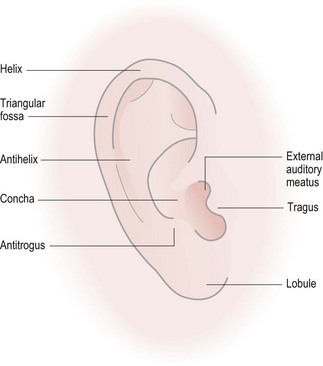
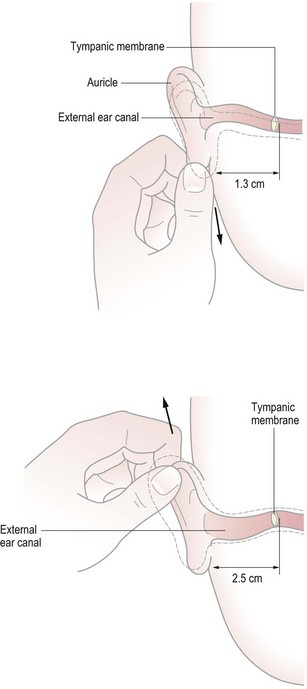
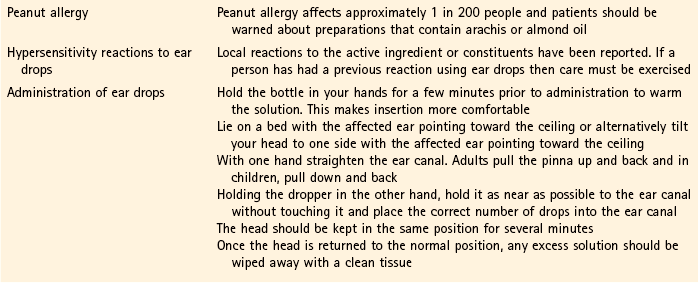
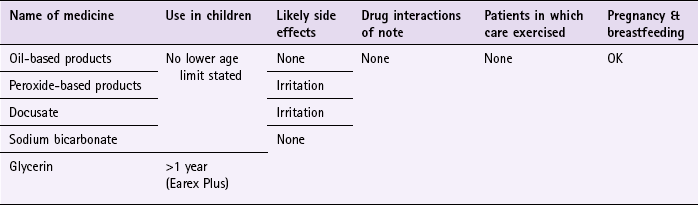
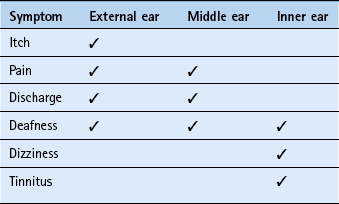
Chapter 3 Background The external ear consists of the pinna (Fig. 3.1) and the external auditory meatus (EAM, ear canal). Their function is to collect and transmit sound to the tympanic membrane (eardrum). A thorough and accurate history coupled with a physical examination of the outer ear should be undertaken, as certain symptoms can help decide what structure of the ear the problem originates from (Table 3.1) and its likely cause (Table 3.2). Table 3.1 Ear symptoms and the affected ear structures Adapted from C Acomb, Pharmaceutical Journal, August 1991. Table 3.2 Possible causes of the presenting complaint 2. Next inspect the external ear for redness, swelling and discharge. 3. Then apply pressure to the mastoid area which is directly behind the pinna (If the area is tender this suggests mastoiditis, a rare complication of otitis media). 4. Next move the pinna up and down and manipulate the tragus. If either is tender on movement then this suggests external ear involvement. 5. You should finally examine the EAM. This is best performed using an otoscope, however currently most pharmacists have not had appropriate training in their use. An alternative way to inspect the EAM would be to use a pen torch. Because of the shape of the EAM, when performing an examination the pinna needs to be manipulated to obtain the best view of the ear canal (Fig. 3.2). Ear wax is by far the commonest external ear problem that pharmacists encounter and is the most common ear problem in the general population. Careful questioning along with inspection of the EAM should mean that wax impaction is readily distinguished from other conditions (Table 3.3). Specific questions to ask the patient: Ear wax Cerumenolytics have been used for many years to help soften, dislodge and remove impacted ear wax. Two systematic reviews have been published (Burton & Doree 2009; Hand & Harvey 2004) to determine if pharmacological intervention is effective in wax removal. Each had slightly different inclusion criteria resulting in some trials being included in both but also some trials reviewed in only one of the reviews. All trials reviewed had aspects of poor methodological quality (e.g. lack of clear randomisation and blinding and potential for publication bias as some were company sponsored trials) and were of relatively small size. The findings from these reviews support the use of oil-based softeners, sodium bicarbonate and sterile water over no treatment at all, but no active treatment proved more superior over any other. Further trials between oil-based products and saline reported oil-based products to be significantly better than saline but again showed no differences between each other. Prescribing information relating to ear wax medicines reviewed in the section ‘Evidence base for over-the-counter medication’ is discussed and summarised in Table 3.4 and useful tips relating to patients presenting with ear wax are given in Hints and Tips Box 3.1. Cerumol Ear Drops (Arachis – peanut oil, 57.3%): The standard dose for adults and children is five drops into the affected ear two or three times a day repeated for up to 3 days. In between administration a plug of cotton wool moistened with Cerumol or smeared with petroleum jelly should then be applied to retain the liquid. Cerumol Olive Oil Drops (olive oil 100%): For adults and children, two to three drops should be instilled twice a day for up to 7 days. Like Cerumol, a cotton wool plug should be gently placed in the ear to retain the liquid. Peroxide-based products (Exterol & Otex range): For adults and children, five drops should be instilled once or twice daily for at least 3 to 4 days. Unlike Cerumol, the patient should be advised not to plug the ear but retain the drops in ear for several minutes by keeping the head tilted and then wipe away any surplus. Patients might experience mild, temporary effervescence in the ear as the urea hydrogen peroxide complex liberates oxygen.
Ear conditions
General overview of ear anatomy
History taking and physical exam
Patient presents with
Possible causes
Redness and swelling
Perichondritis, haematoma
Discharge
Otitis externa or media. If discharge mucinous, originates from middle ear as EAM has no mucous glands
Pain in mastoid area
Otitis media, mastoiditis
Pain when pressing tragus or moving pinna
Otitis externa
Physical examination
Ear wax impaction
Arriving at a differential diagnosis
![]() Table 3.3
Table 3.3
Question
Relevance
Course of symptoms
The patient usually has a history of gradual hearing loss with ear wax impaction
Associated symptoms
Dizziness and tinnitus indicates an inner ear problem and should be referred. Ear wax impaction rarely causes tinnitus, vertigo or true pain
History of trauma
Check if the person has recently tried to clean the ears. This often leads to wax impaction
Use of medicines
If a patient has used an appropriate OTC medication correctly this would necessitate referral for further investigation and possibly ear-syringing
Evidence base for over-the-counter medication
Practical prescribing and product selection
Cerumenolytics
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree