Chapter 6 Gastrointestinal disease
Introduction
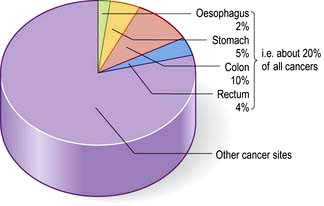
In developed countries gastrointestinal symptoms are a common reason for attendance to primary care clinics and to hospital outpatients. Approximately 75% of these consultations are for non-organic symptoms. The clinician’s main task is therefore to recognize when organic disease must be sought or excluded, remembering that 20% of all cancers occur in the gastrointestinal tract (Fig. 6.1). In developing countries, malnutrition and poor hygiene make infection a more probable diagnosis. The clinician needs to recognize and treat these infections promptly and also help with prevention by encouraging good hygiene.
Gastrointestinal symptoms and signs
Dyspepsia and indigestion
Features of dyspepsia suggestive of serious diseases such as cancer are known as ‘Alarm’ symptoms.
Vomiting
Many gastrointestinal (and non-gastrointestinal) conditions are associated with vomiting (Table 6.1). This is controlled by a complex reflex involving central neural control centres located in the lateral reticular formation of the medulla which are stimulated by the chemoreceptor trigger zones (CTZs) in the floor of the fourth ventricle, and also by vagal afferents from the gut. The central zones are directly stimulated by toxins, drugs, motion sickness and metabolic disturbances. Raised intracranial pressure has a direct effect on the vomiting centre leading to vomiting. Luminal toxins, inflammation and mechanical obstruction are local GI causes of vomiting.
Table 6.1 Causes of vomiting: some examples
Faeculent vomit suggests low intestinal obstruction or the presence of a gastrocolic fistula.
Haematemesis is vomiting fresh or altered blood (‘coffee-grounds’) (see p. 254).
Persistent nausea alone is often stress-related and is not due to gastrointestinal disease.
Flatulence
This term describes excessive wind. It is used to indicate belching, abdominal distension, gurgling and the passage of flatus per rectum. Swallowing air (aerophagia) is described on page 296. Some of the swallowed air passes into the intestine where most of it is absorbed, but some remains to be passed rectally. Colonic bacterial breakdown of non-absorbed carbohydrate also produces gas. Rectal flatus thus consists of nitrogen, carbon dioxide, hydrogen and methane. It is normal to pass rectal flatus up to 20 times/day. Causes of increased gas production and intake include high-fibre diet and carbonated drinks.
Diarrhoea and constipation
These are common complaints and in the community are not usually due to serious disease. They are described in detail on pages 291 and 282, respectively. Some general rules concerning the aetiology and investigation of diarrhoea are shown in Box 6.1.
![]() Box 6.1
Box 6.1
Simple rules in diarrhoea
Abdominal pain
Pain is stimulated mainly by the stretching of smooth muscle or organ capsules. Severe acute abdominal pain can be due to a large number of gastrointestinal conditions, and normally presents as an emergency (see p. 298). An apparent ‘acute abdomen’ can occasionally be due to referred pain from the chest, as in pneumonia or to metabolic causes, such as diabetic ketoacidosis or porphyria.
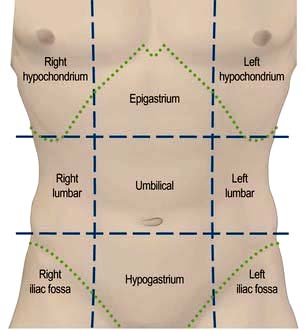
 Site (Fig. 6.2), intensity, character, duration and frequency of the pain
Site (Fig. 6.2), intensity, character, duration and frequency of the pain
 Aggravating and relieving factors
Aggravating and relieving factors
 Associated symptoms, including non-gastrointestinal symptoms.
Associated symptoms, including non-gastrointestinal symptoms.
Upper abdominal pain
Right hypochondrial pain may originate from the gall bladder or biliary tract. Biliary pain can also be epigastric. Biliary pain is typically intermittent and severe, lasts a few hours and remits spontaneously to recur weeks or months later. Hepatic congestion (e.g. in hepatitis or cardiac failure) and sometimes peptic ulcer disease can present with pain in the right hypochondrium. Chronic, persistent or constant pain in the right (or left) hypochondrium in a well-looking patient is a frequent functional symptom; this chronic pain is not due to gall bladder disease (see p. 353).
Examination of the abdomen
Palpation
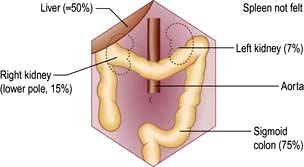
Look for palpable masses or abdominal tenderness. All abdominal quadrants should be palpated in turn followed by deeper palpations; remember to watch the patient’s face for signs of pain or discomfort. Evaluate any palpable mass and note its size, shape and consistency and whether it moves with respiration, to decide which organ is involved. Some abdominal organs may be just palpable normally, usually in thin people (Fig. 6.3). Reidel’s lobe is an anatomical variant consisting of a palpable enlargement of the lateral portion of the right lobe of the liver. The hernial orifices should be examined if intestinal obstruction is suspected.
Examination of the rectum and sigmoid colon
 Proctoscopy (see Practical Box 6.1) is performed in all patients with a history of bright red rectal bleeding to look for anorectal pathology such as haemorrhoids; a rigid sigmoidoscope is too narrow and long to enable adequate examination of the anal canal.
Proctoscopy (see Practical Box 6.1) is performed in all patients with a history of bright red rectal bleeding to look for anorectal pathology such as haemorrhoids; a rigid sigmoidoscope is too narrow and long to enable adequate examination of the anal canal.
 Sigmoidoscopy is part of the routine hospital examination in cases of diarrhoea and in patients with lower abdominal symptoms such as a change in bowel habit or rectal bleeding. The rigid sigmoidoscope allows inspection of a maximum of 20–25 cm of distal colon.
Sigmoidoscopy is part of the routine hospital examination in cases of diarrhoea and in patients with lower abdominal symptoms such as a change in bowel habit or rectal bleeding. The rigid sigmoidoscope allows inspection of a maximum of 20–25 cm of distal colon.
 Flexible sigmoidoscopy (FS) (60 cm) can reach up to the splenic flexure, and can be performed in the outpatient department or endoscopy unit after evacuation of the distal colon using an enema or suppository. FS can be used in patients with increased stool frequency or looseness or rectal bleeding to diagnose colitis or polyps. Most rectal bleeding is due to benign anorectal disease (haemorrhoids or fissure-in-ano) and an otherwise normal FS can be reassuring to avoid over-investigation. Up to 60% of colonic neoplasms occur within the range of FS (see Fig. 6.45) and it has therefore been proposed as screening test for colorectal cancer in asymptomatic individuals.
Flexible sigmoidoscopy (FS) (60 cm) can reach up to the splenic flexure, and can be performed in the outpatient department or endoscopy unit after evacuation of the distal colon using an enema or suppository. FS can be used in patients with increased stool frequency or looseness or rectal bleeding to diagnose colitis or polyps. Most rectal bleeding is due to benign anorectal disease (haemorrhoids or fissure-in-ano) and an otherwise normal FS can be reassuring to avoid over-investigation. Up to 60% of colonic neoplasms occur within the range of FS (see Fig. 6.45) and it has therefore been proposed as screening test for colorectal cancer in asymptomatic individuals.
![]() Practical Box 6.1
Practical Box 6.1
Sigmoidoscopy and proctoscopy
Sigmoidoscopy
 The technique using a 25 cm rigid sigmoidoscope is easy to learn, provides valuable information and is safe in competent hands.
The technique using a 25 cm rigid sigmoidoscope is easy to learn, provides valuable information and is safe in competent hands.
 No bowel preparation is required.
No bowel preparation is required.
 Explain to the patient the nature of the procedure and obtain consent.
Explain to the patient the nature of the procedure and obtain consent.
 The technique is relatively painless. In the irritable bowel syndrome, the patient’s pain is often reproduced by air insufflation:
The technique is relatively painless. In the irritable bowel syndrome, the patient’s pain is often reproduced by air insufflation:
Proctoscopy
1. The proctoscope is passed into the anus and the obturator is removed.
2. The patient strains down as the proctoscope is removed.
3. Haemorrhoids are seen as purplish veins in the left lateral, right posterior or right anterior positions.
4. Fissures may also be seen, but pain often prevents the procedure from being performed.
Stool examination
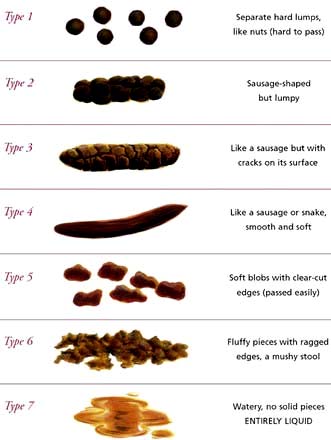
It is useful to confirm a patient’s account (e.g. passing of blood or steatorrhoea). The shape and size may be helpful (e.g. ‘rabbit dropping’ or ribbon-like stools in the irritable bowel syndrome). Stool charts for recording consistency and frequency of defecation are useful in inpatients to follow the progress of diarrhoea, particularly in the management of severe colitis. The Bristol Stool Chart is commonly used in the UK (Fig. 6.4).
Investigations
Routine haematology and biochemistry, followed by endoscopy and radiology, are the principal investigations. The investigation of small bowel disease is discussed in more detail on page 267. Manometry is mainly used in oesophageal disease (see p. 237) and anorectal disorders (see p. 286).
Endoscopy
 Oesophagogastroduodenoscopy (OGD, ‘gastroscopy’) is the investigation of choice for upper GI disorders with the possibility of therapy and mucosal biopsy. Findings include reflux oesophagitis, gastritis, ulcers and cancer. Therapeutic OGD is used to treat upper GI haemorrhage and both benign and malignant obstruction. Relative contraindications include severe chronic obstructive pulmonary disease, a recent myocardial infarction, or severe instability of the atlantoaxial joints. The mortality for diagnostic endoscopy is 0.001% with significant complications in 1 : 10 000, usually when performed as an emergency (e.g. GI haemorrhage).
Oesophagogastroduodenoscopy (OGD, ‘gastroscopy’) is the investigation of choice for upper GI disorders with the possibility of therapy and mucosal biopsy. Findings include reflux oesophagitis, gastritis, ulcers and cancer. Therapeutic OGD is used to treat upper GI haemorrhage and both benign and malignant obstruction. Relative contraindications include severe chronic obstructive pulmonary disease, a recent myocardial infarction, or severe instability of the atlantoaxial joints. The mortality for diagnostic endoscopy is 0.001% with significant complications in 1 : 10 000, usually when performed as an emergency (e.g. GI haemorrhage).
 Colonoscopy allows good visualization of the whole colon and terminal ileum. Biopsies can be obtained and polyps removed. Benign strictures can be dilated and malignant strictures stented. The success rate for reaching the caecum should be at least 90% after training. Cancer, polyps and diverticular disease are the commonest significant findings. Perforation occurs in 1 : 1000 examinations but this is higher (up to 2%) after polypectomy (see Practical Box 6.2).
Colonoscopy allows good visualization of the whole colon and terminal ileum. Biopsies can be obtained and polyps removed. Benign strictures can be dilated and malignant strictures stented. The success rate for reaching the caecum should be at least 90% after training. Cancer, polyps and diverticular disease are the commonest significant findings. Perforation occurs in 1 : 1000 examinations but this is higher (up to 2%) after polypectomy (see Practical Box 6.2).
 Balloon enteroscopy, either double or single balloon, can examine the small bowel from the duodenum to the ileum using specialized enteroscopes in expert centres.
Balloon enteroscopy, either double or single balloon, can examine the small bowel from the duodenum to the ileum using specialized enteroscopes in expert centres.
 Capsule endoscopy is used for the evaluation of obscure GI bleeding (after negative gastroscopy and colonoscopy) and for the detection of small bowel tumours and occult inflammatory bowel disease. It should be avoided if strictures are suspected.
Capsule endoscopy is used for the evaluation of obscure GI bleeding (after negative gastroscopy and colonoscopy) and for the detection of small bowel tumours and occult inflammatory bowel disease. It should be avoided if strictures are suspected.
![]() Practical Box 6.2
Practical Box 6.2
Gastroscopy and colonoscopy
Gastroscopy
1. Patient should be fasted for at least 4 hours.
2. Give oxygen and monitor oxygen saturation with an oximeter.
3. Give lidocaine throat spray or sedation (midazolam ± opiate if required).
4. Pass the gastroscope to the duodenum under direct vision.
5. Examine during insertion and withdrawal.
6. Gastroscopy takes 5–15 min, depending on the indication and findings.
7. Withhold fluid and food until LA/sedation wears off.
8. Complications are rare: beware of over-sedation, perforation and aspiration.
Colonoscopy
1. Stop oral iron a week before the procedure.
2. Restrict diet to low residue foods for 48 hours; clear fluids only for 24 hours.
3. Use local bowel cleansing regime, usually starting 24 hours beforehand (e.g. two sachets of sodium picosulfate with magnesium citrate and 2–4 bisacodyl tablets, or macrogols 2–4 L, or local alternative; more if constipated).
4. Give oxygen and monitor O2 levels.
5. Give sedation (midazolam ± opiate) if required by patient.
6. Pass the colonoscope to the caecum or ileum under direct vision.
7. Examine in detail during withdrawal.
8. Colonoscopy takes 15–30 min, depending on the colon anatomy, indication and findings.
9. Withhold fluid and food until sedation wears off.
10. Observe patient for at least an hour after sedation given.
11. Complications are rare: beware of over-sedation, perforation and aspiration.
Imaging
 Endoscopic ultrasound (EUS) is performed with a gastroscope incorporating an ultrasound probe at the tip. It is used diagnostically for lesions in the oesophageal or gastric wall, including the detailed TNM staging (see p. 245) of oesophageal/gastric cancer and for the detection and biopsy of pancreatic tumours and cysts.
Endoscopic ultrasound (EUS) is performed with a gastroscope incorporating an ultrasound probe at the tip. It is used diagnostically for lesions in the oesophageal or gastric wall, including the detailed TNM staging (see p. 245) of oesophageal/gastric cancer and for the detection and biopsy of pancreatic tumours and cysts.
 Endoanal and endorectal ultrasonography are performed to define the anatomy of the anal sphincters (see p. 285), to detect perianal disease and to stage superficial rectal tumours.
Endoanal and endorectal ultrasonography are performed to define the anatomy of the anal sphincters (see p. 285), to detect perianal disease and to stage superficial rectal tumours.
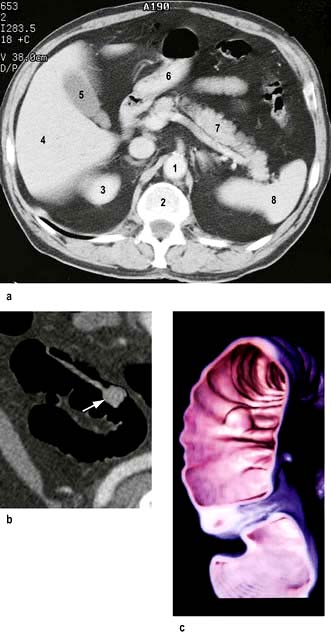
Computed tomography involves a significant dose of radiation (approximately 10 millisieverts). Modern multislice fast scanners and techniques involving intraluminal and intravenous contrast enhance diagnostic capability. Intraluminal contrast may be positive (Gastrografin or Omnipaque) or negative (usually water). The bowel wall and mesentery are well seen after intravenous contrast especially with negative intraluminal contrast. Clinically unsuspected diseases of other abdominal organs are quite often also revealed (Fig. 6.5a).
 CT is widely used as a first-line investigation for the acute abdomen. CT is sensitive for small volumes of gas from a perforated viscus as well as leakage of contrast from the gut lumen.
CT is widely used as a first-line investigation for the acute abdomen. CT is sensitive for small volumes of gas from a perforated viscus as well as leakage of contrast from the gut lumen.
 Inflammatory conditions such as abscesses, appendicitis, diverticulitis, Crohn’s disease and its complications are well demonstrated. In high-grade bowel obstruction, CT is usually diagnostic of both the presence and the cause of the obstruction.
Inflammatory conditions such as abscesses, appendicitis, diverticulitis, Crohn’s disease and its complications are well demonstrated. In high-grade bowel obstruction, CT is usually diagnostic of both the presence and the cause of the obstruction.
 CT is widely used in cancer staging and as guidance for biopsy of tumour or lymph nodes.
CT is widely used in cancer staging and as guidance for biopsy of tumour or lymph nodes.
 CT pneumocolon/CT colonography (virtual colonoscopy) after CO2 insufflation into a previously cleansed colon provides an alternative to colonoscopy for diagnosis of colon mass lesions (Fig. 6.5b). It is being evaluated as a screening test for colon pathology with sensitivities of over 90% for >10 mm polyps.
CT pneumocolon/CT colonography (virtual colonoscopy) after CO2 insufflation into a previously cleansed colon provides an alternative to colonoscopy for diagnosis of colon mass lesions (Fig. 6.5b). It is being evaluated as a screening test for colon pathology with sensitivities of over 90% for >10 mm polyps.
 Unprepared CT is a good test for colon cancer in the frail (often elderly) patient who would have problems with bowel preparation.
Unprepared CT is a good test for colon cancer in the frail (often elderly) patient who would have problems with bowel preparation.
Contrast studies
 Barium swallow examines the oesophagus and proximal stomach. Its main use is for investigating dysphagia.
Barium swallow examines the oesophagus and proximal stomach. Its main use is for investigating dysphagia.
 Double-contrast barium meal examines the oesophagus, stomach and duodenum. Barium is given to produce mucosal coating and effervescent granules producing carbon dioxide in the stomach create a double contrast between gas and barium. This test has a high accuracy for the detection of significant pathology – ulcers and cancer – but requires good technique. Gastroscopy is a more sensitive test and enables biopsy of suspicious areas.
Double-contrast barium meal examines the oesophagus, stomach and duodenum. Barium is given to produce mucosal coating and effervescent granules producing carbon dioxide in the stomach create a double contrast between gas and barium. This test has a high accuracy for the detection of significant pathology – ulcers and cancer – but requires good technique. Gastroscopy is a more sensitive test and enables biopsy of suspicious areas.
 Small bowel meal or follow-through specifically examines the small bowel. Ingested barium passes through the small bowel into the right colon. The fold pattern and calibre of the small bowel are assessed. Specific views of the terminal ileum can be obtained and are used to identify early changes in patients with suspected Crohn’s disease.
Small bowel meal or follow-through specifically examines the small bowel. Ingested barium passes through the small bowel into the right colon. The fold pattern and calibre of the small bowel are assessed. Specific views of the terminal ileum can be obtained and are used to identify early changes in patients with suspected Crohn’s disease.
 Small bowel enema (enteroclysis) is an alternative specific technique for small bowel examination. A tube is passed into the duodenum and a large volume of dilute barium is introduced. It is particularly used to demonstrate strictures or adhesions when there is suspicion of intermittent obstruction. Generally, this has been replaced by MR enteroclysis.
Small bowel enema (enteroclysis) is an alternative specific technique for small bowel examination. A tube is passed into the duodenum and a large volume of dilute barium is introduced. It is particularly used to demonstrate strictures or adhesions when there is suspicion of intermittent obstruction. Generally, this has been replaced by MR enteroclysis.
 Barium enema examines the colon and is used for altered bowel habit. Colonoscopy and CT colonography have largely replaced this examination for rectal bleeding, polyps and inflammatory bowel disease.
Barium enema examines the colon and is used for altered bowel habit. Colonoscopy and CT colonography have largely replaced this examination for rectal bleeding, polyps and inflammatory bowel disease.
 Absorbable water-soluble (Gastrografin or Omnipaque) contrast agents should be used in preference to barium when perforation is suspected anywhere in the gut.
Absorbable water-soluble (Gastrografin or Omnipaque) contrast agents should be used in preference to barium when perforation is suspected anywhere in the gut.
Radioisotopes
 Detect urease activity of Helicobacter pylori – 13C urea breath test (see p. 249)
Detect urease activity of Helicobacter pylori – 13C urea breath test (see p. 249)
 Assess oesophageal reflux – gamma camera scan after oral [99mTc]technetium-sulphur colloid
Assess oesophageal reflux – gamma camera scan after oral [99mTc]technetium-sulphur colloid
 Measure rate of gastric emptying – sequential gamma camera scans after oral [99mTc]technetium-sulphur colloid or 111In-DTPA (indium-labelled diethylene triamine penta-acetic acid)
Measure rate of gastric emptying – sequential gamma camera scans after oral [99mTc]technetium-sulphur colloid or 111In-DTPA (indium-labelled diethylene triamine penta-acetic acid)
 Demonstrate a Meckel’s diverticulum – gamma camera scan after i.v. [99mTc]pertechnetate, which has affinity for gastric mucosa
Demonstrate a Meckel’s diverticulum – gamma camera scan after i.v. [99mTc]pertechnetate, which has affinity for gastric mucosa
 Assess extent of inflammation and presence of inflammatory collections in inflammatory bowel disease – gamma camera scan after i.v. 99mTc-HMPAO (hexamethylpropylene amine oxime) labelled white cells
Assess extent of inflammation and presence of inflammatory collections in inflammatory bowel disease – gamma camera scan after i.v. 99mTc-HMPAO (hexamethylpropylene amine oxime) labelled white cells
 Evaluate neuroendocrine tumours and their metastases – gamma camera scan after i.v. radiolabelled octreotide or MIBG (meta-iodobenzylguanidine)
Evaluate neuroendocrine tumours and their metastases – gamma camera scan after i.v. radiolabelled octreotide or MIBG (meta-iodobenzylguanidine)
 Assess obscure gastrointestinal bleeding – gamma camera abdominal scan after i.v. injection of red cells labelled with 99mTc (only useful if the bleeding is >2 mL/min)
Assess obscure gastrointestinal bleeding – gamma camera abdominal scan after i.v. injection of red cells labelled with 99mTc (only useful if the bleeding is >2 mL/min)
 Measure albumin loss in the stools (in protein-losing enteropathy) – following albumin labelled in vivo with i.v. 51CrCl3. This test has been replaced by the measurement of the intestinal clearance of α1 antitrypsin
Measure albumin loss in the stools (in protein-losing enteropathy) – following albumin labelled in vivo with i.v. 51CrCl3. This test has been replaced by the measurement of the intestinal clearance of α1 antitrypsin
 Assess bile salt malabsorption (in patients with unexplained diarrhoea) – gamma camera scan to measure both isotope retention and faecal loss of orally administered 75selenium-homocholic acid taurine (SeHCAT) (see p. 293)
Assess bile salt malabsorption (in patients with unexplained diarrhoea) – gamma camera scan to measure both isotope retention and faecal loss of orally administered 75selenium-homocholic acid taurine (SeHCAT) (see p. 293)
 Detect bacterial overgrowth in the small bowel – measure 14CO2 in breath following oral 14C glycocholic acid.
Detect bacterial overgrowth in the small bowel – measure 14CO2 in breath following oral 14C glycocholic acid.
The mouth
Recurrent aphthous ulceration
 Minor aphthous ulcers are the most common, are <10 mm diameter, have a grey/white centre with a thin erythematous halo and heal within 14 days without scarring. They rarely affect the dorsum of the tongue or hard palate.
Minor aphthous ulcers are the most common, are <10 mm diameter, have a grey/white centre with a thin erythematous halo and heal within 14 days without scarring. They rarely affect the dorsum of the tongue or hard palate.
 Major aphthous ulcers (>10 mm diameter) often persist for weeks or months and heal with scarring.
Major aphthous ulcers (>10 mm diameter) often persist for weeks or months and heal with scarring.
The tongue
 Glossitis is a red, smooth, sore tongue associated with B12, folate or iron deficiency. It is also seen in infections due to Candida and in riboflavin and nicotinic acid deficiency.
Glossitis is a red, smooth, sore tongue associated with B12, folate or iron deficiency. It is also seen in infections due to Candida and in riboflavin and nicotinic acid deficiency.
 A black hairy tongue is due to a proliferation of chromogenic microorganisms causing brown staining of elongated filiform papillae. The causes are unknown, but heavy smoking and the use of antiseptic mouthwashes have been implicated.
A black hairy tongue is due to a proliferation of chromogenic microorganisms causing brown staining of elongated filiform papillae. The causes are unknown, but heavy smoking and the use of antiseptic mouthwashes have been implicated.
 A geographic tongue is an idiopathic condition occurring in 1–2% of the population and may be familial. There are erythematous areas surrounded by well-defined, slightly raised irregular margins. The lesions are usually painless and the patient should be reassured.
A geographic tongue is an idiopathic condition occurring in 1–2% of the population and may be familial. There are erythematous areas surrounded by well-defined, slightly raised irregular margins. The lesions are usually painless and the patient should be reassured.
The gums
 Chronic gingivitis follows the accumulation of bacterial plaque. It resolves when the plaque is removed. It is the most common cause of bleeding gums.
Chronic gingivitis follows the accumulation of bacterial plaque. It resolves when the plaque is removed. It is the most common cause of bleeding gums.
 Acute (necrotizing) ulcerative gingivitis (‘Vincent’s angina’) is characterized by the proliferation of spirochaete and fusiform bacteria associated with poor oral hygiene and smoking. Treatment is with oral metronidazole 200 mg three times daily for 3 days, improved oral hygiene and chlorhexidine gluconate mouthwash.
Acute (necrotizing) ulcerative gingivitis (‘Vincent’s angina’) is characterized by the proliferation of spirochaete and fusiform bacteria associated with poor oral hygiene and smoking. Treatment is with oral metronidazole 200 mg three times daily for 3 days, improved oral hygiene and chlorhexidine gluconate mouthwash.
 Desquamative gingivitis is a clinical description of smooth, red atrophic gingivae caused by lichen planus or mucous membrane pemphigoid. The diagnosis is confirmed by biopsy.
Desquamative gingivitis is a clinical description of smooth, red atrophic gingivae caused by lichen planus or mucous membrane pemphigoid. The diagnosis is confirmed by biopsy.
 Gingival swelling may be due to inflammation or fibrous hyperplasia. The latter may be hereditary (gingival fibromatosis) or associated with drugs (e.g. phenytoin, ciclosporin, nifedipine). Inflammatory swellings are seen in pregnancy, gingivitis and scurvy. Swelling due to infiltration is seen in acute leukaemia and Wegener’s granulomatosis.
Gingival swelling may be due to inflammation or fibrous hyperplasia. The latter may be hereditary (gingival fibromatosis) or associated with drugs (e.g. phenytoin, ciclosporin, nifedipine). Inflammatory swellings are seen in pregnancy, gingivitis and scurvy. Swelling due to infiltration is seen in acute leukaemia and Wegener’s granulomatosis.
The salivary glands
Dry mouth (xerostomia) can result from a variety of causes:
 Drugs (e.g. antimuscarinic, antiparkinsonian, antihistamines, lithium, monoamine oxidase inhibitors, tricyclic and related antidepressants, and clonidine)
Drugs (e.g. antimuscarinic, antiparkinsonian, antihistamines, lithium, monoamine oxidase inhibitors, tricyclic and related antidepressants, and clonidine)
Sialadenitis
Acute sialadenitis is viral (mumps, p. 110) or bacterial. Bacterial sialadenitis is a painful ascending infection with Staphylococcus aureus, Streptococcus pyogenes and Strep. pneumoniae, usually secondary to secretory failure. Pus can be expressed from the affected duct.
The pharynx and oesophagus
Structure and physiology
Swallowing
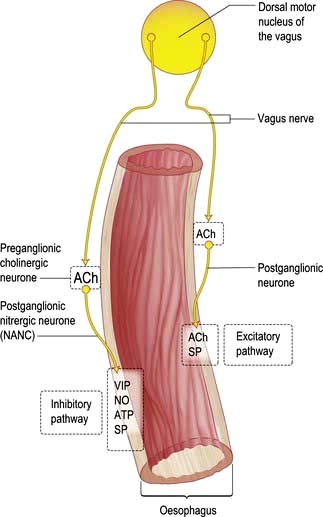
The smooth muscle of the thoracic oesophagus and lower oesophageal sphincter is supplied by vagal autonomic motor nerves consisting of extrinsic preganglionic fibres and intramural postganglionic neurones in the myenteric plexus (Fig. 6.6). There are parallel excitatory and inhibitory pathways.
Symptoms of oesophageal disorders
Major oesophageal symptoms are:
 Dysphagia, or difficulty in swallowing, is defined as a sensation of obstruction during the passage of liquid or solid through the pharynx or oesophagus, i.e. within 15 s of food leaving the mouth. The characteristics of the progression of dysphagia to solids can be helpful, e.g. intermittent slow progression with a history of heartburn suggests a benign peptic stricture; relentless progression over a few weeks suggests a malignant stricture. The slow onset of dysphagia for solids and liquids at the same time suggests a motility disorder, e.g. achalasia (see p. 237). The causes are shown in Table 6.3.
Dysphagia, or difficulty in swallowing, is defined as a sensation of obstruction during the passage of liquid or solid through the pharynx or oesophagus, i.e. within 15 s of food leaving the mouth. The characteristics of the progression of dysphagia to solids can be helpful, e.g. intermittent slow progression with a history of heartburn suggests a benign peptic stricture; relentless progression over a few weeks suggests a malignant stricture. The slow onset of dysphagia for solids and liquids at the same time suggests a motility disorder, e.g. achalasia (see p. 237). The causes are shown in Table 6.3.
 Odynophagia is pain during the act of swallowing and is suggestive of oesophagitis. Causes include reflux, infection, chemical oesophagitis due to drugs such as bisphosphonates or slow-release potassium or associated with oesophageal stenosis.
Odynophagia is pain during the act of swallowing and is suggestive of oesophagitis. Causes include reflux, infection, chemical oesophagitis due to drugs such as bisphosphonates or slow-release potassium or associated with oesophageal stenosis.
 Substernal discomfort, heartburn. This is a common symptom of reflux of gastric contents into the oesophagus. It is usually a retrosternal burning pain that can spread to the neck, across the chest, and when severe can be difficult to distinguish from the pain of ischaemic heart disease. It is often worst lying down at night when gravity promotes reflux or on bending or stooping.
Substernal discomfort, heartburn. This is a common symptom of reflux of gastric contents into the oesophagus. It is usually a retrosternal burning pain that can spread to the neck, across the chest, and when severe can be difficult to distinguish from the pain of ischaemic heart disease. It is often worst lying down at night when gravity promotes reflux or on bending or stooping.
 Regurgitation is the effortless reflux of oesophageal contents into the mouth and pharynx. Uncommon in normal subjects, it occurs frequently in patients with gastro-oesophageal reflux disease or organic stenosis.
Regurgitation is the effortless reflux of oesophageal contents into the mouth and pharynx. Uncommon in normal subjects, it occurs frequently in patients with gastro-oesophageal reflux disease or organic stenosis.
Investigations available for oesophageal disorders
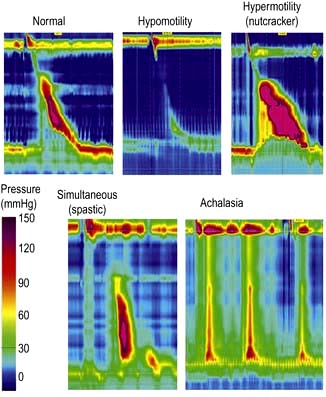
 Manometry (Fig. 6.7) is performed by passing a catheter through the nose into the oesophagus and measuring the pressures generated within the oesophagus. It is used to assess oesophageal motor activity. It is not a primary investigation and should be performed only when the diagnosis has not been achieved by history, barium radiology or endoscopy. Recordings are usually made over a short time period, or much more rarely for up to 24 h. High resolution manometry has superseded conventional manometry and the greater concentration of pressure sensors enables the identification of a wider range of abnormalities of oesophageal function with a greater diagnostic accuracy.
Manometry (Fig. 6.7) is performed by passing a catheter through the nose into the oesophagus and measuring the pressures generated within the oesophagus. It is used to assess oesophageal motor activity. It is not a primary investigation and should be performed only when the diagnosis has not been achieved by history, barium radiology or endoscopy. Recordings are usually made over a short time period, or much more rarely for up to 24 h. High resolution manometry has superseded conventional manometry and the greater concentration of pressure sensors enables the identification of a wider range of abnormalities of oesophageal function with a greater diagnostic accuracy.
 pH monitoring – 24-hour ambulatory monitoring uses a pH-sensitive probe positioned in the lower oesophagus and is used to identify acid reflux episodes (pH <4). Catheter and implantable sensors are available; both are insensitive to alkali. Although only 5–10% of recorded acid reflux episodes are perceived by the patient, pH is a valuable means of correlating episodes of acid reflux with patient’s symptoms.
pH monitoring – 24-hour ambulatory monitoring uses a pH-sensitive probe positioned in the lower oesophagus and is used to identify acid reflux episodes (pH <4). Catheter and implantable sensors are available; both are insensitive to alkali. Although only 5–10% of recorded acid reflux episodes are perceived by the patient, pH is a valuable means of correlating episodes of acid reflux with patient’s symptoms.
 Impedance uses a catheter to measure the resistance to flow of ‘alternating current’ in the contents of the oesophagus. Combined with pH it allows assessment of acid, weakly acid, alkaline and gaseous reflux, which is helpful in understanding the symptoms that are produced by a non-acid reflux. Treatment is, however, still difficult in these conditions.
Impedance uses a catheter to measure the resistance to flow of ‘alternating current’ in the contents of the oesophagus. Combined with pH it allows assessment of acid, weakly acid, alkaline and gaseous reflux, which is helpful in understanding the symptoms that are produced by a non-acid reflux. Treatment is, however, still difficult in these conditions.
Gastro-oesophageal reflux disease (GORD)
Pathophysiology
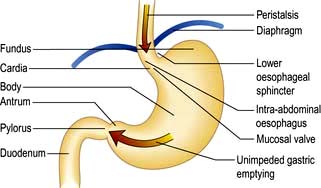
Between swallows, the muscles of the oesophagus are relaxed except for those of the sphincters. The LOS remains closed due to the unique property of the muscle and relaxes when swallowing is initiated. Transient Lower Oesophageal Sphincter Relaxations (TLESRs) are part of normal physiology, but occur more frequently in GORD patients (Fig. 6.8).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree