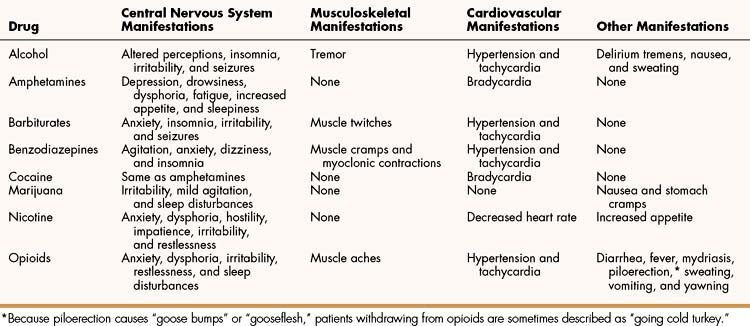
TABLE 25–2 Emergency Treatment of Drug Intoxication
| Drug | Pharmacologic Treatment | Nonpharmacologic Treatment |
|---|---|---|
| Alcohol | None | Support vital functions |
| Amphetamines | Lorazepam for agitation and haloperidol for psychosis | Monitor and support cardiac function |
| Barbiturates | None | Support vital functions |
| Benzodiazepines | Flumazenil | Support vital functions |
| Cocaine | Lorazepam for agitation or seizures | Support vital functions |
| Hallucinogens | Lorazepam for agitation | Give reassurance and support vital functions |
| Marijuana | Lorazepam for agitation | Give reassurance and support vital functions |
| Opioids | Naloxone | Support vital functions |
| Phencyclidine | Lorazepam for agitation and haloperidol for psychosis | Minimize sensory input |
CENTRAL NERVOUS SYSTEM DEPRESSANTS
Alcohols and Glycols
In North America, about 12 million individuals have one or more symptoms of alcoholism, making alcohol abuse the number one substance abuse problem. In the United States alone, the cost of health care, lost work hours, criminal activity, and other problems related to alcohol use is roughly $90 billion each year.
The alcohols and glycols most commonly ingested are ethanol, methanol, and ethylene glycol. Whereas ethanol selectively produces CNS depression at normal doses, even relatively small doses of methanol and ethylene glycol affect multiple organ systems and can produce severe or life-threatening toxicity, even when ingested in relatively small doses.
Ethanol
Ethanol, or ethyl alcohol, is classified as a CNS depressant and has pharmacologic effects similar to those of the barbiturates and benzodiazepines.
PHARMACOKINETICS
Ethanol has sufficient lipid solubility to enable rapid and almost complete absorption from the gut. It is more rapidly absorbed from the duodenum than from the stomach, and food slows its absorption by slowing the rate of gastric emptying. Ethanol is widely distributed throughout the body and has a volume of distribution that is roughly equivalent to the total body water, or about 38 L/70 kgof body weight.
As shown in Figure 25–1, ethanol is primarily oxidized by alcohol dehydrogenase to form acetaldehyde and is then oxidized by acetaldehyde dehydrogenase to form acetate. The acetate derived from ethanol enters the citric acid cycle for further oxidation to carbon dioxide and water. The oxidation of ethanol utilizes significant quantities of nicotinamide adenine dinucleotide (NAD), and the depletion of NAD is responsible for some of the metabolic effects of ethanol that are described below. Ethanol at higher or chronic doses also undergoes oxidation by cytochrome P450 enzymes, namely the CYP2E1 isozyme. Unlike alcohol dehydrogenase metabolism, CYP2E1 metabolism is induced by long-term alcohol use, contributing to alcohol tolerance in heavy drinkers.
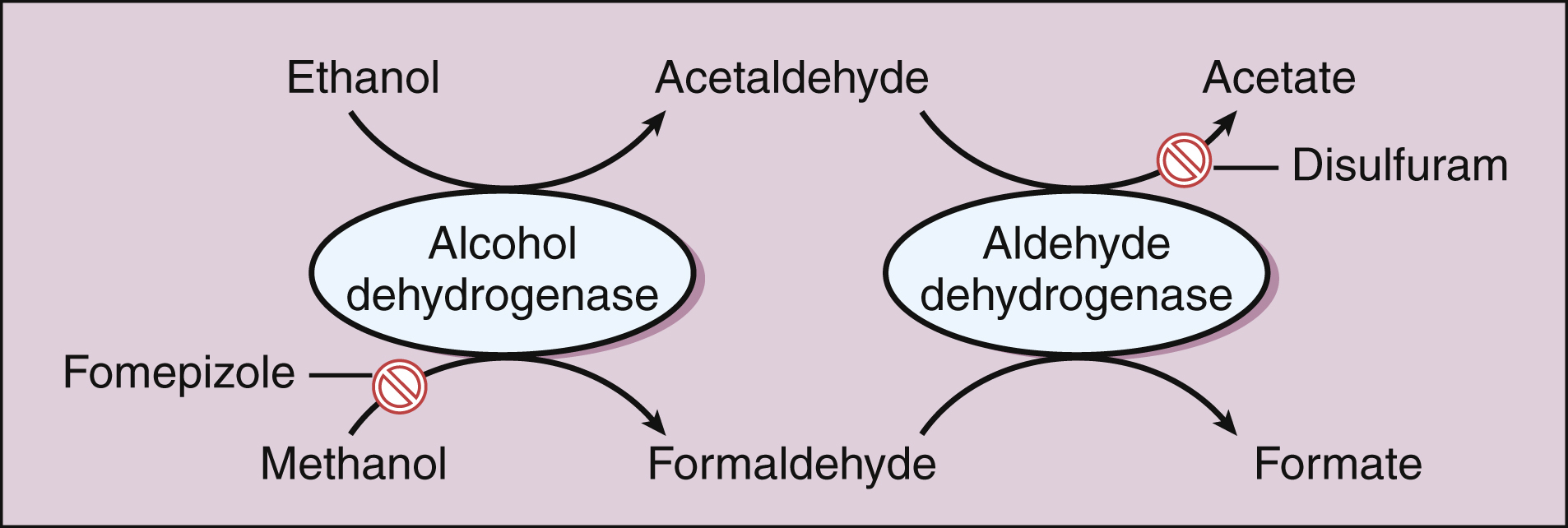
Figure 25–1 Metabolism of ethanol and methanol.
Alcohols are oxidized to aldehydes by alcohol dehydrogenase. The aldehydes are oxidized to acetate or formate by aldehyde dehydrogenase. Disulfiram inhibits aldehyde dehydrogenase and leads to the accumulation of acetaldehyde during ethanol ingestion. Fomepizole inhibits alcohol dehydrogenase and is used in methanol or ethylene glycol poisoning.
About 2% of ethanol is excreted unchanged by the kidneys and lungs. The concentration of ethanol in alveolar air is about 0.05% of that in the blood, and this relationship is used to estimate the blood alcohol concentration (BAC) in exhaled air when the breathalyzer test is administered. Because ethanol can markedly impair the psychomotor skills required to safely drive a vehicle, nearly all nations prohibit the operation of motor vehicles while under the influence of alcohol. As of July 2004, the legal limit of blood alcohol is a BAC less than 0.08% (80 mg/dL) in all states and federal territories of the United States.
The capacity of alcohol dehydrogenase to metabolize ethanol is limited because the enzyme is saturated at relatively low ethanol concentrations. Hence, ethanol metabolism exhibits zero-order kinetics, except when serum concentrations of ethanol are very low. For this reason, the BAC is largely determined by the rate of ethanol ingestion. An adult weighing 70 kg usually metabolizes only about 10 mL of absolute ethanol per hour, which is roughly equivalent to the amount of ethanol contained in one alcoholic drink. A BAC of 0.08% to 0.10% in most cases is reached after an adult consumes from two to four drinks (bottles of beer, glasses of wine, or 6 ounces of distilled liquor) within an hour.
CENTRAL NERVOUS SYSTEM EFFECTS, MECHANISMS, AND INTERACTIONS
Ethanol potentiates the actions of γ-aminobutyric acid (GABA) in a manner similar to that of benzodiazepines and barbiturates (see Chapter 19). It thereby produces sedative-hypnotic, anxiolytic, amnesic, and anticonvulsant effects. However, long-term ethanol use or ethanol withdrawal may lower the seizure threshold and thereby cause seizures. Predictably, ethanol potentiates the effects of benzodiazepines and barbiturates, so the combination of any of these drugs with ethanol can produce fatal CNS depression.
Ethanol at low doses produces disinhibition and mild euphoria, which facilitate social interactions by reducing behavioral inhibitions and self-consciousness. These reinforcing effects are correlated to the rise of the BAC, which probably determines the rate at which dopamine increases in the nucleus accumbens. In many individuals, reinforcement leads to the continued consumption of alcoholic beverages and to ethanol intoxication. This problem is exacerbated by the limited rate at which ethanol can be eliminated from the body.
Ethanol inhibits the release of acetylcholine from CNS neurons, and this action may contribute to the sedation and delirium that occur during alcohol intoxication. Ethanol also inhibits the release of antidiuretic hormone from the pituitary gland and thereby produces a diuretic effect. This diuretic effect is augmented by the consumption of large volumes of alcoholic beverages, such as a six-pack of beer.
Ethanol produces vasodilation and increases heat loss from the body, partly by interfering with temperature regulation by the hypothalamus. Hence, alcohol consumption can contribute to hypothermia during cold weather.
OTHER EFFECTS, MECHANISMS, AND INTERACTIONS
In addition to producing CNS effects, ethanol ingestion produces a variety of short-term and long-term cardiovascular and autonomic effects.
Blood pressure fluctuations are caused by the combination of peripheral vasodilation, depression of regulatory centers in the medulla, and the release of norepinephrine from sympathetic neurons. Consumption of large amounts of ethanol on a long-term basis can eventually lead to alcoholic cardiomyopathy and cardiac arrhythmias.
In alcoholic patients, thiamine deficiency secondary to a poor diet is commonly observed, which leads to nerve demyelination. This, in turn, causes peripheral neuropathies, characterized by paresthesias and reduced sensory acuity. Thiamine deficiency can also cause Wernicke-Korsakoff syndrome, a behavioral disorder characterized by confusion, severe anterograde and retrograde amnesia, ataxia, nystagmus, and ophthalmoplegia. The administration of thiamine substantially reverses all but the amnesic effects seen in patients with this syndrome.
Alcoholic patients can also develop several metabolic disorders. The depletion of NAD causes several citric acid cycle metabolites and lactate to accumulate and eventually contributes to liver degeneration (cirrhosis) and impaired glycogenolysis. The resulting hypoglycemia exacerbates the effects of ethanol on the CNS. A dietary deficiency of folate can lead to megaloblastic anemia, whereas a deficiency of other vitamins and antioxidants contributes to the overall tissue damage observed in alcoholism.
The consumption of significant quantities of ethanol during pregnancy is responsible for the occurrence of the fetal alcohol syndrome, which is characterized by low birth weight, microcephaly, facial abnormalities (flattening), mental retardation, heart defects, and other abnormalities.
Other Alcohols and Glycols
Methanol, also called methyl alcohol or wood alcohol, is a highly toxic form of alcohol that can cause profound anion gap metabolic acidosis and severe damage to the eyes. As shown in Figure 25–1, methanol is converted to formaldehyde and then to formate. Formate is primarily responsible for optic nerve damage, which can result in visual field impairment or permanent blindness. In cases of methanol poisoning, patients are treated with ethanol, which serves to saturate alcohol dehydrogenase and thereby prevent the formation of formaldehyde and formate. Ethanol has a greater affinity for alcohol dehydrogenase than does methanol. Hemodialysis is also used to reduce methanol levels in severe intoxication. Fomepizole, an inhibitor of alcohol dehydrogenase can also be administered, which prevents the formation of toxic metabolites in cases of methanol and ethylene glycol poisoning.
Isopropyl alcohol, which is contained in many formulations of rubbing alcohol, produces more CNS depression than does ethanol or methanol. Isopropyl alcohol is converted to acetone, a substance that can be smelled on the breath. The treatment of intoxication is largely supportive.
Ethylene glycol is contained in automobile antifreeze and de-icing fluids, and its ingestion can cause anion gap metabolic acidosis and serious toxicity to the kidneys, lungs, and CNS. Due to its sweet taste and appealing color, children often succumb to ethylene glycol poisoning from automobile antifreeze left accessible in the garage. Ethylene glycol is metabolized to oxalic acid, and calcium oxalate crystals may be found in the urine of patients after ethylene glycol ingestion. Treatment consists of supporting vital functions, giving ethanol or fomepizole, managing acidosis, and performing hemodialysis.
Barbiturates and Benzodiazepines
The pharmacologic properties of barbiturates and benzodiazepines are discussed in Chapter 19. These drugs are sedative-hypnotic agents that are prescribed for the treatment of anxiety disorders, insomnia, and other conditions. They are used recreationally for their euphoric and anxiolytic effects, and some polydrug users use them to reduce the irritability and anxiety associated with cocaine or amphetamine use.
The short-acting barbiturates (e.g., pentobarbital) are among the most widely abused sedative-hypnotic drugs. Several benzodiazepines have also been used illicitly, including flunitrazepam. Although this drug is not approved for use in the United States, it is used throughout much of the world as an anxiolytic or hypnotic drug. In the United States, it is widely available from street dealers and is sometimes referred to as roofies, derived from its trade name, Rohypnol. Flunitrazepam has gained notoriety as a party drug, a club drug, and a drug that contributes to date rape. It is an extremely potent benzodiazepine that is tasteless when dissolved in a beverage. Flunitrazepam produces drowsiness, impaired motor skills, and anterograde amnesia. Hence, victims do not recall events that happened the night before.
The long-term use of barbiturate or benzodiazepine drugs can lead to psychological and physical dependence, and their abrupt withdrawal produces symptoms that are similar to those caused by alcohol withdrawal (see Table 25–3).
Gamma hydroxybutyrate (GHB) usually comes as an odorless liquid, slightly salty to the taste, and is sold in small bottles. It has also been found in powder and capsule form. The use of this club drug has resulted in deaths from CNS depression and to synergistic effects when mixed with alcohol. It is also listed by the Drug Enforcement Administration as a predatory or date-rape drug. Its exact mechanism of action is unknown, but it has agonist activity at GABAB-receptors in the brain.
Opioids
The most commonly abused opioid street drug is heroin. This drug is prepared from morphine by the addition of acetyl groups, so structurally it is known as diacetylmorphine. Heroin is highly potent and water soluble and thus can be injected intravenously. Because it rapidly enters the brain following injection, heroin can produce an intense euphoric sensation called a rush. Long-term heroin users develop considerable drug tolerance and physical dependence, and they undergo a wide variety of withdrawal symptoms (see Table 25–3) if they abruptly discontinue their use of the drug (Box 25–1).
BOX 25-1 THE CASE OF THE OVERDOSED OPIOID ADDICT
CASE PRESENTATION
An 18-year-old male is brought to the emergency room in an unresponsive state with depressed respiration, pinpoint pupils, and cold, clammy skin. His pulse rate is 40 beats per minute. There are multiple needle tracks on both his arms. He is administered 2 mg of naloxone in an intravenous bolus and within minutes is sitting up and acting bellicose, complaining to the emergency room staff that they “ruined his high.”
CASE DISCUSSION
The needle tracks and the triad of apnea or depressed respiration, miosis (pinpoint pupils), and a comatose state indicate that the patient arrived at the hospital in an opioid overdose condition. Needle tracks in his arms suggest heroin use, although prescription opioids are also increasingly injected intravenously in opioid-dependent individuals. Naloxone is a pure opioid receptor antagonist and can quickly reverse the near-death condition of an opioid overdose, a phenomenon sometimes called the Lazarus effect, from the biblical story. As the elimination halflife of naloxone is sometimes shorter than the opioid that caused the overdose, patients may be given multiple doses of naloxone and monitored so that a relapse does not occur. It is recommended that patients who receive naloxone be continuously observed for a minimum of 2 hours after the last dose. It is not uncommon that the overdosed individual will be angry at the hospital staff for reversing the opioid effect, and naloxone may precipitate an opioid withdrawal syndrome.
Other opioids produce effects similar to those of heroin, but usually to a lesser degree. These effects vary with the potency and pharmacokinetic properties of the opioid and with the route of administration. Opioids administered orally tend to produce less euphoria and dependence than do opioids administered by other routes. For this reason, an orally administered drug such as methadone (see Chapter 23)can be used to prevent the craving for heroin as well as the opioid withdrawal reaction without causing significant reinforcement or exacerbating drug dependence. Oxycodone, in the slow-release formulation marketed as OxyContin, gained notoriety among street users because a dose intended for 24-hour pain relief in patients with chronic pain could be crushed and injected intravenously for a powerful rush. This has led to an increase in the number of deaths caused by opioid overdose. It is also a leading prescription abuse drug (see below).
CENTRAL NERVOUS SYSTEM STIMULANTS
The CNS stimulants include amphetamine, amphetamine derivatives, cocaine, caffeine, and nicotine. The amphetamine compounds and cocaine increase the synaptic concentration of norepinephrine and dopamine and exert sympathomimetic effects. They also induce a release of dopamine in the nucleus accumbens because this is the final common pathway for all chronically abused drugs and reinforced behaviors.
Amphetamine and Its Derivatives
Amphetamine and its derivatives increase the synaptic concentration of norepinephrine and dopamine by gaining entry into the presynaptic terminal through the reuptake transporter protein and releasing the catecholamines from vesicles. Amphetamine also facilitates the reverse transport of the catecholamines inside the terminal out through the reuptake transporter into the synapse. At high concentrations, amphetamine, but not all derivatives, can also inhibit monoamine oxidase and, by this second mechanism, can increase the levels of catecholamines.
The use of amphetamines produces a constellation of central and peripheral effects, including euphoria, insomnia, psychomotor stimulation, anxiety, loss of appetite, increased concentration, decreased fatigue, respiratory stimulation, and hyperthermia. It also produces sympathomimetic effects such as mydriasis, tachycardia, and hypertension. The euphoria and other reinforcing effects are caused by increased dopamine levels in the nucleus accumbens, whereas the jittery and anxious feelings produced by amphetamines primarily result from enhanced release of norepinephrine in the central and peripheral nervous systems.
The amphetamines, including methamphetamine, have legitimate medical indications such as attention-deficit/hyperactivity disorder (ADHD), narcolepsy and other sleep disorders, and obesity (see Chapter 22).
Methamphetamine
Amphetamine and methamphetamine are closely related sympathomimetic amines, and both are drugs of abuse. Of the two, methamphetamine is often preferred by abusers because it causes less norepinephrine to be released and can be more easily pyrolyzed (burned) and smoked. When methamphetamine free base is extracted by ether, pyrolyzed, and smoked, it is called ice or crystal meth. The euphoria produced by smoking “ice” is much greater than that produced by taking methamphetamine orally, presumably because of the faster rate at which dopamine levels are increased by inhaling the drug. The inexpensive cost and relative ease of making methamphetamine from precursor drugs found in nonprescription cold medicines enabled an illicit cottage industry in small-scale meth labs.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree