Otitis Media and Its Management
Otitis media (OM), defined as an inflammation of the middle ear, is the most prevalent disorder of childhood. The condition affects more than 75% of children by age 3 years and about 95% by age 12 years. In the United States OM is responsible for more than 16 million clinic visits a year.
OM may result from bacterial or viral infection or from noninfectious causes. Only bacterial OM responds to antibiotics. Furthermore, most cases resolve spontaneously, making antibiotics largely unnecessary—even when bacteria are the cause. Nonetheless, antibiotics have been used routinely. In fact, OM is the most common reason antibiotics are prescribed for children—at an estimated cost of $5 billion a year.
Acute Otitis Media
Characteristics, Pathogenesis, and Microbiology
Acute OM (AOM) is defined by infection, inflammation, and fluid in the middle ear. Otalgia (ear pain) is characteristic, often causing the young child to tug at or hold the affected ear. Other signs and symptoms accompanying AOM may include fever, vomiting, anorexia, irritability, sleeplessness, and diarrhea.
AOM results from a bacterial or viral infection of the middle ear. It occurs most commonly among children. The middle ear is filled with purulent fluid, which can cause the tympanic membrane to bulge outward. If the membrane is perforated, purulent otorrhea results.
AOM commonly develops after a viral upper respiratory infection, which can cause inflammation, swelling, and subsequent blockage of the eustachian tube. This results in negative pressure in the middle ear that, in turn, leads to fluid accumulation in the middle ear. When the eustachian tube opens, causing pressure equalization, bacteria and viruses can be sucked in. If the mucociliary system is sufficiently impaired, it will be unable to transport these pathogens back to the nasopharynx. OM results when bacteria colonize the fluid of the middle ear or when viruses colonize cells of the middle-ear mucosa. Common pathogens are provided in Table 86.1.
TABLE 86.1
Primary Pathogens Found in Fluid From the Middle Ear of Children With Acute Otitis Media
| Pathogen | Children With the Pathogen (%) |
| Streptococcus pneumoniae | 12 |
| Haemophilus influenzae | 56 |
| Moraxella catarrhalis | 22 |
| Others (e.g., Streptococcus pyogenes, Staphylococcus aureus, gram-negative bacilli) | Uncommon |
| No bacteria found | 10–30 |
| Both bacteria and viruses | 66 |
| Viruses alone* | 4 |
Diagnosis
To diagnose AOM, three elements must be present: (1) acute onset of signs and symptoms; (2) middle-ear effusion (MEE) or, if the tympanic membrane is ruptured, purulent otorrhea; and (3) middle-ear inflammation. The presence of MEE is indicated by limited mobility of the tympanic membrane on pneumatic otoscopy or tympanometry. (The best predictor of AOM is a bulging tympanic membrane.) Middle-ear inflammation is indicated by either (1) distinct erythema of the tympanic membrane or (2) distinct otalgia.
It is important to distinguish between AOM and otitis media with effusion (OME). As discussed later, children with OME have fluid in the middle ear but no signs of local or systemic illness. Prolonged OME is common after resolution of AOM.
Standard Treatment
All children with AOM should receive pain medication, and some should receive antibiotics. Prescribing antibiotics for all children should be discouraged because most (over 80%) of AOM episodes resolve spontaneously within a week. If antibiotics are prescribed routinely, most recipients will be taking drugs they don’t really need. Not only does this generate unnecessary expense, worse yet, it puts children at needless risk for adverse drug effects, increases their risk for recurrent AOM, and accelerates the emergence of antibiotic-resistant bacteria.
In 2013, the American Academy of Pediatrics (AAP) released guidelines for treating AOM in children. (See Fig. 86.2.) These build on earlier guidelines developed jointly by the AAP and the American Academy of Family Physicians. For many patients, the guidelines include an important option—observation—rather than immediate treatment with antibiotics. Observation is defined as management by symptomatic relief alone for 48 to 72 hours, thereby allowing time for AOM to resolve on its own. If symptoms persist or worsen, antibacterial therapy is then started. As part of this strategy, parents are informed about (1) the high probability of spontaneous AOM resolution and (2) the drawbacks of giving antibiotics when they are not needed. Observation is considered appropriate only when follow-up can be ensured. The recommendation for observation is based on studies showing the following:
• Most episodes of AOM resolve spontaneously.
• Immediate antibacterial therapy is only marginally superior to observation at causing AOM resolution and is no better at relieving pain or distress.
• Parents find the observation approach acceptable.
• Delaying antibacterial therapy does not significantly increase the risk for mastoiditis, which can occur when bacteria invade the mastoid bone.
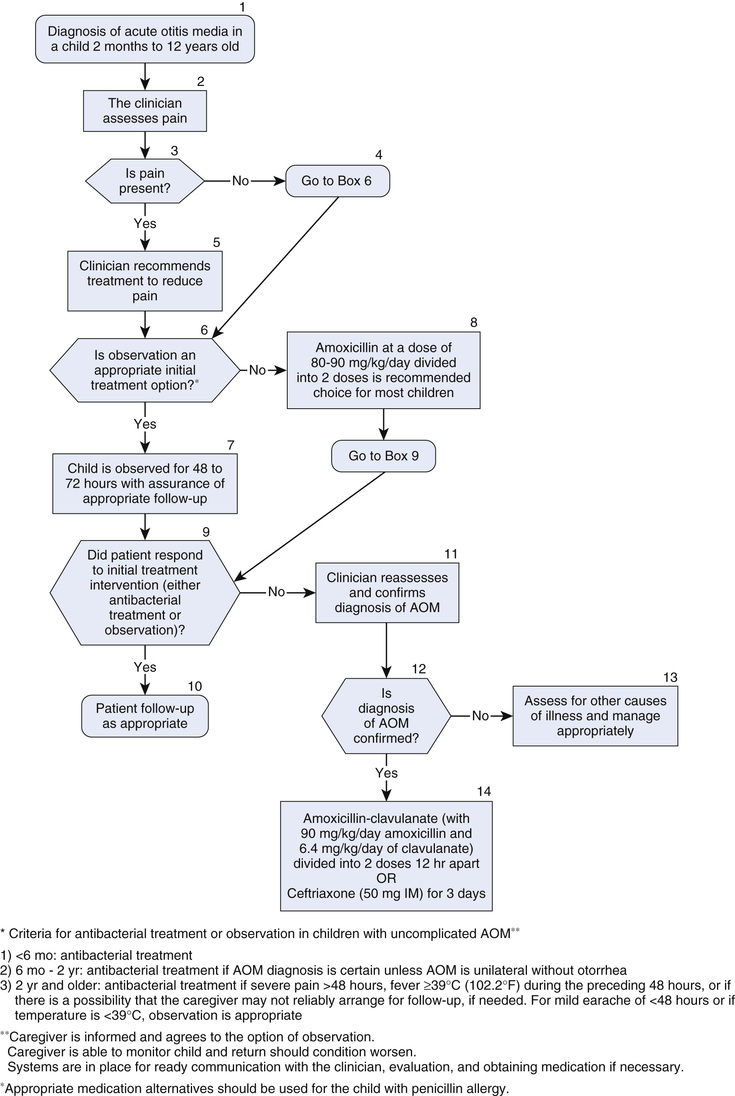
Criteria for choosing between observation and initial antibacterial therapy are shown in Table 86.2. As indicated, all children younger than 6 months should receive antibiotics, regardless of diagnostic certainty or symptom severity. Among children 6 months to 2 years old, antibiotics are indicated whenever the diagnosis is certain. For children 2 years and older, antibacterial therapy is indicated only if the diagnosis is certain, and then only if symptoms are severe. In all other cases, observation is the preferred strategy.
TABLE 86.2
Criteria for Choosing Initial Antibacterial Therapy Versus Observation in Children With Acute Otitis Media
| Age | Management Recommendation | |
| Certain Diagnosis | Uncertain Diagnosis | |
| Less than 6 months | Antibacterial therapy | Antibacterial therapy |
| 6 months to 2 years | Antibacterial therapy* | Antibacterial therapy if illness is severe; observation if illness is not severe† |
| 2 years and older | Antibacterial therapy if illness is severe; observation if illness is not severe† | Observation, regardless of symptom severity |
When antibacterial drugs are indicated, high-dose amoxicillin is the treatment of choice (Table 86.3). Benefits of amoxicillin are efficacy, safety, low cost, acceptable taste, and narrow microbiologic spectrum. The duration of treatment ranges from 5 to 10 days, depending on patient age and illness severity.
TABLE 86.3
Recommended Antibacterial Drugs for Acute Otitis Media
| Patient Group and Illness Severity | Recommended Drugs | |
| For Most Patients | For Patients With Penicillin Allergy* | |
| PATIENTS RECEIVING IMMEDIATE ANTIBIOTIC THERAPY | ||
| Nonsevere illness | Amoxicillin, 40–45 mg/kg twice daily | Non–type I allergy: Type I allergy: |
| Severe illness | Amoxicillin, 45 mg/kg twice daily plus clavulanate, 3.2 mg/kg twice daily† | Ceftriaxone, 50 mg/kg IM for 1 or 3 days |
| PATIENTS WITH PERSISTENT SYMPTOMS AFTER 48–72 HOURS OF OBSERVATION (WITH NO ANTIBIOTIC THERAPY) | ||
| Same as for patients receiving immediate antibiotic therapy | ||
| PATIENTS WITH PERSISTENT SYMPTOMS AFTER 48–72 HOURS OF ANTIBIOTIC THERAPY (INDICATING DRUG RESISTANCE) | ||
| Nonsevere illness | Amoxicillin, 45 mg/kg twice daily plus clavulanate, 3.2 mg/kg twice daily† | Non–type I allergy: Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|