Gynecomastia
Key Facts
Terminology
Nonneoplastic enlargement of male breast due to hyperplasia of epithelium and stroma
Etiology/Pathogenesis
Gynecomastia develops due to imbalance in ratio of free androgen to estrogen (variety of etiologies)
Clinical Issues
3 distinct peaks in occurrence of gynecomastia
Male infants (60-90%), transient
Males at puberty (48-64%, peak age: 13-14)
Highest prevalence in older males (50-80 years)
Gynecomastia is benign, usually self-limited
For persistent or symptomatic lesions, pharmacological and surgical options are available
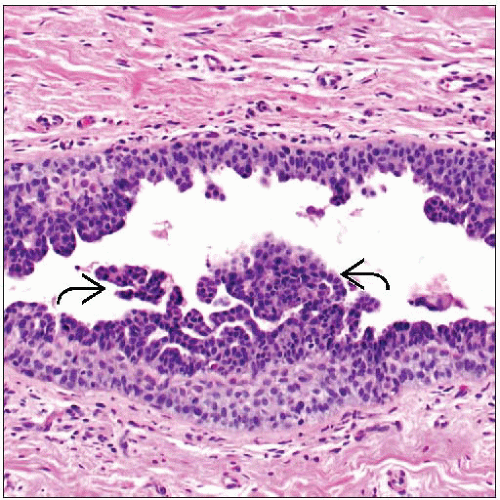
Microscopic Pathology
Hormonal imbalance stimulates stromal and glandular tissue in gynecomastia
Early changes (active florid phase)
Proliferation of periductal connective tissue, edema, inflammation
Mammary ductular epithelial hyperplasia
Later changes (inactive fibrous phase)
Flattening of ductal epithelium
Progressive fibrosis of adjacent stroma
Histological appearance of gynecomastia is same regardless of underlying cause
Top Differential Diagnoses
Male breast cancer
Myofibroblastoma
TERMINOLOGY
Definitions
Nonneoplastic enlargement of the male breast due to hyperplasia of both epithelium and stroma
ETIOLOGY/PATHOGENESIS
Endocrine Alterations and Pathogenesis
Gynecomastia develops because of alterations in ratio of free androgen to estrogen
Affected by serum levels of sex hormone-binding globulin
Many causes are recognized
Obesity resulting in enhanced peripheral aromatization of androgen to estrogen
Due to displacement of estrogen from sex hormone-binding globulin or decreased metabolism
Declining androgen synthesis with age
Medications
Digitalis, tricyclic antidepressants, amiodarone, simvastatin, atorvastatin, omeprazole, marijuana, topical agents, spironolactone, many anti-hypertensive medications
Anabolic steroid use in body builders
Nonsteroidal antiandrogen monotherapy treatment in patients with prostate cancer
Liver disease (cirrhosis, liver transplantation)
Renal disease (chronic renal failure, dialysis, kidney transplantation)
Hormone deficiency (hypogonadism, pituitary adenoma) and prostate cancer
Gonadal failure: Decreased testosterone
Primary gonadal failure includes Klinefelter syndrome (47,XXY; 50% of affected men develop gynecomastia), mumps orchitis, castration
Secondary gonadal failure includes hypothalamic and pituitary disease
Hormone-producing tumors
Leydig cell tumor
Sertoli cell tumor
Granulosa cell tumor
In at least 25% of cases, no cause is identified
CLINICAL ISSUES
Epidemiology
Incidence
Gynecomastia is common finding
Palpable breast tissue can be detected in 36% of healthy young adult males
57% of healthy older men and 70% of hospitalized elderly males show evidence of gynecomastia
3 distinct peaks of gynecomastia occur during male life span
Infancy: 60-90% of male infants show transient gynecomastia due to maternal estrogens; may produce milk (“witch’s milk”)
Puberty: 48-64% of males develop gynecomastia (peak incidence: 13-14 years); over 1/2 have family history of gynecomastia
Older age: Highest prevalence seen in males between 50-80 years of age
Incidence of symptomatic gynecomastia is markedly lower
Site
Subareolar and just superior to nipple
Presentation
Most often presents as a palpable, tender, firm, mobile, disc-shaped mound of tissue
May be painful; most common in 1st 6 months; possibly associated with stromal edema
May be unilateral or bilateral
Can be localized or diffuse