Female Genital and Reproductive Function
Rosemary A. Jadack
Key Questions
• What are the major structures of the internal and the external female reproductive tract?
• What are the major hormonal events of the female reproductive cycle?
• What are the physiologic changes associated with pregnancy?
• What gestational events occur in the fetus during each of the three trimesters of pregnancy?
• What hormonal changes lead to menopause?
• What physiologic changes and complications may result from menopausal hormone deficiencies?
![]()
http://evolve.elsevier.com/Copstead/
The female reproductive system is complex both in structure and in function. From birth to senescence, the organs of the female reproductive system function in concert with each other, with the brain, and with other endocrine organs. This integrated functioning constitutes some of the most intricate and elegant processes of the human body. This chapter presents an overview of these functions, beginning with the development of the female reproductive tract.
The major processes related to the reproductive tract throughout life, including the menstrual cycle, pregnancy, lactation, and menopause, are then described with an emphasis on recent research findings. Health care providers must also consider the developmental, cognitive, functional, social, and financial aspects of women’s reproductive lives.1–3 Because the functioning of the female reproductive system has an enormous impact on the life of the individual woman, increased importance has been placed on the active involvement of women in understanding their own health care needs. Health care professionals are encouraged to include women as collaborators in decisions about their reproductive health.4,5
Reproductive Structures
Organization of the Female Reproductive Organs
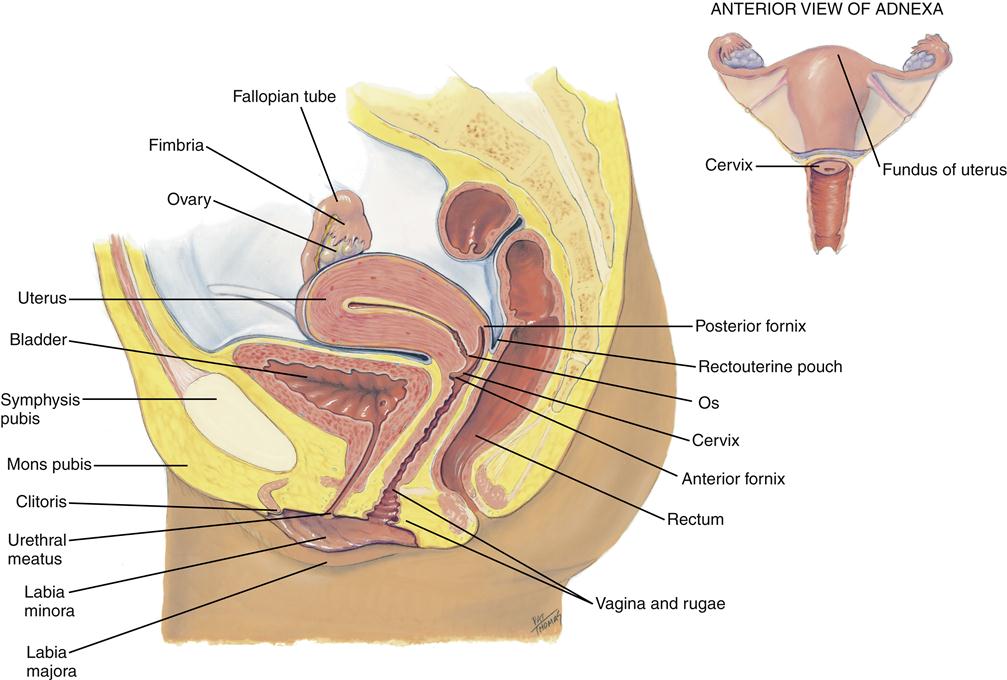
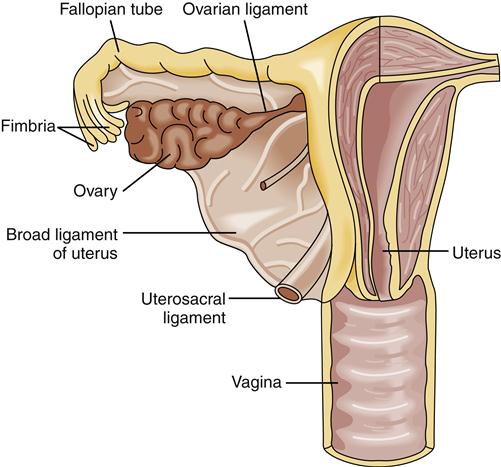
The internal organs of the female reproductive system include the ovaries, oviducts (fallopian tubes), uterus, cervix, and vagina (Figure 32-1). These organs are situated in the pelvic cavity and are supported and anchored in place by a series of ligaments (Figure 32-2).
Ovaries
The two ovaries, which are the female gonads, are located close to the lateral walls of the pelvic cavity. When the ovary is in its normal position, its long axis is nearly vertical with respect to the horizontal axis of the body. The size of the ovary varies with age and with the stage of the menstrual cycle. It is somewhat larger before than after pregnancy and further reduces in size with the aging process.6
The ovary is covered with a single layer of epithelium. Underneath the epithelium is a layer of dense fibrous connective tissue called the tunica albuginea. The tunica albuginea constitutes the outer portion of the cortex of the ovary. The remainder of the cortex consists of connective tissue called the stroma, which contains ova in various stages of maturation. The innermost part of the ovary, the medulla, consists of loose connective tissue that is richly supplied with blood and lymph vessels and nerve fibers.7
Before birth, hundreds of thousands of oogonia (cells that develop into ova) are present in the ovaries. Thus the entire lifetime supply of ova is established during embryonic development; no new oogonia arise after birth. Each oogonium is surrounded by a cluster of granulosa cells. The oogonium and its granulosa cells constitute a follicle. During prenatal development, the oogonia increase in size and become primary oocytes. By the time of full gestational development, the primary oocytes are in the prophase of the first meiotic division. Ovarian follicular development is shown in Figure 32-3. During childhood and into adult life, the oocytes enter a nonactive phase. After puberty, a few of the oocytes develop in follicles each month in response to follicle-stimulating hormone (FSH) secreted by the anterior pituitary gland. The vast majority of follicles and their oocytes die by atresia. Generally, each month, only one mature follicle will develop to eject an oocyte through the wall of the ovary in the process of ovulation, which is described in more detail in the Menstrual Cycle section.
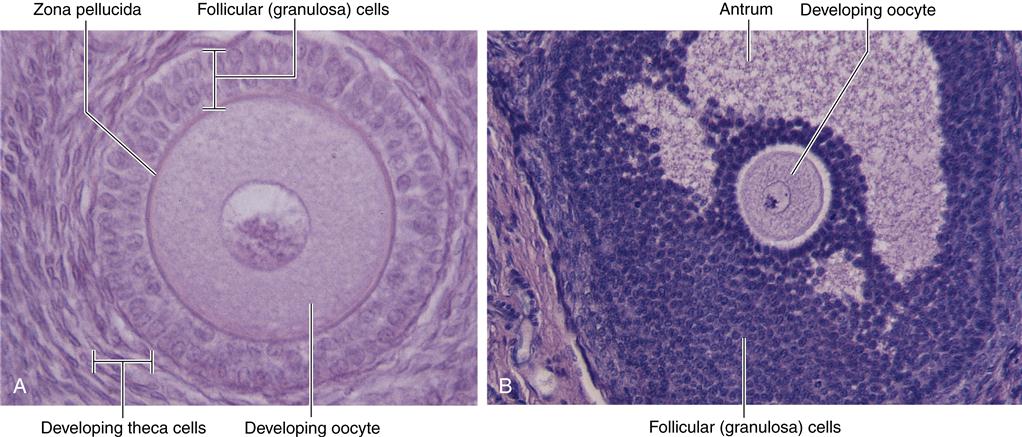
Female gametes mature within follicles in the outer region of an ovary. Follicles in early stages of development (A) and late stages of development (B) exhibit a developing oocyte (immature ovum) surrounded by hormone-secreting follicular (granulosa) cells. Notice that the more mature ovarian follicle in (B) has a fluid-filled cavity called the antrum. (From Patton KT, Thibodeau GA: Anatomy & physiology, ed 8, St Louis, 2013, Elsevier, p 1067.)
Oviducts
The two oviducts, also called the fallopian or uterine tubes, are each about 10 cm long and located in the upper margin of the broad ligament. Each oviduct runs laterally from the uterus to the uterine end of the ovary. The free end of the oviduct adjacent to the ovary is called the infundibulum. It is shaped like a funnel with long, fingerlike projections termed fimbriae. The ampulla, the longest part of the oviduct, has an inner lining consisting of ciliated mucous membrane arranged in longitudinal folds. Beneath this ciliated lining is a double layer of smooth muscle with a thick outer layer of peritoneal serosa. The oviduct has an active role in propelling the ovum toward the uterus; the current created by the beating cilia and the peristaltic contractions of the muscular wall are powerful forces that move ova along the oviduct. Once inside the oviduct, the ovum is moved through the ampulla to the isthmus (the short, narrow portion near the uterus) and finally through the intramural passageway to the uterus. Fertilization of the ovum occurs in the upper third of the oviduct, and the zygote (fertilized ovum) begins developing as it moves through the oviduct. If no fertilization occurs, the ovum undergoes degeneration in the oviduct.7
Uterus
The uterus varies in size, shape, location, and structure during various phases of a woman’s life and reproductive status. In the nonpregnant state, the uterus is about 8 cm long, 4 cm wide in its upper part, and 2 cm thick. The rounded part of the uterus, which lies above and in front of the openings of the oviducts, is called the fundus; the main portion of the uterus is the corpus, or body. The lower, narrow portion of the uterus is the cervix, which extends downward to the opening within the vagina. The cervix contains a narrow canal that joins the uterine cavity at the internal os and opens into the vagina at the external os.
The wall of the body and fundus of the uterus consists of three layers: endometrium, myometrium, and serosa (Figure 32-4). The outermost layer of the uterus, the serosa, consists of a single layer of mesothelial cells supported by a thin layer of loose connective tissue. The middle layer, the myometrium, consists of three layers of smooth muscle with the muscle fibers arranged in a different direction in each layer. The innermost lining of the uterus, the endometrium, consists of two layers: a thin deep layer called the basilar layer and a thick superficial layer referred to as the functional layer. During a woman’s reproductive years, the endometrium displays a constant cyclic activity of alternate proliferation and sloughing of the functional layer in response to estrogen and progesterone secretion.8 These changes will be discussed in more detail in the Menstrual Cycle section.
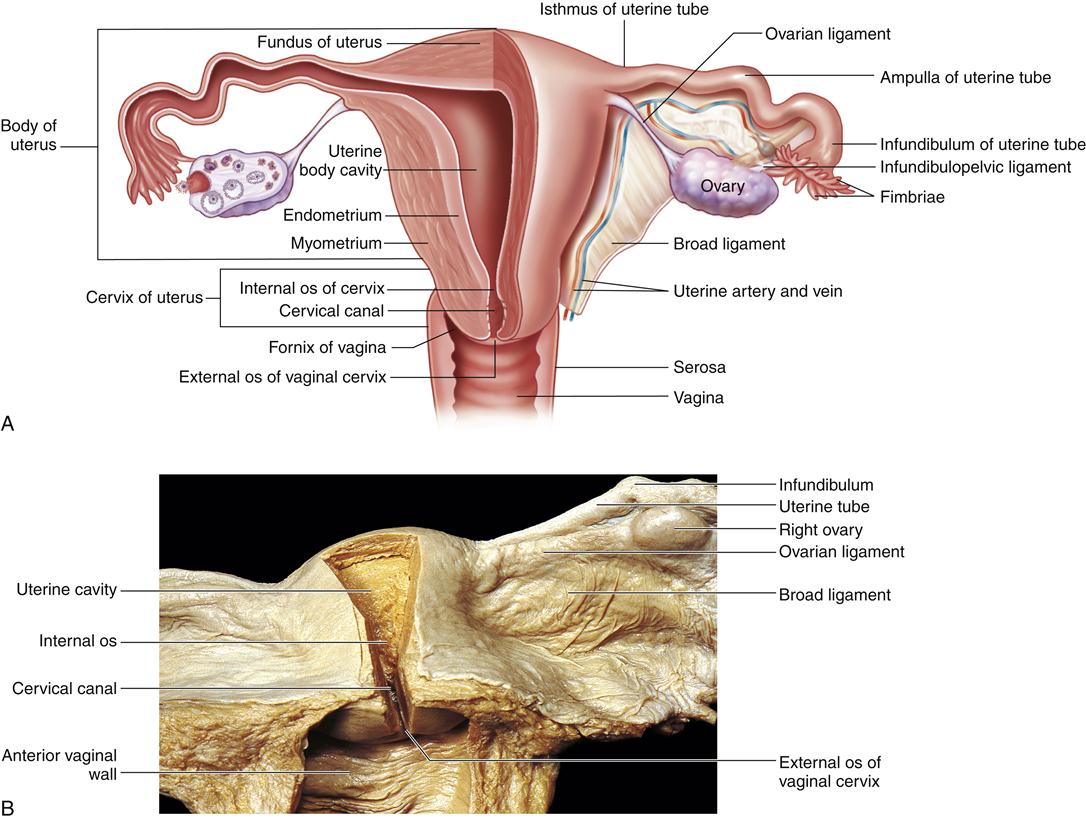
A, Diagram shows left side of uterus and upper portion of the vagina and the left uterine tube and ovary in a frontal section. The broad ligament has been removed from the posterior surface of the uterus and adjacent structures. B, Cadaver dissection showing uterine cavity and cervical canal, exposed by removal of parts of their posterior walls. Note that the uterine wall consists of an epithelial lining from which uterine glands extend through the full thickness of the mucosa. Beneath the endometrium, a portion of myometrium is shown. (A, From Patton KT, Thibodeau GA: Anatomy & physiology, ed 8, St Louis, 2013, Elsevier, p 1066. B, From Gosling J et al: Human anatomy, ed 4, Philadelphia, 2005, Mosby.)
Vagina
The vagina is the sexual organ that enfolds the penis during sexual intercourse, serves as an exit for discarded endometrium, and forms the lower end of the birth canal. It is located anterior to the rectum and posterior to the urethra and urinary bladder. The vagina surrounds the cervix at one end and opens to the vestibule at its other end. The vagina is a highly elastic muscle that is capable of considerable distention. Two longitudinal ridges run along the anterior and posterior walls, with numerous transverse folds called rugae. The vagina is lined by a mucous membrane of stratified squamous epithelium overlying a layer of connective tissue.7 The vaginal wall is subject to thinning with aging; this and other age-related changes in the female sexual organs are described in the Menopause section.
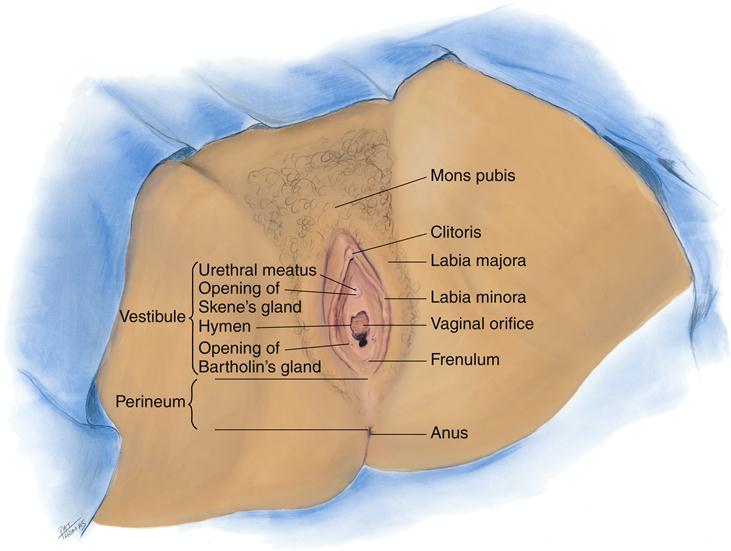
External Genitalia
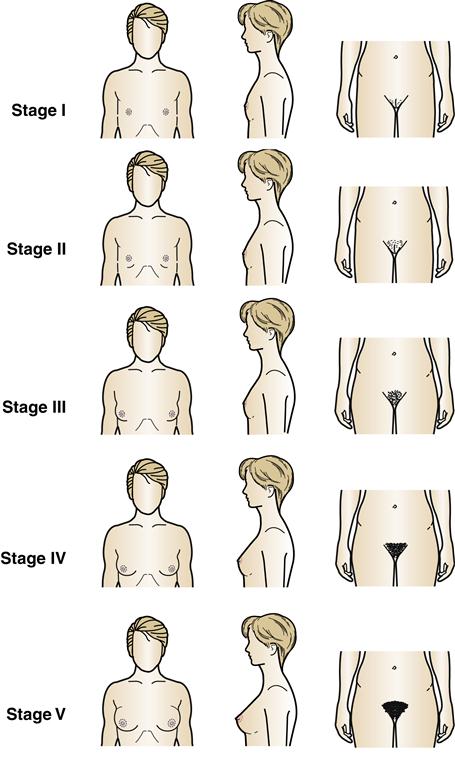
The external female genital structures include the mons pubis, labia majora, labia minora, clitoris, and vestibule of the vagina (Figure 32-5). The stages of development of the female external genitalia are depicted in Figure 32-6. The mons pubis is a rounded elevation in front of the pubis symphysis. It consists primarily of an accumulation of fat. After puberty, the skin over it is covered by coarse hair. The labia majora, which are homologous (i.e., corresponding in structure) with the scrotum of the male, are folds of skin that run downward and backward from the mons pubis to the area behind the vaginal opening. After puberty, the labia majora become pigmented and covered with hair. The labia minora are two small folds of skin located between the labia majora on either side of the vaginal opening. The vestibule of the vagina is the cleft between the labia minora and contains the openings of the vagina, the urethra, and the ducts of the greater vestibular glands (also called Bartholin glands). These glands, along with the lesser vestibular or Skene glands, secrete mucus to provide lubrication during sexual intercourse.7
The clitoris is a body of erectile tissue that projects from the anterior end of the vulva at the anterior junction of the labia minora. It is about 2 cm long and 0.5 cm in diameter and is covered by a fold of tissue called the prepuce, which is formed by the merging of labial tissue. The glans of the clitoris is the rounded elevation on the free end of the body and is highly sensitive to stimulation. During sexual arousal, the erectile tissue of the clitoris becomes engorged with blood.7,8
Menstrual Cycle
From menarche onward, the normal reproductive years of the female are characterized by rhythmic changes in hormonal secretion and corresponding changes in the sexual organs, which are called the target organs of the female hormones. This rhythmic pattern is called the menstrual cycle (Figure 32-7). Two significant results of the menstrual cycle are stimulation of the production of an ovum and preparation of the uterine endometrium for the implantation of a fertilized ovum at the appropriate phase of the cycle.8
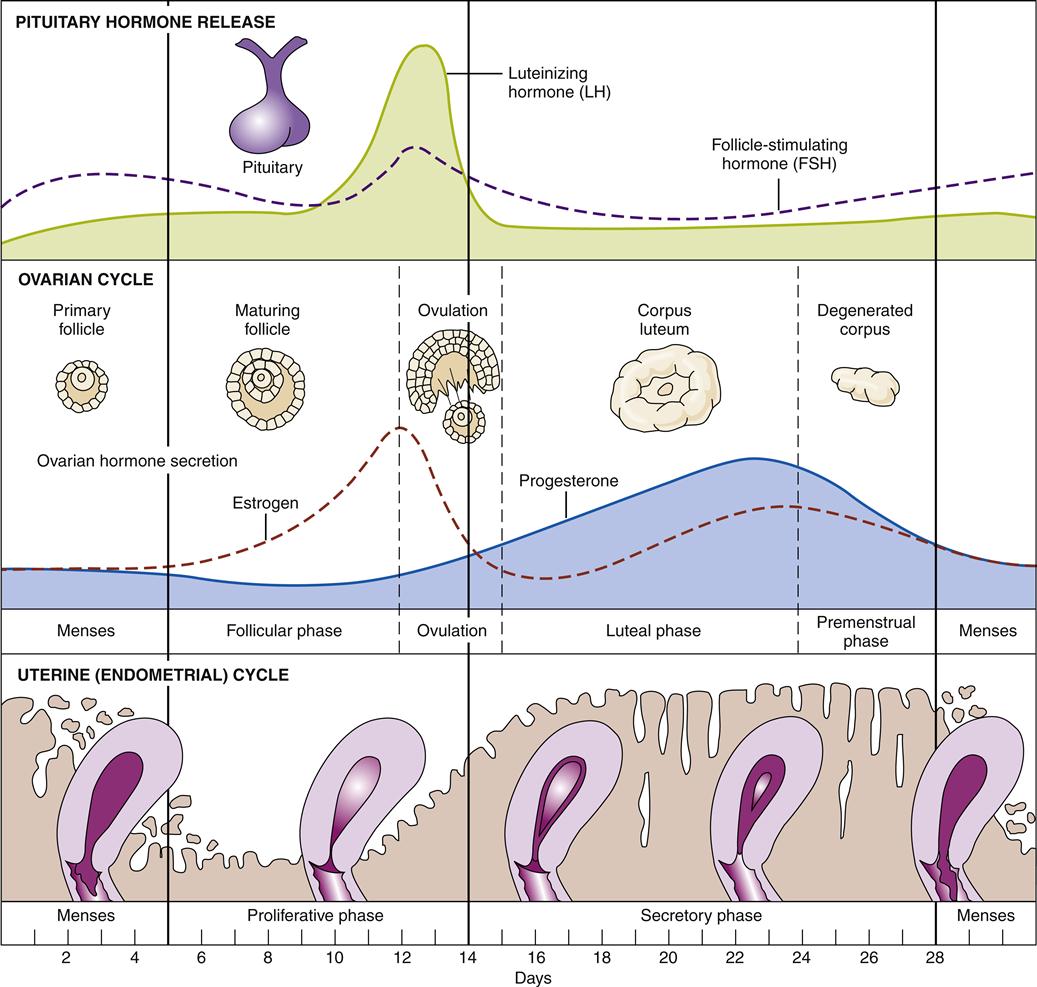
The events that take place within the pituitary, ovary, and uterus are precisely synchronized. When fertilization does not occur, the cycle repeats itself about every 28 days.
Although considerable variation can be found in human females, an average menstrual cycle is 28 days long, with cycles as short as 20 days or as long as 45 days occurring in normal women. The first day of menstruation is considered the first day of the menstrual cycle. Ovulation occurs approximately 14 days before the next cycle begins; thus in a 28-day cycle, ovulation occurs on about day 14 of the cycle.
The release of hormones and the accompanying response of the female sexual target organs are depicted in Figure 32-7. The principal female reproductive hormones are summarized in Table 32-1. As shown in Figure 32-7, the events of the menstrual cycle require precise synchronization between the activities of the pituitary gland, ovary, and uterus. Beginning at the first day of the menstrual cycle, or the first day of menstruation, these events can be summarized as follows. The thickened functional layer of the endometrium of the uterus is gradually sloughed off, and about 35 ml of blood is lost. During this phase of the menstrual cycle, follicle-stimulating hormone (FSH) is released by the pituitary gland and stimulates a group of follicles to develop in the ovary.
TABLE 32-1
PRINCIPAL FEMALE REPRODUCTIVE HORMONES
| HORMONE | TARGET ORGANS | SIGNIFICANT ACTIONS |
| Estrogen | Multiple sites throughout body, including reproductive structures, bone, fat, and muscle tissues | Development of reproductive organs during puberty Development of secondary sex characteristics, including breast maturation, widening of pelvis, and distribution of fat and muscle tissues in a distinctively female pattern Cyclic preparation of endometrium for implantation of an ovum |
| Progesterone | Primarily uterus and breasts | Cyclic preparation and maintenance of endometrium for implantation of an ovum Stimulation of development of breast lobes and alveoli |
| Follicle-stimulating hormone | Ovary | Stimulates ovarian follicle development; with luteinizing hormone, stimulates secretion of estrogen and ovulation |
| Luteinizing hormone | Ovary | Stimulates final development of ovarian follicle, process of ovulation, and development of corpus luteum |
In the preovulatory phase, also called the proliferative phase, theca and granulosa cells in the developing follicles in the ovary secrete estrogen, which stimulates growth of the uterine endometrium once again. At about the midpoint of the cycle, an increase in estrogen secretion from the follicles occurs. This increase in estrogen level is thought to render the anterior pituitary more responsive to luteinizing hormone–releasing hormone secreted by the hypothalamus.9 The anterior pituitary gland then produces a burst of luteinizing hormone (LH). The FSH level also increases about twofold at the same time, and these two hormones act synergistically to cause the extremely rapid swelling of the follicle that culminates in ovulation.10 During the process of ovulation, the secondary oocyte is ejected through the wall of the ovary into the peritoneal cavity. The free end of the oviduct is strategically located so that the ovum enters its fimbriated end almost immediately.7
After ovulation, the postovulatory phase (also called the luteal phase) begins. During the luteal phase the site of the ruptured follicle becomes a corpus luteum (Latin for “yellow body”), which secretes estrogen and progesterone. These hormones stimulate continued thickening of the uterine endometrium. The cells of the corpus luteum become greatly enlarged and develop lipid, or fatty, areas that give the cells a distinctive yellow color. In a normal cycle, the corpus luteum grows to approximately 1.5 cm, with maximal development attained about 7 to 8 days after ovulation. If pregnancy does not occur, the corpus luteum begins to degenerate, and progesterone and estrogen levels in the blood fall markedly. Constriction of the spiral arteries located in the uterine wall occurs, and the portion of the endometrium supplied by these arteries becomes ischemic. As the cells in the endometrium die, tissue is sloughed off and menstruation begins again. It is presently thought that prostaglandins liberated in the endometrium may have a role in stimulating the sloughing of endometrial tissue.7,11
If fertilization of the ovum occurs, the embryo arrives in the uterus on about the fourth day of development. Small glands in the endometrium stimulated by progesterone produce a nutritive fluid for the developing embryo. On approximately the seventh day after fertilization, the embryo implants itself in the thick endometrium of the uterus, and development of the placenta occurs. The placenta secretes the hormone human chorionic gonadotropin (hCG), which in turn signals the corpus luteum to continue to function. Subsequent events in pregnancy are described later in this chapter.