Encapsulated Papillary Carcinoma
Key Facts
Terminology
Papillary carcinoma present within single well-circumscribed cystic space
Synonyms: Encysted papillary carcinoma, intracystic carcinoma
Clinical Issues
0.5-2% of breast cancers in women
Most common in elderly women (median age: 70)
Often presents as palpable mass or circumscribed mammographic density
Some women present with nipple discharge
Survival is > 95% at 10 years
Although absence of myoepithelial cells is more compatible with classification as invasive carcinoma, clinical behavior is more similar to DCIS
Ancillary Tests
Estrogen and progesterone receptors are positive in almost all cases
HER2 is absent
Myoepithelial markers will confirm absence of myoepithelial cells in papillary fronds and in surrounding capsule
p63 is most useful marker for detecting myoepithelial cells in papillary fronds
Collagen type IV is present around periphery of lesion
Top Differential Diagnoses
Ductal carcinoma in situ, papillary type
Solid papillary carcinoma
Large duct papilloma
 Encapsulated papillary carcinoma occurs as a well-circumscribed mass, usually located in the central breast below the nipple. Many cases are associated with nipple discharge. |
TERMINOLOGY
Abbreviations
Encapsulated papillary carcinoma (EPC)
Synonyms
Intracystic papillary carcinoma
Encysted papillary carcinoma
Definitions
Papillary carcinoma present within single well-circumscribed cystic space
CLINICAL ISSUES
Epidemiology
Incidence
0.5-2% of breast cancers in women
Rare in men but more common than invasive ductal carcinoma or DCIS
Age
Most common in elderly women (median: 70 years)
Presentation
Often presents as palpable mass or circumscribed mammographic density
Location is usually central below nipple
Usually deeper in breast than large duct papillomas
Some women present with nipple discharge
Natural History
EPC was originally classified as DCIS
Lymph node metastases are rare
Macrometastases have been reported in rare cases; associated carcinomas are often exceptionally large
Cases of isolated tumor cells in nodes may be related to epithelial displacement by prior core needle biopsy
Survival is > 95% at 10 years
Although absence of myoepithelial cells is more compatible with classification as invasive carcinoma, clinical behavior is more similar to DCIS
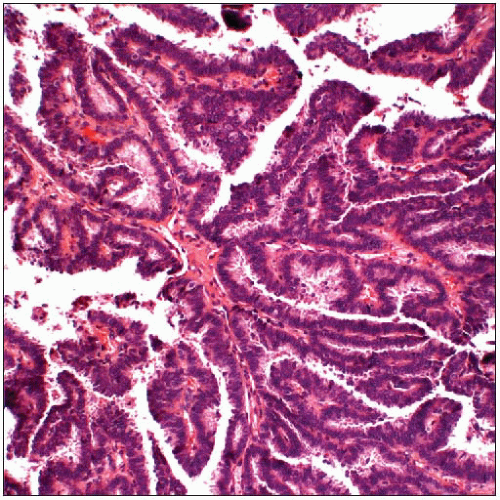
MICROSCOPIC PATHOLOGY
Histologic Features
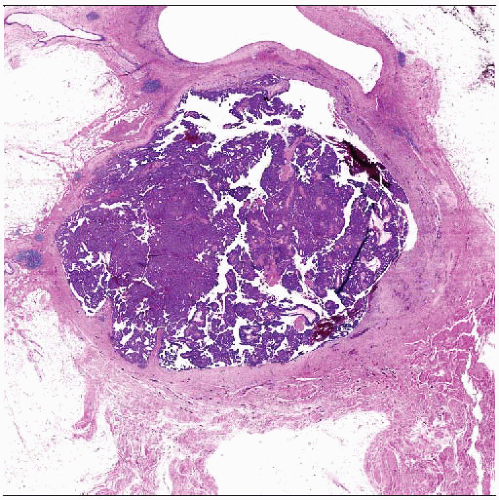
Carcinoma is confined to well-circumscribed space
Outer capsule is generally fibrotic with scattering of lymphocytes
Entrapment of epithelium within capsule may occur
Delicate thin papillary fronds with thin fibrovascular core
Fronds are lined by single layer of monotonous-appearing columnar cells
Occasional globoid cells may be present
More abundant pale cytoplasm and rounded in shape
Often positive for GCDFP-15
Should not be misinterpreted as myoepithelial cells
Approximately 25% of cases are associated with areas of frank stromal invasion
Invasive carcinoma extends beyond fibrous capsule of lesion
Carcinoma is generally of no special type and is not papillary in appearance
ANCILLARY TESTS
Immunohistochemistry
Estrogen and progesterone receptors are positive in almost all cases
HER2 is absent
Myoepithelial markers will confirm absence of myoepithelial cells in papillary fronds and in surrounding capsule
p63 is most useful marker for detecting myoepithelial cells in papillary fronds
Endothelial cells often lie close to tumor cells and will also be positive for muscle markers (e.g., smooth muscle actin, calponin)
Collagen type IV is present around periphery of lesion
DIFFERENTIAL DIAGNOSIS
Ductal Carcinoma In Situ, Papillary Type
Usually involves multiple ductal spaces
Myoepithelial cells will be present around periphery of involved ducts
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree