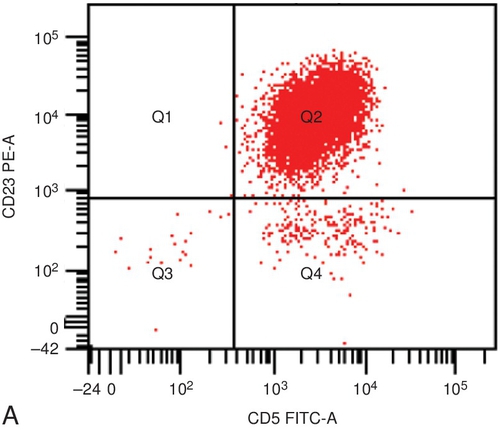
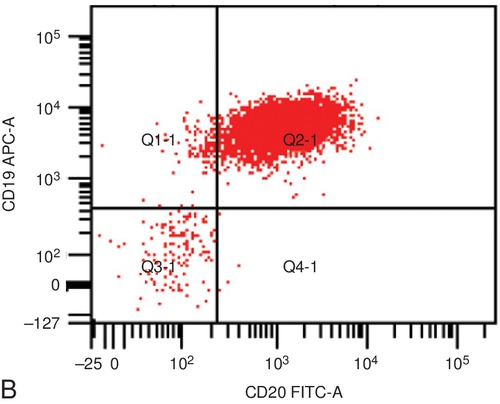
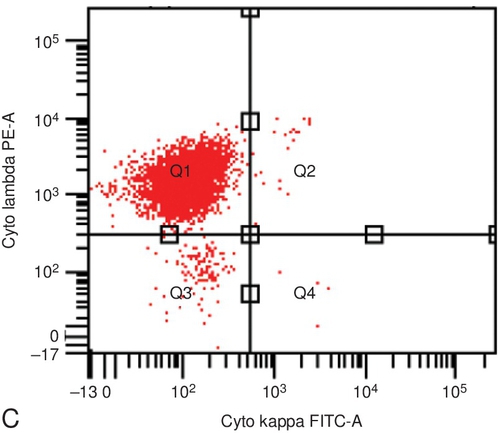
Figure 11-13 Selected flow cytometry scattergrams. A, CD5 and CD23. B, CD20 and CD19. C, κ and λ. D, Wright-Giemsa stain of peripheral blood smear (× 40).
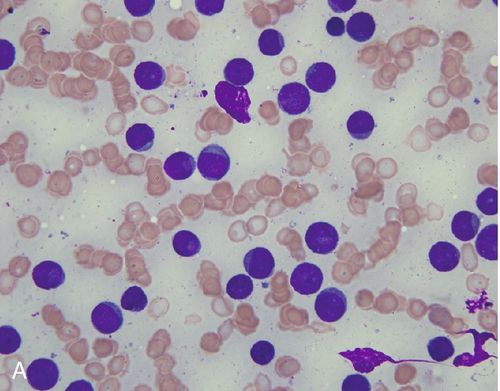
Figure 11-14 A, Peripheral blood smear. B, Bone marrow aspirate smear.
Figure 11-15 Peripheral blood smear with a characteristic cell from the disease described.
Figure 11-16 Scatterplot (CD45 versus side scatter) on a peripheral blood sample from a healthy patient.
Figure 11-17 H&E-stained lymph node biopsy specimen with accompanying CD20 immunohistochemistry.
Figure 11-18 Peripheral blood smear.
Figure 11-19 A peripheral blood smear demonstrating a characteristic lesional cell from the disease described.
Figure 11-20 Wright-Giemsa peripheral blood smear and bone marrow biopsy specimen.
Figure 11-21 Bone marrow aspirate smear.
Figure 11-22 H&E-stained slide of a cervical lymph node.
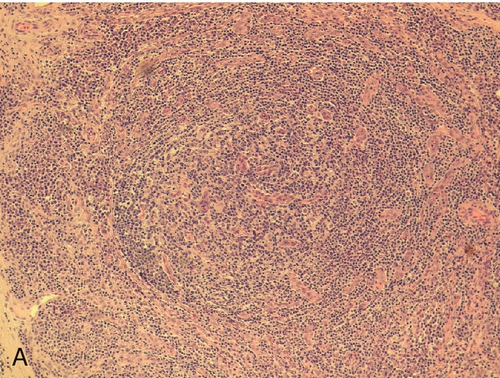
Figure 11-23 H&E-stained lymph node biopsy specimen.
Figure 11-24 Giemsa-Wright–stained slide of bone marrow aspirate.
Figure 11-25 Neutrophil found in the peripheral blood smear.
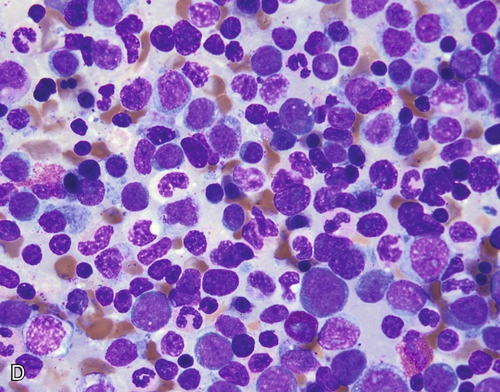
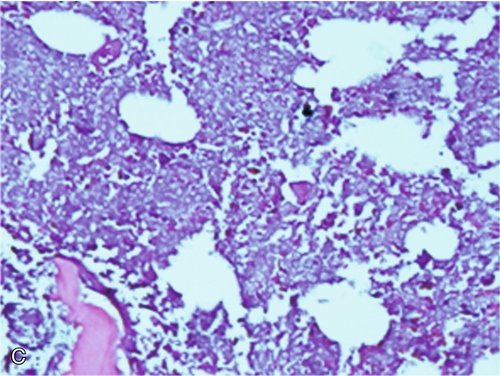
Figure 11-26 A, Wright-Giemsa–stained peripheral blood smear. B, Wright-Giemsa–stained bone marrow aspirate smear. C, Wright-Giemsa–stained peripheral blood smear. D, Wright-Giemsa–stained bone marrow aspirate smear.
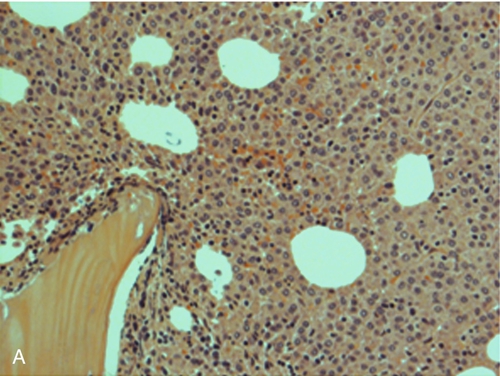
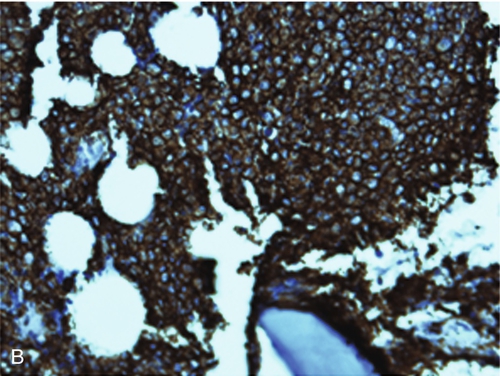
Figure 11-27 H&E-stained bone marrow biopsy specimen with accompanying CD138 immunohistochemistry and κ/λ in situ hybridization.
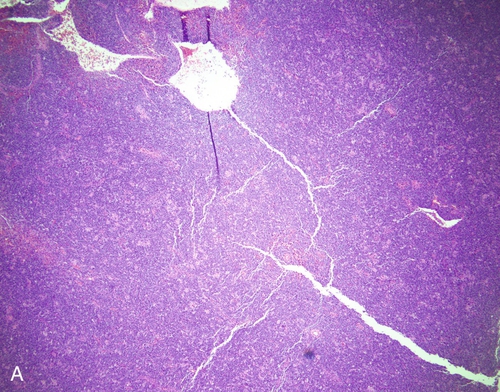
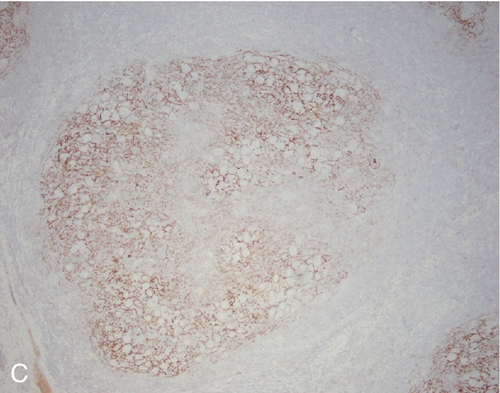
Figure 11-28 A. H&E-stained bone marrow trephine biopsy specimen (× 40). B, Wright-Giemsa–stained peripheral blood smear (× 40).
Figure 11-29 Bone marrow aspirate smear (× 63).
Figure 11-30 Representative field of a Wright-Giemsa–stained peripheral blood smear (× 40).
Figure 11-31 A, H&E-stained lymph node biopsy specimen. B, Lymph node biopsy specimen stained with CD68. C, Lymph node biopsy specimen stained with S100. D, Lymph node biopsy specimen stained with CD1a.
Figure 11-32 Wright-Giemsa–stained bone marrow aspirate smear.
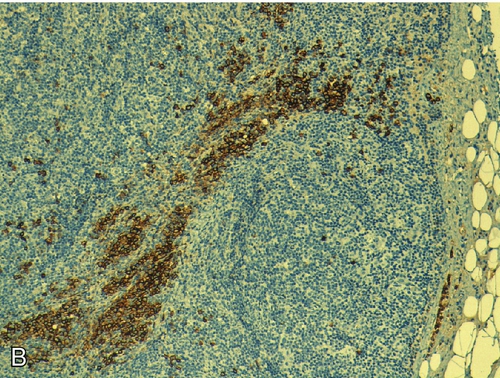
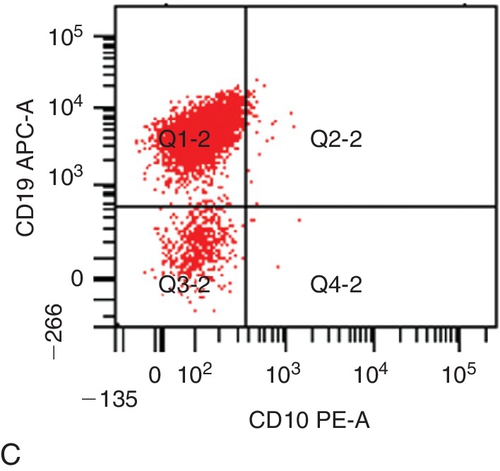
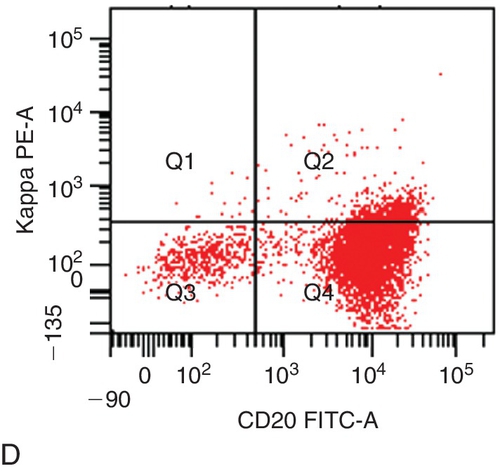
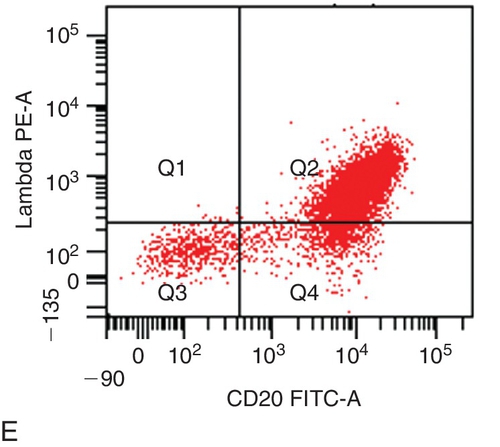
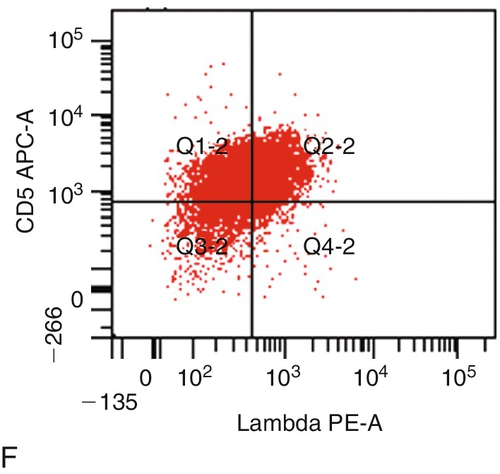
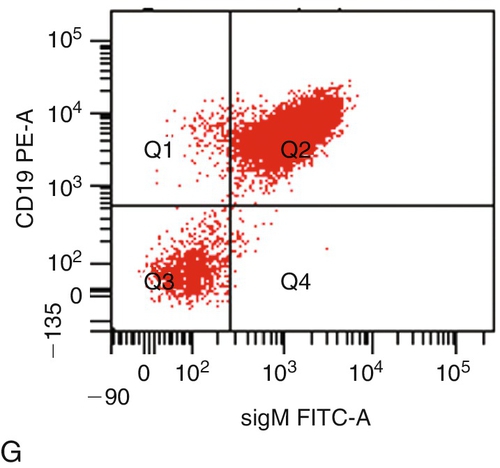
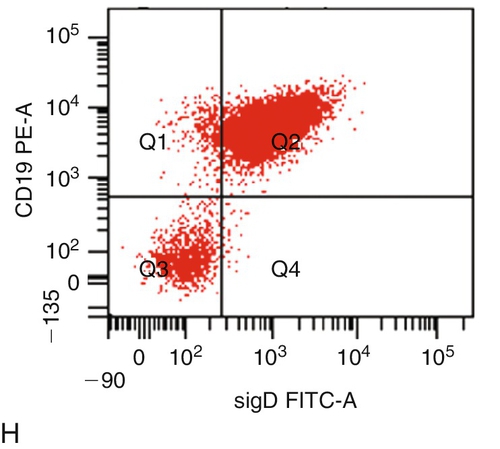
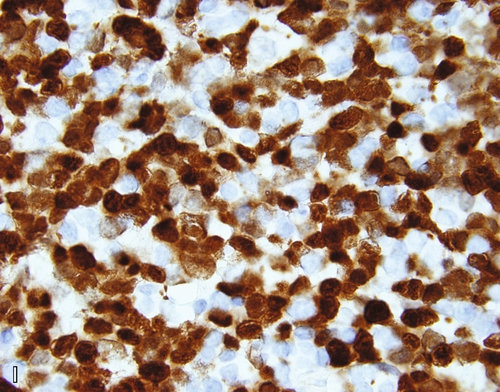
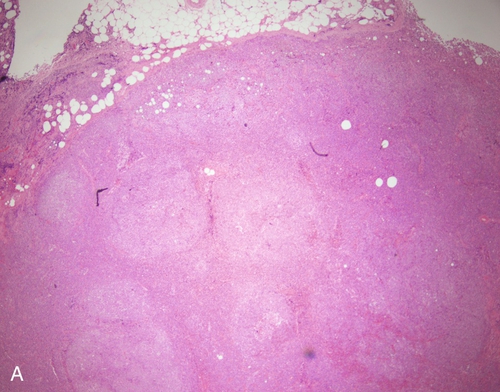
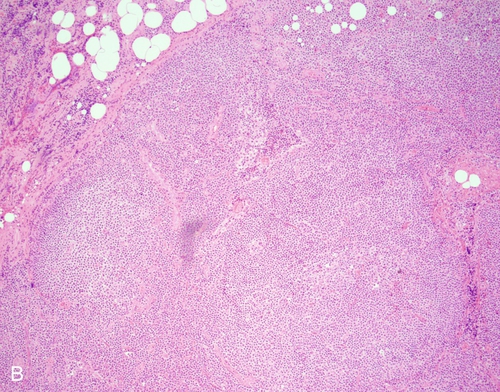
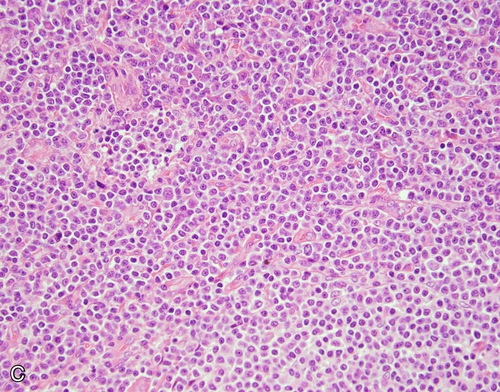
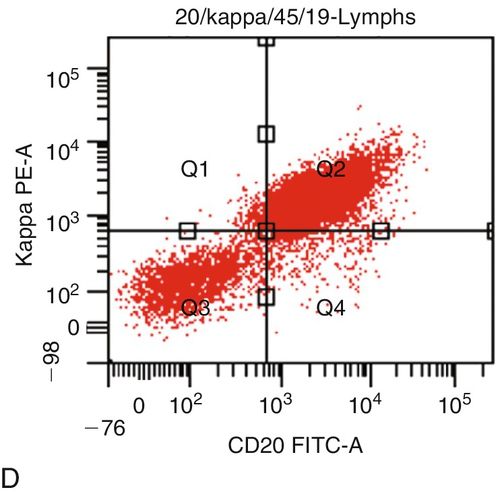
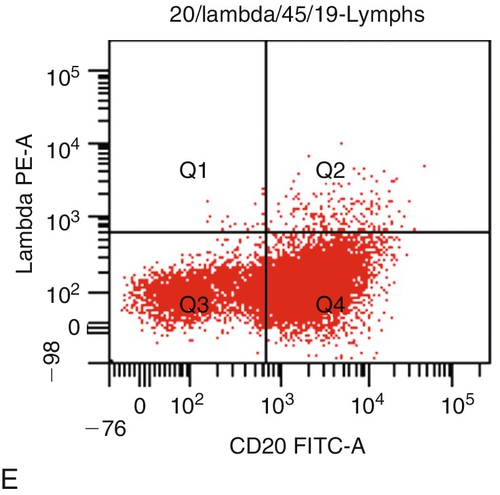
Figure 11-33 A, Lymph node morphology (× 4). B, Lymph node morphology (× 40). C, Flow cytometry scatterplot CD19 and CD10 staining. D, Flow cytometry scatterplot κ light-chain and CD20 staining. E, Flow cytometry scatterplot λ light-chain and CD20 staining, F, Flow cytometry scatterplot CD5 and λ light-chain staining. G, Flow cytometry scatterplot CD19 and surface immunoglobulin M (IgM) staining. H, Flow cytometry scatterplot CD19 and surface IgD staining. I, Diagnostic immunostain.
Figure 11-34 A, H&E stain, lymph node (× 4). B, H&E stain, lymph node (× 10). C, H&E stain, lymph node (× 40). D, Flow cytometry scatterplot κ light-chain and CD20 staining. E, Flow cytometry scatterplot λ light-chain and CD20 staining. F, Flow cytometry scatterplot CD19 and CD10 staining. G, Flow cytometry scatterplot CD5 and κ light-chain staining.
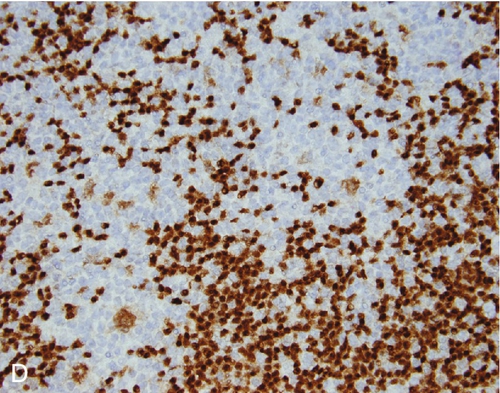
Figure 11-35 Stained sections of right inguinal lymph node. A, H&E stain (× 4). B, H&E stain (× 40). C, CD21 (× 10). D, PAX5 (× 40).
Figure 11-36 Sections of decalcified bone marrow. A, H&E stain × 10. B, H&E stain × 40.