(1)
Department of Pathology, Rutgers-New Jersey Medical School, Newark, NJ, USA
Keywords
Pap smear slide preparationThe Bethesda systemNormal pap smearAtrophyPap smearMaturation indexCandida bacterial vaginosisTrichomonasHerpes simplexActinomycesAtypical squamous cells of uncertain significanceAsc-HAtypical glandular cellsLow-grade squamous intraepithelial lesionHigh-grade squamous intraepithelial lesionAdenocarcinoma-in-situSquamous cell carcinomaEndocervical adenocarcinomaPeritoneal washingsPapillary serous adenocarcinoma14.1 The Pap Smear
The pap smear is one of the best examples of the success of a screening test, with significant decreases in the incidence of cervical cancer since the availability of the test. It is not meant to be a diagnostic test, but a screening modality indicating that further evaluation may be warranted (Table 14.1).
Table 14.1
Key points about gynecologic cytology
The pap smear has markedly decreased the incidence of cervical cancer |
The pap smear is an excellent screening tool, but it is not a diagnostic tool. The purpose is to indicate that additional investigation is needed |
The pap smear may have false positives and false negatives |
Although an occasionally malignancy above the cervix (endometrium, ovary, fallopian tube) may shed and be detected on a pap smear, the pap smear is not a valid screening modality for these neoplasms |
14.2 The Bethesda System
Most laboratories utilize the Bethesda system for classification of pap smears (nih.techriver.net/). The report has several different components. Whether the slide is a conventional pap smear or liquid-based preparation is noted. Adequacy of the specimen is also noted. Interpretation includes negative for intraepithelial lesion or malignancy, epithelial cell abnormalities, and other malignancies. Also noted are any ancillary testing, automated review, and the option for educational notes or suggestions is included. Under negative for intraepithelial lesion/malignancy, organisms and other nonneoplastic findings can be reported.
14.3 Preparation of Cytology Slides
Most pap smears were previously prepared by obtaining the cells on the sampling device, smearing them directly onto the slide, and fixing the slide. This preparation can be difficult to interpret at times, due to thick areas and obscuring inflammation. Most laboratories now utilize liquid-based cytology, where the sampling device is placed in a preservative jar and the cells suspended in the liquid by swishing the sampling device around. The machines that prepare the slides filter out much of the inflammatory debris and prepare thinner cell layers, making the slides prepared in this manner easier to read. In addition, the residual cytology preservative can be utilized for ancillary testing such as HPV testing.
14.4 Normal Pap Smear Findings
14.4.1 Normal Squamous Epithelium
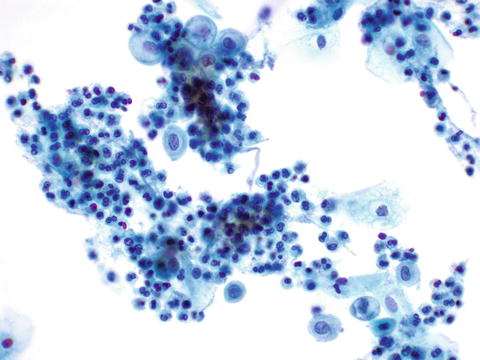
Normal squamous epithelial cells as seen on a cytology preparation may be seen at different stages of maturation. Superficial cells contain small nuclei in abundant cytoplasm. Intermediate cells have slightly larger nuclei (Fig. 14.1). Parabasal cells are usually not seen during reproductive life, but show up on menopausal pap smears. The hormonal status of a woman used to be evaluated by pap smears, with estrogenic effect shifting the cell ratio towards superficial cells with intermediate cells and atrophic estrogen-deficient smears showing prominent parabasal cells with intermediate cells. This used to be used in clinical practice, expressed as the maturation index, expressed as percentages of parabasal:intermediate:superficial cells; however, has fallen by the wayside for the most part.
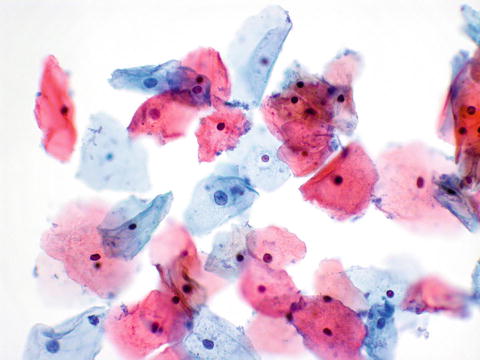
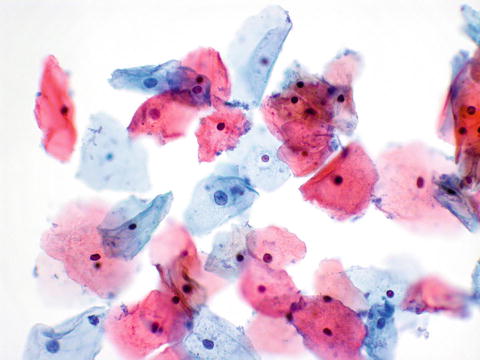
Fig. 14.1
Normal pap. Superficial cells with smaller nuclei, and intermediate cells (center) with larger nuclei are seen
14.4.2 Normal Endocervical Cells
The presence of endocervical cells or metaplastic squamous cells indicates that the transformation zone was sampled. Endocervical cells can either have a picket-fence arrangement in strips, or sheets of cells may show a honeycomb pattern (Fig. 14.2).
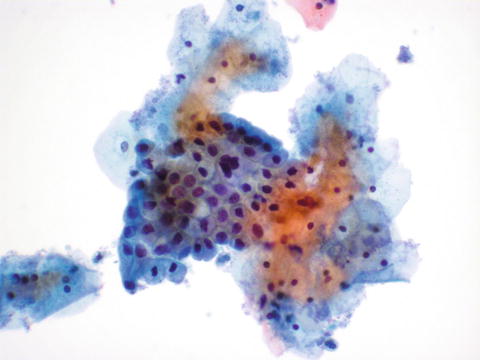
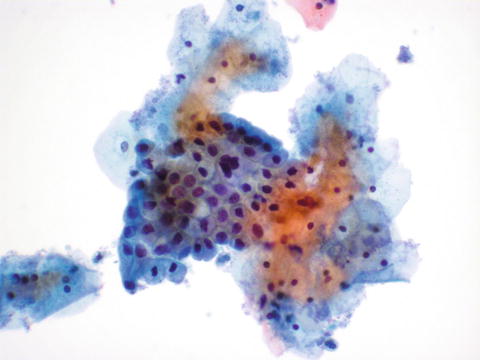
Fig. 14.2
Normal pap. Cluster of endocervical cells is seen showing a mix of the honeycomb configuration at the left, and the picket fence appearance at the upper right of the cell cluster
14.4.3 Endometrial Cells
Abnormal endometrial cells can indicate neoplasia; however, it is not rare to see normal-appearing endometrial cells (Fig. 14.3a, b), particularly during or shortly after menses. As pathologists don’t always have menstrual or menopausal status information, it is up to the clinician to determine if shedding endometrial cells are out of cycle or postmenopausal. The Bethesda system makes note of them in women over 40 to make sure to capture menopausal patients.
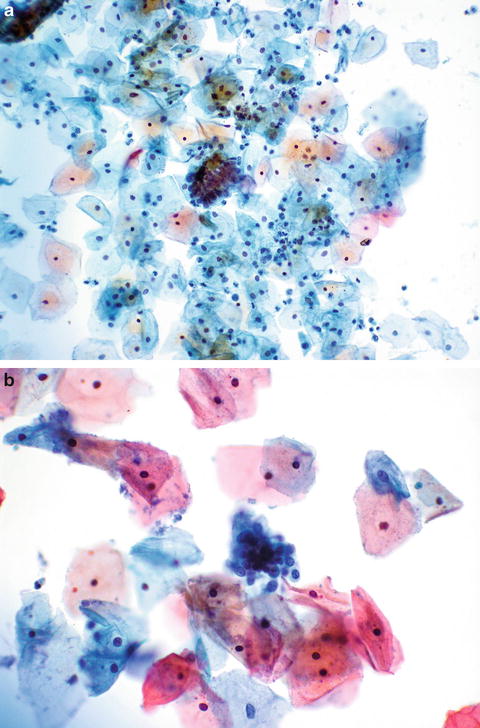
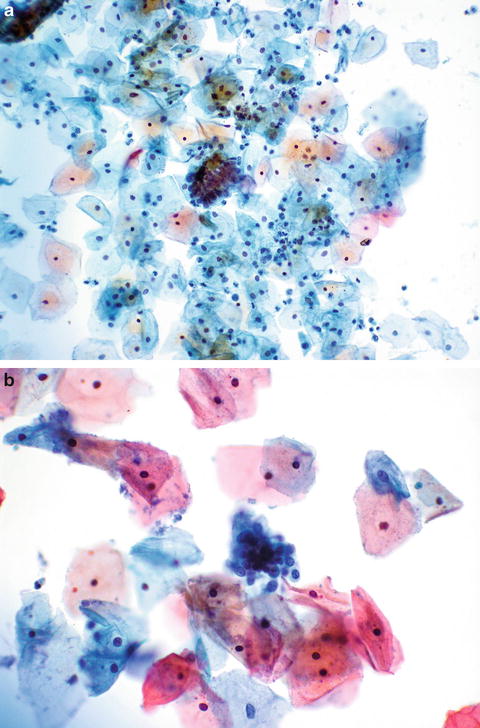
Fig. 14.3
Endometrial cells on pap. A cluster of endometrial cells is seen (a). The endometrial cells are much smaller than squamous and endocervical cells (b)
14.4.4 Atrophy
Atrophy associated with loss of estrogenic stimulus is a normal finding. It is characterized by a predominance of parabasal cells (Fig. 14.4). There may be abundant inflammatory cells; however, the histologic diagnosis of “atrophic vaginitis” as opposed to “atrophic pattern” does not correlate with clinical symptomatology [1].