Epithelial Hyperplasia
Key Facts
Terminology
Usual type ductal epithelial hyperplasia (UDH)
Clinical Issues
UDH found in up to 25% of breast biopsies
UDH is frequent constituent of benign epithelial changes
Florid UDH associated with 1.5-2x increased relative risk of developing subsequent carcinoma
Microscopic Pathology
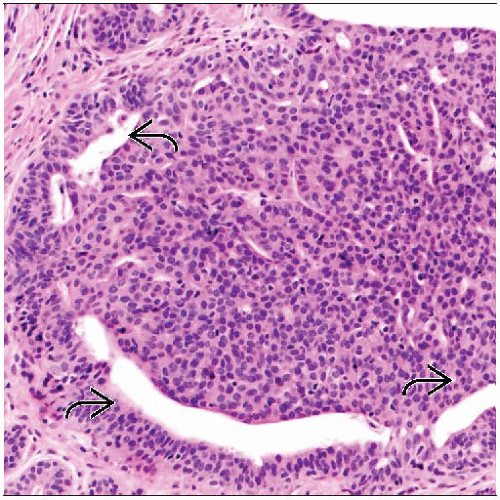
Solid pattern
Heterogeneity in cell size, shape, and placement
Haphazard arrangement of cells
Fenestrated pattern
Luminal spaces irregular and variable in size and shape (slit-like)
Peripherally located luminal spaces
Cellular proliferation may have syncytial appearance
Individual cell borders are inconspicuous
Cellular proliferation has benign cytologic features
Some cases may show spindle-shaped cells with prominent streaming or swirling pattern
Ancillary Tests
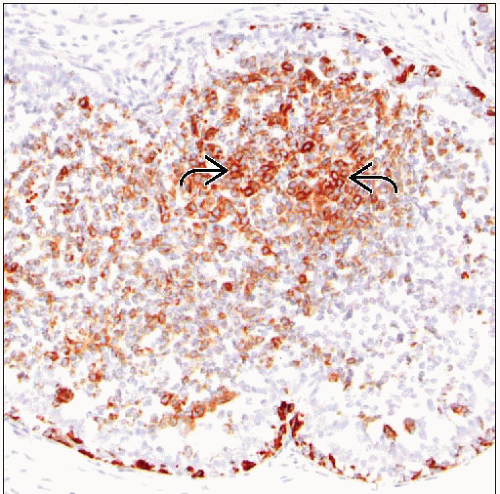
UDH shows diffuse or mosaic pattern of staining with high molecular weight cytokeratin
Cells of UDH show variable expression of ER and PR
Stains for CK5/6 or 34BE12 may be helpful for distinguishing UDH from ADH
Top Differential Diagnoses
Atypical ductal hyperplasia
Low-grade ductal carcinoma in situ
TERMINOLOGY
Abbreviations
Usual type ductal epithelial hyperplasia (UDH)
Synonyms
Ductal epithelial hyperplasia
Definitions
UDH: Benign intraductal epithelial proliferation
Proliferation tends to fill and bridge across involved spaces
Considerable variability in degree of proliferation
Mild proliferation: 2-4 cell layers
Florid proliferation: > 4 cell layers filling and distending duct spaces
Florid UDH may show solid, fenestrated, or micropapillary-type architecture
Florid UDH must be distinguished from atypical ductal epithelial hyperplasia (ADH) and low-grade ductal carcinoma in situ (LGDCIS)
ETIOLOGY/PATHOGENESIS
Molecular Changes in UDH
Molecular studies have shown loss of heterozygosity in subsets of UDH
No consistent molecular alterations have been reported
Fewer genetic abnormalities compared with ADH, LGDCIS, and invasive cancer from same patients
Molecular data support the concept that UDH does not represent a direct cancer precursor
Current concept: Moderate to florid UDH is a marker of generalized increased cancer risk
CLINICAL ISSUES
Epidemiology
Incidence
UDH can be found in up to 25% of benign breast biopsies
Age
Majority of women with UDH are 35-60 years of age
UDH is less frequent in patients > 60 years of age
Presentation
Microscopic finding and is not clinically apparent
UDH is frequent constituent of benign epithelial changes
Can include any of the following
Apocrine cysts
Sclerosing adenosis
Papillary apocrine metaplasia
Stromal hyperplasia and fibrosis
Benign epithelial changes may present as indeterminate mammographic calcifications
Calcifications are usually associated with cysts or sclerosing adenosis
UDH is not typically associated with calcifications
These changes may also present as palpable abnormality
Most often, mass is ill-defined palpable area of breast thickening
Treatment
UDH is benign process requiring no further treatment
Patients should be encouraged to participate in regular clinical follow-up
Prognosis
UDH is associated with a 1.5-2x increased relative risk of developing subsequent carcinoma
This means that 5-7% of women with UDH are expected to develop breast cancer during their lifetimes
Subsequent risk is higher with diagnosis of ADH (5x increase in relative risk)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree