Normal porta hepatis and cystic duct anatomy. (With permission from Mulholland MW, Lillemoe KD, Doherty GM, Maier RV, Upchurch GR, eds. Greenfield’s Surgery. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005.)
•The most common hepatic ductal anomaly is either of the right sectoral ducts (i.e., anterior or posterior) draining directly into the CBD (16% to 20%)
•The cystic duct usually joins the common hepatic duct approximately 2 to 4 cm distal to the bifurcation of the right and left hepatic ducts. Common variants include:
•Joins the middle 1/3 of the hepatic duct at an angle (75%)
•Fused to the hepatic duct along a parallel course (20%)
•Spiral course to enter at the left side (5%)
•Most rarely, the cystic duct can empty in the proximal hepatic duct or directly into the right hepatic duct (0.3%)
Porta Hepatis Anatomy
•The portal triad
•Portal vein—posterior
•CBD—lateral
•Common hepatic artery—medial and anterior
•Portal venous anatomy is relatively constant and has much less variation than the biliary ductal and hepatic arterial systems
What is the most common hepatic artery anomaly?
A replaced right hepatic artery occurs in 15% to 20% of the population and originates from the superior mesenteric artery (SMA).
Hepatic Artery Anomalies
•Definitions
•Replaced artery: A substitute for the normal/usual hepatic artery, which is absent
•Accessory artery: Appears in addition to one that is normally/usually present
•Normal anatomy present in 51% to 76%
•Replaced right hepatic artery originating from the SMA
•The most common anomaly
•10.6% to 21% of people
•Runs behind the head and uncinate process of the pancreas
•Courses posterolateral to the CBD
•If in question, can aspirate with 25G needle
•Replaced left hepatic artery originating from the celiac trunk
•4.6% to 18% of people
•Accessory left hepatic artery originating from left gastric artery
•8% to 18% of people
•Accessory right hepatic artery
•7% of people
•Replaced common hepatic artery originating from the SMA
•1.4% to 5% of people
•Anterior location of right hepatic artery
•The artery originates from the proper hepatic artery and courses anterior to the common hepatic duct
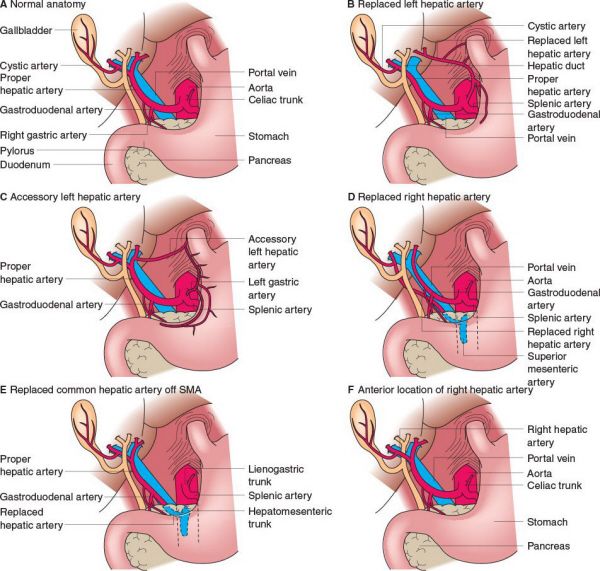
Variations in hepatic artery anatomy. (A) Normal anatomy. (B) Replaced left hepatic artery originating from the left gastric artery. (C) Accessory left hepatic artery originating from the left gastric artery in addition to the normal arterial supply. (D) Replaced right hepatic artery originating from the SMA. (E) Replaced common hepatic artery originating from the SMA. (F) Anterior location of the right hepatic artery (courses anterior to the common hepatic duct). (With permission from Mulholland MW, Lillemoe KD, Doherty GM, Maier RV, Upchurch GR, eds. Greenfield’s Surgery. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005.)
A replaced left hepatic artery is a potential pitfall during a Nissen fundoplication and a replaced right hepatic artery is a potential pitfall during a pancreaticoduodenectomy.
What layers of the bowel are not present in the gallbladder (GB) wall?
The GB lacks a submucosa and muscularis mucosa.
Layers of the Gallbladder
•The GB has a mucosa, a muscularis propria, a perimuscular subserosal connective tissue, and a serosa
•It lacks the submucosa and muscularis mucosa layers
•The lack of submucosa makes the GB wall weaker than the intestinal wall
•Rokitansky-Aschoff sinuses—form from the invagination of the epithelium through the fibromuscular layer as a result of inflammation and increased pressure in the GB (e.g., during cholecystitis)
•During cholecystectomy, the plane of dissection is the subserosal plane and therefore, all T2 and higher GB cancers require additional resection if a cancer is incidentally identified following a cholecystectomy
What is the blood supply of the CBD?
The CBD has a segmental blood supply.
Blood Supply of the Common Bile Duct
•Derived inferiorly from the gastroduodenal artery—the main blood supply
•Derived superiorly from the right hepatic artery
•Supply blood vessels on the CBD are located at the cross-sectional 3 and 9 o’clock positions
•Occasionally, these may need to be oversewn when performing a bile duct resection or pancreaticoduodenectomy
Upon an ultrasound examination for cholelithiasis, a 5-mm CBD is noted. What is the normal diameter of the CBD?
A normal CBD is 4 to 6 mm in diameter, with a couple of exceptions.
Common Bile Duct Size
•A normal CBD is up to 4 to 6 mm
•Add 1 mm per decade over 50 to the normal CBD size
•The CBD is normally enlarged status post cholecystectomy
•The size of the CBD accommodates for the removed GB
•Ultrasound is the best method for determining CBD size
When performing a manual Pringle maneuver, what structure is located directly posterior to the surgeon’s finger in the foramen of Winslow?
The inferior vena cava is directly posterior to the porta hepatis.
What is the average volume of daily bile production per day?
Approximately 600 to 1,000 mL of bile is produced each day.
What is the source of routine bilirubin formation?
80% of bilirubin is derived from hemoglobin.
20% of bilirubin is derived from hemoproteins and a small pool of free heme.
What is the most common element in bile?
Bile is 90% water.
Composition of Bile
•Iso-osmotic (about 300 mOsm)
•pH 7.8
•Water 90%
•Electrolytes 10%
•Bile is high in: Na, K, HCO3
•Bile is low in: Cl, Ca, Mg
•At higher flow rates, stimulated by secretin and vasoactive intestinal peptide, [HCO3] increases and [Cl] decreases
•Organic solutes
•Primary and secondary bile acids > phospholipids [lecithin] > cholesterol > proteins > bilirubin
•Bile acid pool: Approximately 5 g
•Recirculate in enterohepatic circulation approximately every 4 hours
•0.5 g (10%) of bile acids lost in stool each day
What are the primary bile acids? What are the secondary bile acids?
The primary bile acids are cholic acid and chenodeoxycholic acid.
The secondary bile acids are deoxycholic, lithocholic, and ursodeoxycholic acid.
Where are secondary bile acids synthesized?
Small intestine.
Primary Bile Acids
•Cholic acid and chenodeoxycholic acid
•Synthesized from cholesterol in the liver
•The rate-limiting enzyme in bile acid production is cholesterol 7α-hydroxylase
•Each of these comprise approximately 40% of bile acids
•Conjugated with either glycine or taurine in the liver to render them more useful for fat digestion and absorption
Secondary Bile Acids
•Deoxycholic acid, lithocholic acid, and ursodeoxycholic acid
•Synthesized in the small intestine from primary bile acids via intestinal bacterial enzymes
•Conjugated with either glycine or taurine in the liver for fat emulsification
•Note that lithocholic acid is insoluble and lost in stool
•Bile is reabsorbed in the terminal ileum/colon in order to enter the enterohepatic circulation
•Bile acids are resorbed via an Na-dependent bile salt transporter
•They are then returned to the liver via portal venous flow
Hemoglobin Degradation
•Hgb  heme
heme  biliverdin
biliverdin  bilirubin
bilirubin
•Free, unconjugated bilirubin undergoes glucuronidation (glucuronyl transferase) to the conjugated, water soluble form that is excreted
•Conjugated bilirubin is actively secreted in bile
•Urobilinogen
•Breakdown of bilirubin by bacteria in the terminal ileum  resorption of bilirubin into blood
resorption of bilirubin into blood  release of bilirubin in urine
release of bilirubin in urine
What is the main type of bile pigment?
Bilirubin glucuronide (via conjugation of bilirubin to glucuronic acid by glucuronic transferase).
What are the main functions of bile?
•Fat emulsification
•Aids with absorption of lipid-soluble vitamins A, D, E, and K
•Excretion of bilirubin derived from senescent erythrocytes
•Cholesterol excretion via transport in biliary lecithin vesicles
What is the principal hormone involved in GB contraction?
Cholecystokinin (CCK) is the main hormone involved in GB contraction.80% of the GB empties within 2 hours post-prandially.
The Gallbladder and Pregnancy
•GB contraction is decreased in the second half of the menstrual cycle and the third trimester of pregnancy
•There are more gallstones, sludge, and cholesterol content in bile, derived from estrogen, during pregnancy
•Optimal timing for the operation is during the second trimester
What happens to the enterohepatic circulation following a cholecystectomy?
The enterohepatic circulation increases to accommodate increased bile flow into the small bowel.
Changes Status Post-cholecystectomy
•CBD dilatation
•Decreased bile acid pool
•More continuous flow of bile into the intestine
•Cholesterol solubility in the bile increases
•Bile acid secretion increases
•Enterohepatic recycling increases
A 25-year-old male with no past medical history presents after a football injury with a ulnar fracture. He undergoes reduction of the fracture, but postoperatively is noted to have an elevated bilirubin of 4.0; his other LFTs are normal. You fractionate the bilirubin and the conjugated portion is 0.5 and the unconjugated portion is 3.5. Does this need further workup?
This patient has Gilbert syndrome, which results in elevation of unconjugated (indirect) bilirubin, particularly after stress. No further workup is needed.
Unconjugated Hyperbilirubinemia
•Causes: Hemolysis, hepatic deficiency of uptake or conjugation
•Gilbert disease
•Abnormal bilirubin uptake in the liver
•Hyperbilirubinemia, particularly during stress
•Usually asymptomatic; no treatment needed
•Crigler-Najjar disease
•Inability to conjugate bilirubin secondary to a glucuronyl transferase deficiency
•Have high unconjugated bilirubin
•A life-threatening disease
•Physiologic jaundice of a newborn
•Due to immature glucuronyl transferase
Conjugated Hyperbilirubinemia
•Causes: Secretion defects into bile ducts, excretion defects into GI tract (stones, stricture, tumor)
•Rotor syndrome
•Deficiency in storage ability
•Dubin-Johnson syndrome
•Deficiency in secretion ability
A 41-year-old obese Native American woman underwent resection of her terminal ileum for Crohn’s disease and was maintained on TPN for 6 weeks. What is her predisposition to have cholelithiasis?
She has multiple risk factors for cholelithiasis.
Risk Factors for Cholelithiasis
•Middle age
•Female
•Obesity
•Rapid weight loss (secondary to GB sludge)
•Exogenous estrogen
•Pregnancy
•Terminal ileum resection
•Total parenteral nutrition (cholestasis leads to increased pigmented stone formation)
•Truncal or hepatic branch vagotomy (loss of cholinergic stimulation for GB contraction leads to stasis)
•Genetic susceptibility to cholesterol stone formation (e.g., Native Americans)
•Cirrhosis
•Crohn’s disease
•Hereditary spherocytosis
•Hemolytic anemia
•Gallstones in obese people with no other risk factors: Usually secondary to overactive HMG Co-A reductase
•Gallstones in thin people with no other risk factors: Due to underactive 7α-hydroxylase
What types of gallstones are most common following a terminal ileum resection?
Pigmented stones.
Gallstones
•Cholesterol stones (most common)
•Yellow stones
•Recurrent stones are usually cholesterol stones
•Due to a failure of cholesterol and calcium salts to remain in solution as a result of an imbalance of cholesterol, lecithin, and bile acids (relatively increased cholesterol)
•Pure cholesterol stones
•Nearly 100% cholesterol
•Typically multiple with bumpy, spheroid, or faceted shape
•Mixed cholesterol stones
•≥70% cholesterol
•Typically single, ovoid, spherical
•Dark stones due to calcium bilirubinate, i.e., a precipitation of unconjugated bilirubin with Ca
•Most contain <20% cholesterol
•Causes
•Congenital or acquired hemolytic anemia (i.e., sickle cell disease or thalassemia)
•Higher incidence after terminal ileum resection
•Crohn’s disease (secondary to bile salt malabsorption)
•Black pigment stones
•Jet black, brittle, and spiculated shape
•Generally form in the GB
•May contain polymerized bile pigments
•Found with cirrhosis, hemolysis, Crohn’s disease, long-term TPN administration
•Brown pigment stones
•Brown or brownish-yellow with a soft or malleable consistency
•Pliable due to a higher percent composition of cholesterol and calcium palmitate (bacterial derived)
•Associated with infected bile and are largely composed of bacterial cell bodies and precipitated calcium bilirubinate
•Also associated with parasitic infections (Opisthorchis viverrini, Clonorchis sinensis, and Ascaris lumbricoides)
•Generally form in the bile ducts and result in CBD stones
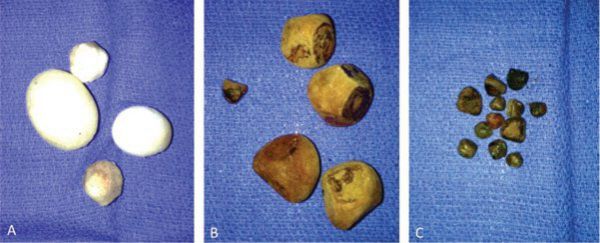
(A) Cholesterol gallstones. (B) Brown pigment gallstone. (C) Black pigment gallstones.
What is the best laboratory test for biliary obstruction?
Alkaline phosphatase. It can also be elevated during childhood, pregnancy, and due to primary/metastatic bone malignancies.
Differential Diagnosis of Conjugated Hyperbilirubinemia
•Choledocholithiasis
•Intrinsic or extrinsic periampullary, biliary, or hepatic tumors
•Primary sclerosing cholangitis (PSC)
•Parasitic infections (adult A. lumbricoides or eggs of C. sinensis or Fasciola hepatica)
•AIDS cholangiopathy (Cryptosporidium, CMV, or HIV)
•Biliary stricture
•Sepsis
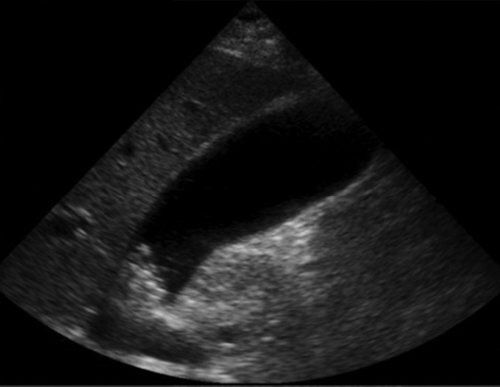
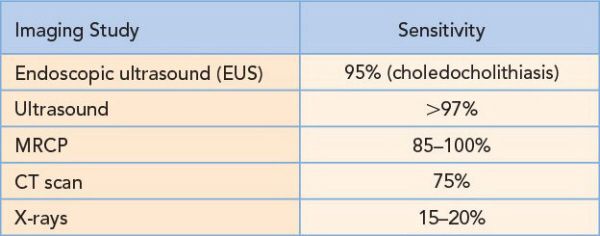
What is the imaging method of choice for the initial workup of right upper quadrant pain?
RUQ ultrasound is the imaging study of choice for patients with RUQ pain. It is useful in diagnosing cholelithiasis, cholecystitis, liver masses, and pyelonephritis.
Imaging Studies for Gallstones
A 43-year-old obese woman presents to the emergency department with right upper quadrant pain. Her pain is colicky in nature, has been intermittent for several months, and is worse after consuming fatty foods. She has no fever or leukocytosis. An abdominal ultrasound confirms gallstones in the GB. What is the next step in her management?
Discharge the patient with dietary instructions to avoid fatty foods and to take analgesics as needed. An elective cholecystectomy should be planned for symptomatic cholelithiasis. Admission to the hospital is generally reserved for patients who cannot tolerate a regular diet or have severe pain.
Cholelithiasis
•Defined as the presence of gallstones within the GB
•Typically asymptomatic (8% to 15% prevalence in the general population)
•
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


