Fluid, Electrolyte, and Acid-Base Imbalances
Learning Objectives
After studying this chapter, the student is expected to:
1. Explain the movement of water between body compartments that results in edema.
2. Describe the causes and effects of dehydration.
3. Explain the meaning of third-spacing.
4. Discuss the causes and signs of hyponatremia and hypernatremia.
5. Explain the causes and signs of hypokalemia and hyperkalemia.
6. Describe the causes and signs of hypocalcemia and hypercalcemia.
9. Explain how decompensation develops and its effects on the central nervous system.
Key Terms
aldosterone
anion
anorexia
antidiuretic hormone (ADH)
ascites
atrial natriuretic peptide
capillary permeability
carpopedal spasm
cation
diffusion
diuretic
dysrhythmia
electrocardiogram
extracellular
filtration
hydrogen ions
hydrostatic pressure
hypertonic/hyper-osmolar
hypervolemia
hypothalamus
hypotonic/hypo-osmolar
hypovolemia
interstitial fluid
intracellular
intravascular fluid
isotonic/iso-osmolar
laryngospasm
milliequivalent (mEq)
nonvolatile metabolic acids
osmoreceptor
osmosis
osmotic pressure
paresthesias
skin turgor
tetany
transcellular
Fluid Imbalance
Review of Concepts and Processes
Water is a major component of the body and is found both within and outside the cells. It is essential to homeostasis, the maintenance of a relatively constant and favorable environment for the cells. Water is the medium within which metabolic reactions and other processes take place. It also comprises the transportation system for the body. For example, water carries nutrients into cells and removes wastes, transports enzymes in digestive secretions, and moves blood cells around the body. Without adequate fluid, cells cannot continue to function, and death results. Fluid also facilitates movement of body parts, for example, the joints and the lungs.
Fluid Compartments
Although the body appears to be a solid object, approximately 60% of an adult’s body weight consists of water, and an infant’s body is about 70% water (Table 2-1). Female bodies, which contain a higher proportion of fatty tissue, have a lower percentage of water than male bodies. The elderly and the obese also have a lower proportion of water in their bodies. Individuals with less fluid reserve are more likely to be adversely affected by any fluid or electrolyte imbalance.
TABLE 2-1
Fluid Compartments in the Body
| Volume | Approximate Percentage of Body Weight | |||
| Adult Male (L) | Male (%) | Female (%) | Infant (%) | |
| Intracellular fluid | 28 | 40 | 33 | 40 |
| Extracellular fluid | 15 | 20 | 17 | 30 |
| Plasma | (4.5) | (4) | (4) | (4) |
| Interstitial fluid | (10.5) | (15) | (9) | (25) |
| Other | (1) | (1) | (1) | |
| Total water | 43 | 60 | 50 | 70 |
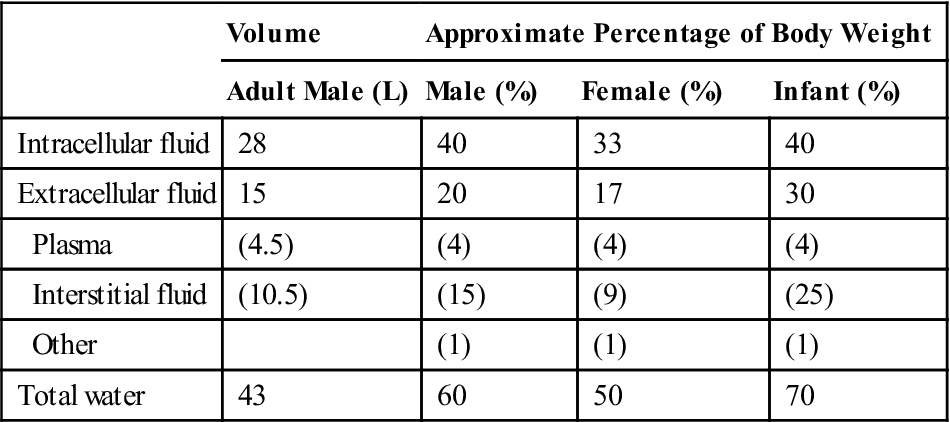
Note: In elderly women, water content is reduced to approximately 45% of body weight.
Fluid is distributed between the intracellular compartment (ICF), or fluid inside the cells, and the extracellular compartment (ECF). See Ready Reference 1 for a diagram showing fluid compartments of the body.
In an adult male, blood constitutes about 4% of body weight and interstitial fluid about 15%; the remaining transcellular fluids amount to about 1% of total body weight. Water constantly circulates within the body and moves between various compartments. For example, CSF forms continuously from the blood and is reabsorbed back into the general circulation. A large volume of water (up to 8 liters in 24 hours) is present in the digestive secretions entering the stomach and small intestine, and this fluid is reabsorbed in the colon, making up a very efficient water-recycling system.
Movement of Water
To maintain a constant level of body fluid, the amount of water entering the body should equal the amount of water leaving the body. Fluid is added to the body through the ingestion of solid food and fluids and as a product of cell metabolism (Table 2-2). Fluid is lost in the urine and feces as well as through insensible (unapparent) losses through the skin (perspiration) and exhaled air.
TABLE 2-2
| Sources (mL) | Losses (mL) | ||
| Liquids | 1200 | Urine | 1400 |
| Solid foods | 1000 | Feces | 200 |
| Cell metabolism | 300 | Insensible losses | |
| Lungs | 400 | ||
| Skin | 500 | ||
| Total | 2500 | 2500 | |
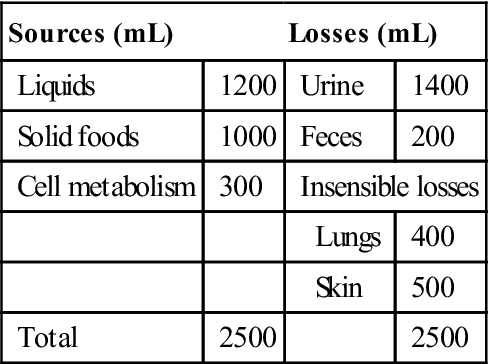
Control of fluid balance is maintained by:
• The hormone, antidiuretic hormone (ADH), which controls the amount of fluid leaving the body in the urine (see Chapters 16 and 18); ADH promotes reabsorption of water into the blood from the kidney tubules
• The hormone atrial natriuretic peptide (ANP) is a hormone synthesized and released by the myocardial cells in the atrium of the heart. Its role in homeostasis relates to reduction of workload on the heart by regulating fluid, sodium, and potassium levels. In the kidney ANP increases glomerular filtration rate (GFR) by altering pressure in the glomerular capillaries; it also reduces the reabsorption of sodium in the distal convoluted tubules through inhibition of antidiuretic hormone (ADH). Renin secretion is also reduced and thus the renin angiotensin system is inhibited. The result is fluid loss from the extracellular compartment and lowered blood pressure. It also reduces aldosterone secretion, leading to retention of potassium. Research has shown that ANP is elevated in patients with congestive heart failure who have increased blood volume in the atria (see Chapter 12). Research is ongoing on this peptide and its possible use in the treatment of hypertension and congestive heart failure.
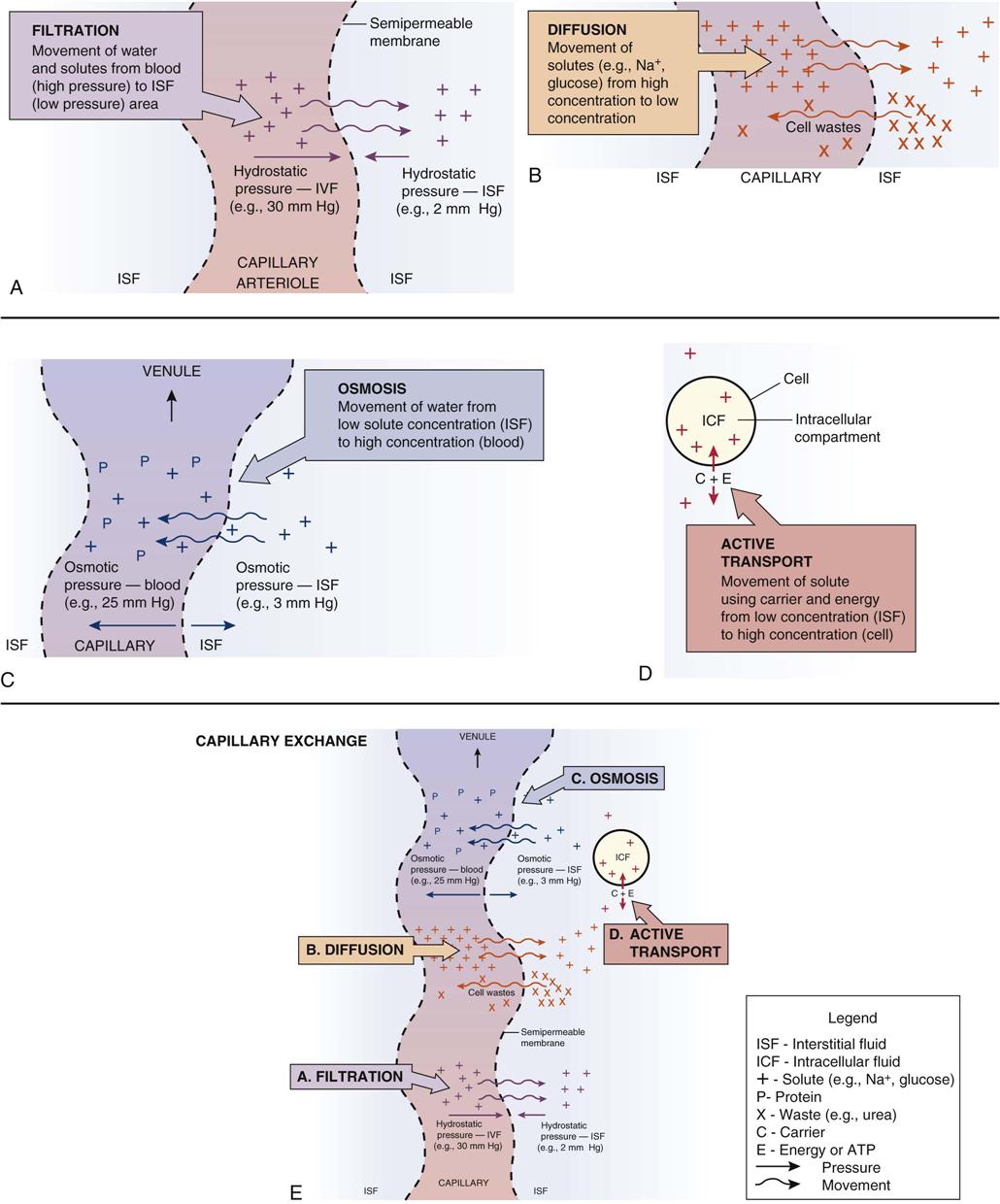
Fluid constantly circulates throughout the body and moves relatively freely, depending on the permeability of the membranes between compartments, by the processes of filtration or osmosis (Fig. 2-1). Water moves between the vascular compartment or blood and the interstitial compartment through the semipermeable capillary membranes, depending on the relative hydrostatic and osmotic pressures within the compartments (see Fig. 2-1). Proteins and electrolytes contribute to the osmotic pressure of a fluid and therefore are very important in maintaining fluid volumes in various compartments. Hydrostatic pressure may be viewed as the “push” force and osmotic pressure as the “pull” or attraction force in such fluid movements. Changes in either force will alter fluid movement and volume in the compartments.
At the arteriolar end of the capillary, the blood hydrostatic pressure (or blood pressure) exceeds the opposing interstitial hydrostatic pressure and the plasma colloid osmotic pressure of the blood, and therefore fluid moves out from (or is “pushed” out of) the capillary into the interstitial compartment. At the venous end of the capillary, the blood hydrostatic pressure is greatly decreased and osmotic pressure higher, and therefore fluid tends to shift (or is “pulled”) back into the capillary. It is easier to remember the direction of movement if one thinks of the movement of nutrients and oxygen out of the arterial blood toward the cells and the flow of wastes and carbon dioxide from the cell back into the venous blood. Excess fluid and any protein in the interstitial compartment is returned to the circulation through the lymphatic capillaries.
Many cells have mechanisms to control intracellular volume. A major factor in the movement of water through cell membranes is the difference in osmotic pressure between the cell and the interstitial fluids. As the relative concentrations of electrolytes in the interstitial fluid and intracellular fluid change, the osmotic pressure also changes, causing water to move across the cell membrane by osmosis. For example, if an erythrocyte is placed in a dilute hypotonic solution (low osmotic pressure), water may enter the cell, causing it to swell and malfunction.
Fluid Excess—Edema
Fluid excess occurs in the extracellular compartment and may be referred to as isotonic/iso-osmolar, hypotonic/hypo-osmolar, or hypertonic/hyper-osmolar, depending on the cause. The osmolarity or the concentration of solute in the fluid, affects fluid shifts between compartments, including the cells.
Edema refers to an excessive amount of fluid in the interstitial compartment, which causes a swelling or enlargement of the tissues. Edema may be localized in one area or generalized throughout the body. Depending on the type of tissue and the area of the body, edema may be highly visible or relatively invisible, or not accurately reflect the amount of fluid hidden in the area; for example, facial edema is usually visible but edema of the liver or a limb may not be. Edema is usually more severe in dependent areas of the body, where the force of gravity is greatest, such as the buttocks, ankles, or feet of a person in a wheelchair. Prolonged edema interferes with venous return, arterial circulation, and cell function in the affected area.
Causes of Edema
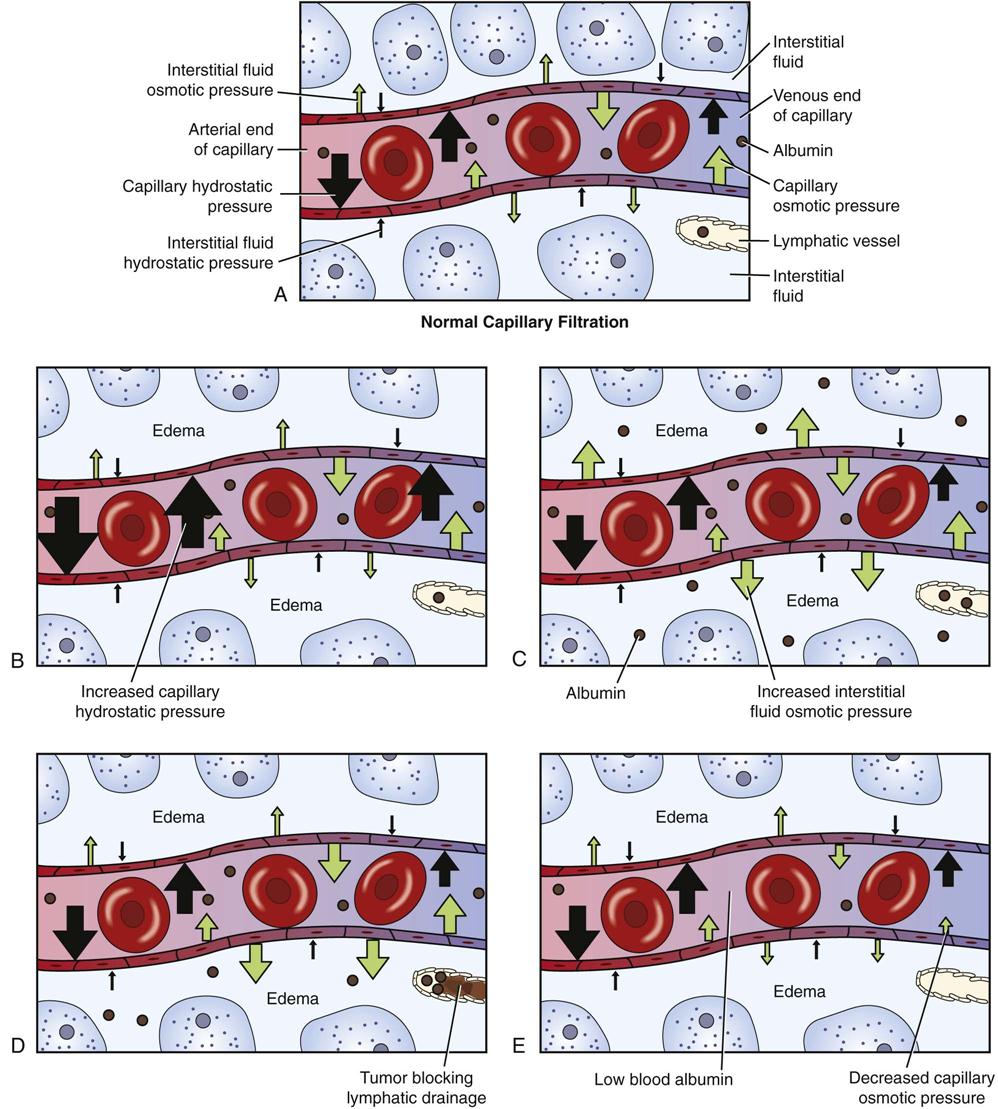
Edema has four general causes (Fig. 2-2).
1. The first cause is increased capillary hydrostatic pressure (equivalent to higher BP or blood pressure), which prevents return of fluid from the interstitial compartment to the venous end of the capillary, or forces excessive amounts of fluid out of the capillaries into the tissues. The latter is a cause of pulmonary edema, in which excessive pressure, often due to increased blood volume, can force fluid into the alveoli, interfering with respiratory function.
Specific causes of edema related to increased hydrostatic pressure include increased blood volume (hypervolemia) associated with kidney failure, pregnancy, congestive heart failure, or administration of excessive fluids. In pregnancy, the enlarged uterus compresses the pelvic veins in the seated position and when a pregnant woman must stand still for long periods of time, the pressure in the leg veins can become quite elevated, causing edema in the feet and legs. In some people with congestive heart failure, the blood cannot return easily through the veins to the heart, raising the hydrostatic pressure in the legs and abdominal organs and causing ascites, or fluid in the abdominal cavity.
2. Second, edema may be related to the loss of plasma proteins, particularly albumin, which results in a decrease in plasma osmotic pressure. Plasma proteins usually remain inside the capillary and seldom move through the semipermeable capillary membrane. The presence of fewer plasma proteins in the capillary allows more fluid to leave the capillary and less fluid to return to the venous end of the capillary.
Protein may be lost in the urine through kidney disease, or synthesis of protein may be impaired in patients with malnutrition and malabsorption diseases or with liver disease. Protein levels may drop acutely in burn patients who have large areas of burned skin; the subsequent inflammation and loss of the skin barrier allow protein to easily leak out of the body.
Frequently excessive sodium levels in the extracellular fluid accompany the two causes just mentioned. When sodium ions are retained, they promote accumulation of fluid in the interstitial compartment by increasing the ISF osmotic pressure and decreasing the return of fluid to the blood. Blood volume and blood pressure are usually elevated as well. High sodium levels are common in patients with heart failure, high blood pressure, kidney disease, and increased aldosterone secretion.
4. The fourth cause of edema is increased capillary permeability. This usually causes localized edema and may result from an inflammatory response or infection (see Chapter 5). In this case, histamine and other chemical mediators released from cells following tissue injury cause increased capillary permeability and increased fluid movement into the interstitial area. Protein also leaks into the interstitial compartment, increasing the osmotic pressure in ISF and thus holding more fluid in the interstitial area. A general increase in capillary permeability can result from some bacterial toxins or large burn wounds, leading to both hypovolemia and shock.
Effects of Edema
• A local area of swelling may be visible and may be very pale or red in color, depending on the cause (Table 2-3).
• In people with generalized edema there is a significant increase in body weight, which may indicate a problem before there are other visible signs (see Fig. 2-3).
• With sustained edema the arterial circulation may be impaired. The increased interstitial pressure may restrict arterial blood flow into the area, preventing the fluid shift that carries nutrients into the cells. This can prevent normal cell function and reproduction and eventually results in tissue necrosis or the development of ulcers. This situation is evident in individuals with severe varicose veins in the legs—large, dilated veins that have a high hydrostatic pressure. Varicose veins can lead to fatigue, skin breakdown, and varicose ulcers (see Chapter 12). These ulcers do not heal easily because of the continued insufficient blood supply.
• Edematous tissue in the skin is very susceptible to tissue breakdown from pressure, abrasion, and external chemicals. Proper skin care is essential to prevent ulceration, particularly in an immobilized patient (see Chapter 25).
TABLE 2-3
Comparison of Signs and Symptoms of Fluid Excess (Edema) and Fluid Deficit (Dehydration)
| Fluid Excess (Edema) | Fluid Deficit (Dehydration) |
| Localized swelling (feet, hands, periorbital area, ascites) | Sunken, soft eyes |
| Pale, gray, or red skin color | Decreased skin turgor, dry mucous membranes |
| Weight gain | Thirst, weight loss |
| Slow, bounding pulse; high blood pressure | Rapid, weak, thready pulse, low blood pressure, and orthostatic hypotension |
| Lethargy, possible seizures | Fatigue, weakness, dizziness, possible stupor |
| Pulmonary congestion, cough, rales | Increased body temperature |
| Laboratory values: | Laboratory values: |
| Decreased hematocrit | Increased hematocrit |
| Decreased serum sodium | Increased electrolytes (or variable) |
| Urine: low specific gravity, high volume | Urine: high specific gravity, low volume |
Note: Signs may vary depending on the cause of the imbalance.
Fluid Deficit—Dehydration
Dehydration refers to insufficient body fluid resulting from inadequate intake or excessive loss of fluids or a combination of the two. Losses are more common and affect the extracellular compartment first. Water can shift within the extracellular compartments. For example, if fluid is lost from the digestive tract because of vomiting, water shifts from the vascular compartment into the digestive tract to replace the lost secretions. If the deficit continues, eventually fluid is lost from the cells, impairing cell function.
Fluid loss is often measured by a change in body weight; knowing the usual body weight of a person is very helpful in assessment of the extent of loss. As a general guide to extracellular fluid loss, a mild deficit is defined as a decrease of 2% in body weight, a moderate deficit as a 5% weight loss, and severe dehydration is a decrease of 8%. This figure should be adjusted for the individual’s age, body size, and condition.
Dehydration is a more serious problem for infants and elderly people, who lack significant fluid reserves as well as the ability to conserve fluid quickly. Infants also experience not only greater insensible water losses through their proportionately larger body surface area but also an increased need for water owing to their higher metabolic rate. The vascular compartment is rapidly depleted in an infant (hypovolemia), affecting the heart, brain, and kidneys. This is indicated by decreased urine output (number of wet diapers), increased lethargy, and dry mucosal membranes.
Water loss is often accompanied by a loss of electrolytes and sometimes of proteins, depending on the specific cause of the loss. For example, sweating results in a loss of water and sodium chloride. Electrolyte losses can influence water balance significantly because electrolyte changes lead to osmotic pressure change between compartments. To restore balance, electrolytes as well as fluid must be replaced. Isotonic dehydration refers to a proportionate loss of fluid and electrolytes, hypotonic dehydration to a loss of more electrolytes than water, and hypertonic dehydration to a loss of more fluid than electrolytes. The latter two types of dehydration cause signs of electrolyte imbalance and influence the movement of water between the intracellular and extracellular compartments (see Electrolyte Imbalances).
Causes of Dehydration
Common causes of dehydration include:
Effects of Dehydration
Initially, dehydration involves a decrease in interstitial and intravascular fluids. These losses may produce direct effects such as:
• Dry mucous membranes in the mouth (see Table 2-3)
Decreased skin turgor or elasticity (Fig. 2-4)
• Lower blood pressure, weak pulse, and a feeling of fatigue
The body attempts to compensate for the fluid loss by:
Third-Spacing: Fluid Deficit and Fluid Excess
Third-spacing refers to a situation in which fluid shifts out of the blood into a body cavity or tissue where it is no longer available as circulating fluid. Examples include peritonitis, the inflammation and infection of the peritoneal membranes, and burns. The result of this shift is a fluid deficit in the vascular compartment (hypovolemia) and a fluid excess in the interstitial space. Until the basic cause is removed, fluid remains in the “third space”—in the body, but is not a functional part of the circulating fluids. Simply weighing the patient will not reflect this shift in fluid distribution. Laboratory tests such as hematocrit and electrolyte concentrations will indicate third-spacing. In the case of burns, the third spacing is evident as edema in the area of the wounds.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree