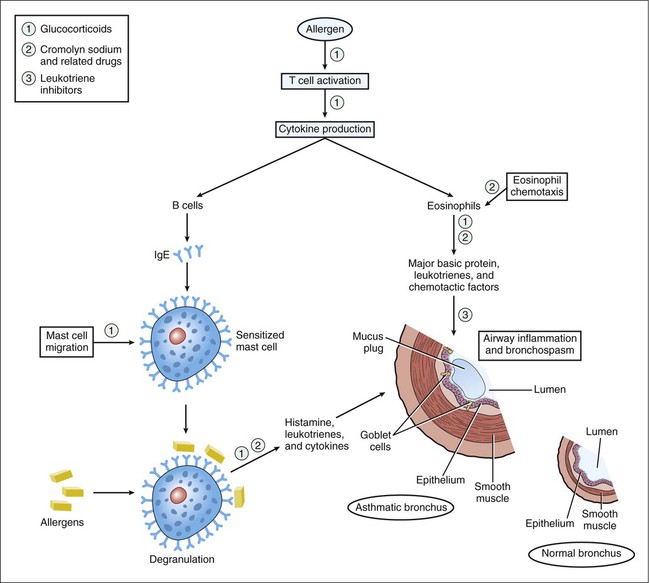
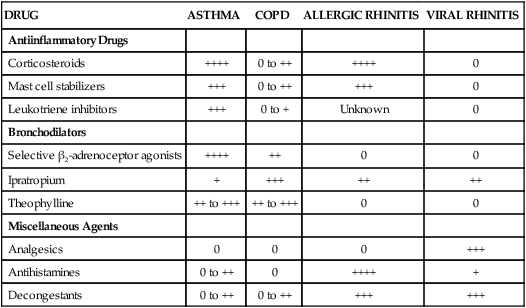
Asthma is characterized by airway inflammation and hyperresponsiveness to stimuli that produce bronchoconstriction. These stimuli include cold air, exercise, a wide variety of allergens, and emotional stress (see Box 27-1). The drugs used to treat asthma include antiinflammatory drugs and bronchodilators. The pathophysiology of asthma and sites of antiinflammatory drug action are illustrated in Figure 27-1. Table 27-1 shows the relative efficacy of various types of respiratory tract drugs, including those used in the treatment of allergic rhinitis and viral rhinitis. TABLE 27-1 Relative Efficacy of Antiinflammatory Drugs, Bronchodilators, and Miscellaneous Agents in the Management of Respiratory Tract Disorders* COPD, Chronic obstructive pulmonary disease (e.g., emphysema). *Ratings range from 0 (not efficacious) to ++++ (highly efficacious). Corticosteroids (glucocorticoids) are effective in the treatment of a wide variety of inflammatory and other diseases. The discussion here focuses on the use corticosteroids for asthma, allergic rhinitis, and COPD. The pharmacologic properties and clinical use of these drugs are described more completely in Chapter 33. The recognition that asthma is primarily an inflammatory disease has increased the role of corticosteroids in asthma therapy. For persons with moderate to severe asthma, steroids have become the cornerstone of therapy, and some patients with mild asthma may derive significant benefit from their use as well. Although corticosteroids are the most efficacious antiinflammatory drugs available for the treatment of both asthma and allergic rhinitis (see Table 27-1), they have the potential to cause a number of adverse effects if given systemically. The incidence of adverse effects is markedly reduced when these drugs are given by inhalation, so this route of administration is employed whenever possible. Systemic administration is usually reserved for the treatment of severe asthma or for short-term treatment of severe allergic rhinitis. Cromolyn sodium and related drugs are nonsteroidal compounds that stabilize the plasma membranes of mast cells and eosinophils and thereby prevent degranulation and release of histamine, leukotrienes, and other substances that cause airway inflammation (see Fig. 27-1). Hence, these drugs are often called mast cell stabilizers. Inhibition of mediator release by cromolyn and related drugs is thought to result from blockade of calcium influx into mast cells. Cromolyn and related drugs do not interfere with the binding of immunoglobulin E (IgE) to mast cells or with the binding of antigen to IgE. Their beneficial effects in asthma and other conditions are largely prophylactic.
Drugs for Respiratory Tract Disorders
Overview
Asthma
Rhinitis
DRUG
ASTHMA
COPD
ALLERGIC RHINITIS
VIRAL RHINITIS
Antiinflammatory Drugs
Corticosteroids
++++
0 to ++
++++
0
Mast cell stabilizers
+++
0 to ++
+++
0
Leukotriene inhibitors
+++
0 to +
Unknown
0
Bronchodilators
Selective β2-adrenoceptor agonists
++++
++
0
0
Ipratropium
+
+++
++
++
Theophylline
++ to +++
++ to +++
0
0
Miscellaneous Agents
Analgesics
0
0
0
+++
Antihistamines
0 to ++
0
++++
+
Decongestants
0 to ++
0 to ++
+++
+++
Antiinflammatory Drugs
Corticosteroids
Mast Cell Stabilizers
Cromolyn Sodium
Chemistry and Mechanisms
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Drugs for Respiratory Tract Disorders
Only gold members can continue reading. Log In or Register to continue