Chapter 32 Ethanol, Other Alcohols, and Drugs for Alcohol Dependence
| Abbreviations | |
|---|---|
| ADH | Alcohol dehydrogenase |
| ALDH | Aldehyde dehydrogenase |
| BAC | Blood alcohol concentration |
| CNS | Central nervous system |
| GABA | γ-Aminobutyric acid |
| GI | Gastrointestinal |
| 5-HT | Serotonin |
| NAD+ | Nicotinamide adenine dinucleotide |
| NADH | Nicotinamide adenine dinucleotide, reduced |
| NADD+ | Nicotinamide adenine dinucleotide phosphate |
| NADPH | Nicotinamide adenine dinucleotide phosphate, reduced |
| NE | Norepinephrine |
| NMDA | N-methyl-D-aspartate |
| TNF | Tumor necrosis factor |
| VTA | Ventral tegmental area |
Therapeutic Overview
| Therapeutic Overview |
|---|
| Ethanol is used: |
| Topically to reduce body temperature and as an antiseptic |
| By injection to produce irreversible nerve block by protein denaturation |
| By inhalation to reduce foaming in pulmonary edema |
| In treatment of methanol and ethylene glycol poisoning |
| Ethanol dependence may be treated with psychosocial/behavioral therapy and an: |
| Aldehyde dehydrogenase inhibitor (Disulfiram) |
| Glutamate receptor antagonist (Acamprosate) |
| Opioid receptor antagonist (Naltrexone) |
Mechanisms of Action
Studies suggest that the effects of ethanol may be attributed to its direct binding to lipophilic areas either near or in ion channels and receptors. The ion channels influenced by ethanol are listed in Table 32-1. Ethanol may have either inhibitory or facilitatory effects, depending on the channel, but its resultant action is CNS depression. Because the barbiturates and benzodiazepines exhibit cross-tolerance to ethanol, and their CNS depressant effects are additive with those of ethanol, they may share a common mechanism, perhaps through the γ-aminobutyric acid (GABA) type A receptor (see Chapter 31). Ethanol may also exert some of its effects by actions at glutamate N-methyl-D-aspartate (NMDA) receptors or serotonin (5-HT) receptors.
TABLE 32–1 Ion Channels Affected by Ethanol
| Channel | Effects | Ethanol Concentration (mM) |
|---|---|---|
| Na+ (voltage-gated) | Inhibition | 100 and higher* |
| K+ (voltage-gated) | Facilitation | 50-100 |
| Ca++ (voltage-gated) | Inhibition | 50 and higher |
| Ca++ (glutamate receptor-activated) | Inhibition | 20-50 |
| Cl− (GABAA receptor-gated) | Facilitation | 10-50 |
| Cl− (glycine receptor-gated) | Facilitation | 10-50 |
| Na+/K+ (5HT3 receptor-gated) | Facilitation | 10-50 |
* 100 mM ethanol is 460 mg/dL.
The reinforcing actions of ethanol are complex but are mediated in part through its ability to stimulate the dopaminergic reward pathway in the brain (see Fig. 27-8). Evidence has indicated that ethanol increases the synthesis and release of the endogenous opioid β-endorphin in both the ventral tegmental area (VTA) and the nucleus accumbens. Increased β-endorphin release in the VTA dampens the inhibitory influence of GABA on the tonic firing of VTA dopaminergic neurons, whereas increased β-endorphin release in the nucleus accumbens stimulates dopaminergic nerve terminals to release neurotransmitter. Both of these actions to increase dopamine release may be involved in the rewarding effects of ethanol.
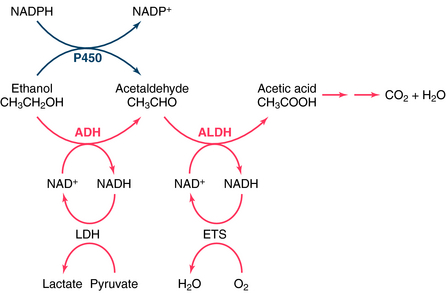
Aldehyde Dehydrogenase Inhibitor
Disulfiram, used for the treatment of alcoholism since the 1940s, is an inhibitor of the enzyme aldehyde dehydrogenase (ALDH), a major enzyme involved in the metabolism of ethanol (Fig. 32-1). Inhibiting the catabolism of acetaldehyde produced by the oxidation of ethanol, leads to the accumulation of acetaldehyde in the plasma, resulting in aversive effects.
Naltrexone is an opioid receptor antagonist at both κ and μ opioid receptors (see Chapter 36). Its ability to inhibit alcohol consumption has been attributed to blockade of μ receptors in both the VTA and nucleus accumbens, thereby decreasing the ethanol-induced activation of the dopamine reward pathway.
Pharmacokinetics
Alcohol taken orally is absorbed throughout the gastrointestinal (GI) tract. Absorption depends on passive diffusion and is governed by the concentration gradient and the mucosal surface area. Food in the stomach will dilute the alcohol and delay gastric emptying time, thereby retarding absorption from the small intestine (where absorption is favored because of the large surface area). High ethanol concentrations in the GI tract cause a greater concentration gradient and therefore hasten absorption. Absorption continues until the alcohol concentration in the blood and GI tract are at equilibrium. Because ethanol is rapidly metabolized and removed from the blood, eventually all the alcohol is absorbed.
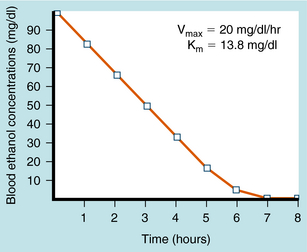
Ethanol undergoes significant first-pass metabolism. Most (>90%) of the ethanol ingested is metabolized in the liver, with the remainder excreted through the lungs and in urine. Alcohol dehydrogenase (ADH) catalyzes the oxidation of ethanol to acetaldehyde, which is oxidized further by ALDH to acetate (see Fig. 32-1). Acetate is oxidized primarily in peripheral tissues to CO2 and H2O. Both ADH and ALDH require the reduction of nicotinamide adenine dinucleotide (NAD+), with 1 mol of ethanol producing 2 mol of reduced NAD+ (NADH). The NADH is reoxidized to NAD+ by conversion of pyruvate to lactate by lactate dehydrogenase (LDH) and the mitochondrial electron transport system (ETS). During ethanol oxidation the concentration of NADH can rise substantially, and NADH product inhibition can become rate-limiting. Similarly, with large amounts of ethanol, NAD+ may become depleted, limiting further oxidation through this pathway. At typical blood alcohol concentrations (BACs), the metabolism of ethanol exhibits zero-order kinetics; that is, it is independent of concentration and occurs at a relatively constant rate (Fig. 32-2). Fasting decreases liver ADH activity, decreasing ethanol metabolism.
Ethanol may also be metabolized to acetaldehyde in the liver by cytochrome P450, a reaction that requires 1 mol of reduced nicotinamide adenine dinucleotide phosphate (NADPH) for every ethanol molecule (see Fig. 32-1). Although P450-mediated oxidation does not normally play a significant role, it is important with high concentrations of ethanol (≥100 mg/dL), which saturate ADH and deplete NAD+. Because this enzyme system also metabolizes other compounds, ethanol may alter the metabolism of many other drugs. In addition, this system may be inhibited or induced (Chapter 2), and induction by ethanol may contribute to the oxidative stress of chronic alcohol consumption by releasing reactive O2 species during metabolism.
Significant genetic differences exist for both ADH and ALDH that affect the rate of ethanol metabolism. Several forms of ADH exist in human liver, with differing affinities for ethanol. Whites, Asians, and African-Americans express different relative percentages of the genes and their respective alleles that encode subunits of ADH, contributing to ethnic differences in the rate of ethanol metabolism. Similarly, there are genetic differences in ALDH. Approximately 50% of Asians have an inactive ALDH, caused by a single base change in the gene that renders them incapable of oxidizing acetaldehyde efficiently, especially if they are homozygous. When these individuals consume ethanol, high concentrations of acetaldehyde are achieved, leading to flushing and other unpleasant effects. People with this condition rarely become alcoholic. As discussed, the unpleasant effects of acetaldehyde accumulation form the basis for the aversive treatment of chronic alcoholism with disulfiram. The pharmacokinetics of ethanol are summarized in Table 32-2.
TABLE 32–2 Pharmacokinetic Considerations of Ethanol
| Pharmacokinetic Parameter | Considerations |
|---|---|
| Route of administration | Topically, orally, inhalation, by injection into nerve trunks, or intravenously for poison management |
| Absorption | |
| Distribution | Total body H2O; volume of distribution is 68% of body weight in men and 55% in women; varies widely |
| Metabolism | |
| Elimination | Excreted in expired air, urine, milk, sweat |