16
Gram-Negative Cocci
CHAPTER CONTENTS
NEISSERIA
Diseases
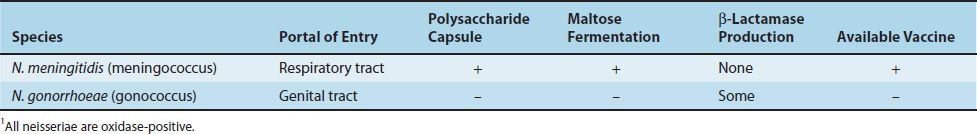
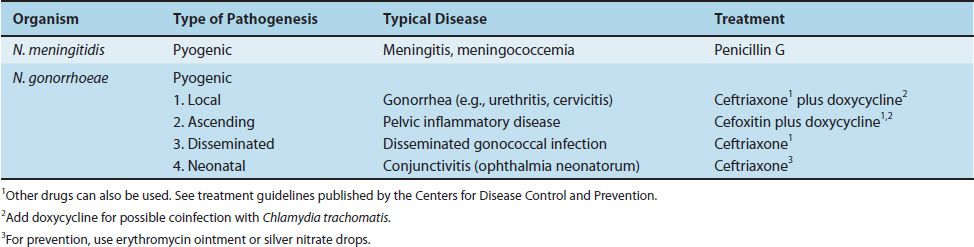
The genus Neisseria contains two important human pathogens: Neisseria meningitidis and Neisseria gonorrhoeae. N. meningitidis mainly causes meningitis and meningococcemia (Figure 16–1). In the United States, it is the leading cause of death from infection in children. N. gonorrhoeae causes gonorrhea (Figure 16–2), the second most common notifiable bacterial disease in the United States (Tables 16–1 and 16–2). It also causes neonatal conjunctivitis (ophthalmia neonatorum) (Figure 16–3) and pelvic inflammatory disease (PID). Note that Neisseria meningitidis is also known as the meningococcus (plural, meningococci), and Neisseria gonorrhoeae is also known as the gonococcus (plural, gonococci).
FIGURE 16–1 Meningococcemia. Note purpuric lesions on leg caused by endotoxin-mediated disseminated intravascular coagulation (DIC). (Reproduced with permission from Wolff K, Johnson R (eds): Fitzpatrick’s Color Atlas & Synopsis of Clinical Dermatology. 6th ed. New York: McGraw-Hill, 2009. Copyright © 2009 by The McGraw-Hill Companies, Inc.)
FIGURE 16–2 Gonorrhea. Note purulent urethral discharge caused by Neisseria gonorrhoeae. (Reproduced with permission from Wolff K, Johnson R (eds): Fitzpatrick’s Color Atlas & Synopsis of Clinical Dermatology. 6th ed. New York: McGraw-Hill, 2009. Copyright © 2009 by The McGraw-Hill Companies, Inc.)
FIGURE 16–3 Neonatal conjunctivitis (ophthalmia neonatorum) caused by Neisseria gonorrhoeae. Note purulent exudate, especially on lower right eyelid. The other common cause of neonatal conjunctivitis is Chlamydia trachomatis.
Important Properties
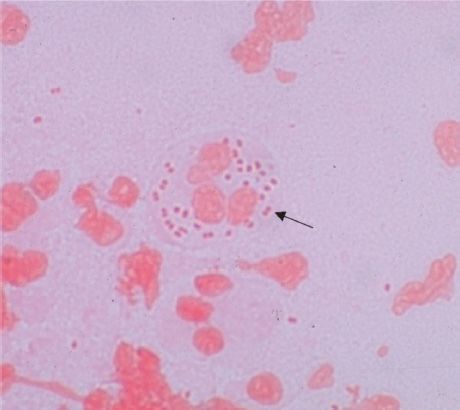
Neisseriae are gram-negative cocci that resemble paired kidney beans (Figure 16–4).
FIGURE 16–4 Neisseria gonorrhoeae—Gram stain. Arrow points to typical “kidney bean”–shaped gram-negative diplococci within a neutrophil. (Used with permission from Professor Shirley Lowe, University of California, San Francisco School of Medicine.)
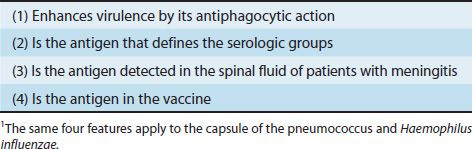
(1) N. meningitidis (meningococcus) has a prominent polysaccharide capsule that enhances virulence by its antiphagocytic action and induces protective antibodies (Table 16–3). Meningococci are divided into at least 13 serologic groups on the basis of the antigenicity of their capsular polysaccharides. Five serotypes cause most cases of meningitis and meningococcemia: A, B, C, Y, and W-135. Serotype A is the leading cause of epidemic meningitis worldwide. Serotype B accounts for most disease in the United States.
(2) N. gonorrhoeae (gonococcus) has no polysaccharide capsule but has multiple serotypes based on the antigenicity of its pilus protein. There is marked antigenic variation in the gonococcal pili as a result of chromosomal rearrangement; more than 100 serotypes are known. Gonococci have three outer membrane proteins (proteins I, II, and III). Protein II plays a role in attachment of the organism to cells and varies antigenically as well.
Neisseriae are gram-negative bacteria and contain endotoxin in their outer membrane. Note that the endotoxin of Neisseriae consist of lipooligosaccharide (LOS), in contrast to the lipopolysaccharide (LPS) found in enteric gram-negative rods. Both LPS and LOS contain lipid A, but the oligosaccharide part of LOS contains few sugars, whereas the polysaccharide part of LPS contains a long repeating sugar side chain.
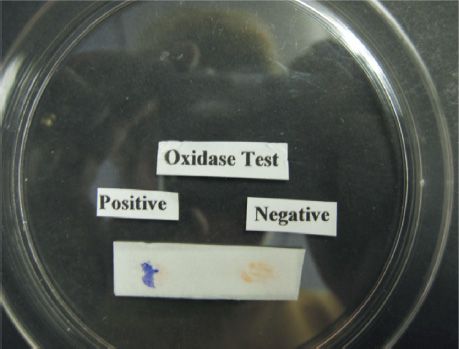
The growth of both organisms is inhibited by toxic trace metals and fatty acids found in certain culture media (e.g., blood agar plates). They are therefore cultured on “chocolate” agar containing blood heated to 80°C, which inactivates the inhibitors. Neisseriae are oxidase-positive (Figure 16–5) (i.e., they possess the enzyme cytochrome c). This is an important laboratory diagnostic test in which colonies exposed to phenylenediamine turn purple or black as a result of oxidation of the reagent by the enzyme (Figure 16–2).
FIGURE 16–5 Oxidase test—A drop of the oxidase reagent was placed on the left and right side of the filter paper. Bacteria from a colony of Neisseria gonorrhoeae were rubbed on the drop on the left, and the purple color indicates a positive test (i.e., the organism is oxidase-positive). Bacteria from a colony of Escherichia coli were rubbed on the drop on the right, and the absence of a purple color indicates a negative test (i.e., the organism is oxidase-negative). (Used with permission from Professor Shirley Lowe, University of California, San Francisco School of Medicine.)
The genus Neisseria is one of several in the family Neisseriaceae. A separate genus contains the organism Moraxella catarrhalis, which is part of the normal throat flora but can cause such respiratory tract infections as sinusitis, otitis media, bronchitis, and pneumonia. M. catarrhalis and members of other genera, such as Branhamella, Kingella, and Acinetobacter, are described in Chapter 27. (M. catarrhalis is the new name for Branhamella catarrhalis.)
1. Neisseria meningitidis
Pathogenesis & Epidemiology
Humans are the only natural hosts for meningococci. The organisms are transmitted by airborne droplets; they colonize the membranes of the nasopharynx and become part of the transient flora of the upper respiratory tract. Carriers are usually asymptomatic. From the nasopharynx, the organism can enter the bloodstream and spread to specific sites, such as the meninges or joints, or be disseminated throughout the body (meningococcemia). About 5% of people become chronic carriers and serve as a source of infection for others. The carriage rate can be as high as 35% in people who live in close quarters (e.g., military recruits); this explains the high frequency of outbreaks of meningitis in the armed forces prior to the use of the vaccine. The carriage rate is also high in close (family) contacts of patients. Outbreaks of meningococcal disease also have occurred in college students living in dormitories.
Two organisms cause more than 80% of cases of bacterial meningitis in infants older than 2 months of age: Streptococcus pneumoniae and N. meningitidis. Of these organisms, meningococci, especially those in group A, are most likely to cause epidemics of meningitis. Group B meningococci cause many cases of meningitis in developed countries because it is not present in the vaccine (see “Prevention”, later). Overall, N. meningitidis ranks second to S. pneumoniae as a cause of meningitis but is the most common cause in persons between the ages of 2 and 18 years.
Meningococci have three important virulence factors:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree