General Considerations
COMMUNICATION BETWEEN SURGEONS AND PATHOLOGISTS
Requisition Forms
Should include information important for optimal processing and interpretation of specimen
Specimen Labeling
Type of specimen must be clearly indicated
Orientation
Specimens must have adequate orientation in order to identify sites of possible margin involvement
Specimen Radiography
Excisions of radiographic lesions must be imaged before transfer to pathology department
INTRAOPERATIVE CONSULTATIONS
Primary Diagnosis
Frozen sections are > 95% accurate for diagnosis of invasive carcinoma
There is a small possibility of error, particularly for small carcinomas and carcinoma in situ
Frozen sections should not be performed for primary diagnosis except in rare circumstances
Technique is limited: Able to freeze only small amount of tissue, ice crystal artifact, loss of nuclear detail, uneven sectioning, and possible tissue loss
Should never be performed if entire lesion is frozen; risk to patient of not having an accurate diagnosis outweighs any value of intraoperative diagnosis
Should not be performed unless patient has consented to additional surgery based on findings
Margins
Radiologic margins
If patient has prior history of cancer associated with a radiologic finding, specimen radiograph can be used as guide to margin or margins closest to cancer
However, DCIS at margins is rarely visualized by radiography
Gross evaluation
Gross distance of palpable cancers to margins can be determined
DCIS is rarely grossly apparent and may be present at margins in grossly normal-appearing tissue
Microscopic evaluation by frozen section
Very difficult to evaluate breast specimen margins by frozen section
Negative results do not preclude positive margins found by additional sampling for permanent sections
Microscopic evaluation by touch preparations
Margins can be evaluated by scraping specimen surfaces
Only evaluate surface for positive margins; close margins are not identified
May be of value at centers where only positive margins undergo reexcision
Lymph Node Evaluation: Frozen Section
Sentinel nodes may undergo intraoperative evaluation if surgeon will complete an axillary dissection if results are positive
Nodes are carefully dissected away from each other and counted
Number of nodes is very important for prognosis and for determining likelihood of additional nodal involvement
Each node is thinly sliced and completely frozen
Most common source of false-negative results is failure to freeze all slices
All macrometastases can be identified by this method
Additional micrometastases and isolated tumor cells may be seen in additional levels evaluated by permanent section
Lymph Node Evaluation: Touch Preparations
Nodes are identified as described above and thinly sectioned
Cut surfaces of each node are scraped and used for touch preparations
Size of metastasis cannot be determined with certainty
SPECIMEN RADIOGRAPHY
Core Needle Biopsies
Cores should be radiographed to document that representative calcifications have been removed
Cores with calcifications are generally identified separately from cores without calcifications
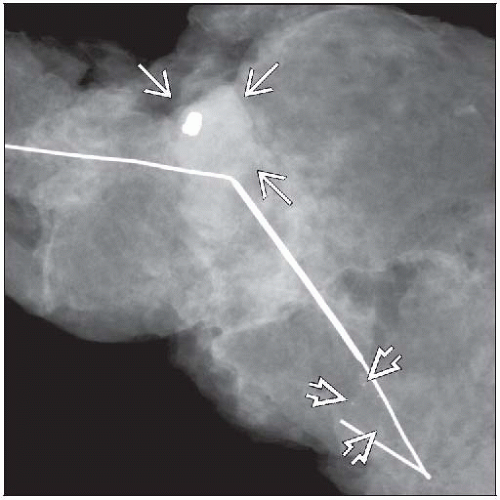
Wire Localized Excisions
Specimen must be radiographed to ensure that targeted lesion has been removed
Radiologist should issue a report stating whether targeted lesion has been removed
Copy of radiograph and radiologist’s report should be available to pathologist
Mammographically guided excisions
Lesions are associated with specific types of pathologic diagnoses
Irregular mass
97% invasive carcinoma
2% surgical or trauma-related scarring
1% rare lesions, such as radial sclerosing lesion, fibromatosis, granular cell tumor
Circumscribed or lobulated mass
65% fibroadenoma
20% cysts or clusters of cysts
9% other benign lesions, such as nodular sclerosing adenosis, myofibroblastoma, hamartoma, angiolipoma
3% DCIS (intracystic DCIS, DCIS involving a fibroadenoma, DCIS with surrounding stromal fibrosis)
3% invasive carcinoma (especially medullary, mucinous, solid lobular, and triple negative types)
Ill-defined mass: May have actual ill-defined margins or may have margins obscured by adjacent fibrous tissue
20% fibroadenoma
15% invasive carcinoma
2% DCIS
63% other benign lesions
Calcifications
Radiologically suspicious calcifications are clustered, linear, or segmental with amorphous or pleomorphic morphology
Many additional nonsuspicious calcifications can be seen radiographically
Thus it is essential to be certain that the suspicious radiologic calcifications are sampled for microscopic examination
75% benign due to apocrine cysts, sclerosing adenosis, hyalinized fibroadenomas
20% DCIS
5% invasive carcinoma; generally small (< 1 cm)
Architectural distortion
Change in texture of breast as compared to other areas, contralateral breast, or over time
33% diffusely invasive carcinoma, especially lobular carcinoma
33% DCIS
33% benign changes
Ultrasound-guided excisions
Performed for mass-forming lesions
Lesion is usually evident on gross examination
Often used to evaluate lesions initially detected by clinical palpation, mammography, or MR
25-50% are carcinoma with majority invasive carcinomas
Presence of lesion may be confirmed by radiologist using US
An image is generally not provided to pathologist
MR-guided excisions
Difficult to perform due to need for open coil and special equipment
Lesions are visualized due to vascular uptake of a contrast agent
Excised specimens cannot be imaged using same method
Lesions are typically small and not grossly evident
Correlation of appearance with pathologic findings is generally low
Irregular mass: 18% invasive carcinoma, 10% DCIS, 16% fibroadenoma, 56% other benign lesions
Circumscribed mass: 11% invasive carcinoma, 3% DCIS, 43% fibroadenoma, 43% other benign lesions
Linear/clumped enhancement: 5% invasive carcinoma, 19% DCIS, 12% fibroadenoma, 64% other benign lesions
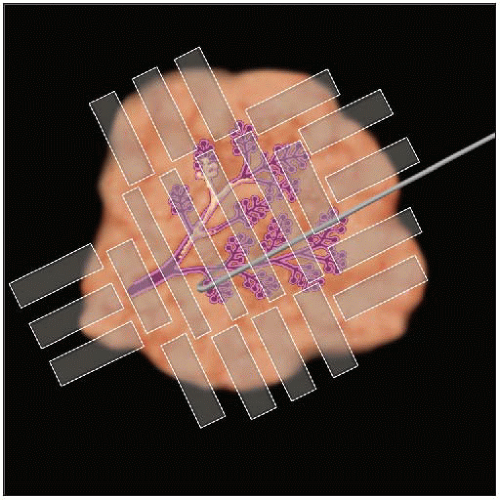
Excisions with > 1 wire
Multiple wires may be used to mark multiple lesions or single lesion that extends over large area
Extensive calcifications
Large area of architectural distortion
If multiple separate lesions are present, distance between lesions should be recorded and tissue between lesion sampled
If lesion extends over large area, all tissue should be sampled when practical
Mastectomies
Generally not sent for radiologic examination by surgeon
Radiologic examination prior to processing can be very helpful in the following circumstances
Suspicious radiologic lesions that have not been previously biopsied
Prior core needle biopsy or biopsies for nonpalpable cancers now marked by clip(s)
Post neoadjuvant cancers with marked or complete imaging response, now marked by clip(s)
FIXATION
Transport to Pathology Department
Should occur as rapidly as possible
Tissue can be transported without fixation if within 1-2 hours
Preferred if frozen sections, flow cytometry, some types of molecular studies, bacterial culture, or tissue banking are planned
Intact specimens can be placed into formalin if longer time to specimen processing is anticipated
Formalin penetrates tissues slowly
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree