Because migraine is the most serious and common type of headache in patients afflicted with a headache disorder, it is the main focus of the discussion. The chapter closes with a brief review of treatment options for cluster and tension headaches.
CHARACTERISTICS AND PATHOGENESIS OF MIGRAINE HEADACHES
In the United States, approximately 24 million people suffer from migraine headaches (Box 29–1). The pathophysiological mechanisms of migraines are not completely understood, but migraine headaches appear to result from neurovascular dysfunction caused by an imbalance between excitatory and inhibitory neuronal activity at various levels in the central nervous system (CNS). This imbalance can be triggered by hormones, stress, fatigue, hunger, diet, or drugs.
BOX 29–1 THE CASE OF THE UNMITIGATING MIGRAINE
CASE PRESENTATION
A 26-year-old woman who suffers from frequent migraine headaches complains to her physician that the drug she has been taking to stop her migraine attacks is not working anymore. The physician looks in her medical record and tells her that he prescribed sumatriptan on her last visit a month ago, and that she may be tolerant to its effects. The physician talks to her about trying a drug to prevent migraine attacks as well as a new drug to abort migraines. She agrees to this new strategy and is prescribed valproate for migraine prevention and a new intranasal formulation of dihydroergotamine for aborting a migraine attack.
CASE DISCUSSION
Migraine is an extremely common condition which will affect 12% to 28% of people at some point. It is more common in women than men, with about 25% of adult women experiencing a migraine headache at least once a year, compared with less than 10% of men. Too-frequent use of an abortive agent for migraine headaches, such as sumatriptan, can lead to loss of effectiveness; another antimigraine agent can be administered which might be effective. In the case above, an ergot alkaloid, dihydroergotamine (DHE), which is now available in a convenient and rapid-acting nasal inhalation formulation, was prescribed. This class of drugs, however, carries potential risks for serious adverse effects, including isehemic conditions, and frequency of their use should be limited. Valproate is an antiseizure drug that is commonly used for migraine prophylaxis. It has an onset of action of a couple of weeks, which may be shorter than other agents used to prevent migraine attacks. Propranolol, a β-blocker, is also used to prevent the occurrence of migraine headaches, and its use in controlled clinical studies did not show tolerance in migraine sufferers who used it for at least six months.
About 15% of patients who have migraine headache disorder report that they experience an aura that precedes each headache attack and lasts for about 15 to 20 minutes. A visual aura can take the form of brightly flashing lights or rippling images that spread from the corner of the visual field (teichopsia). A sensory aura can take the form of paresthesias that involves the arm and face and tends to “march” sequentially from the fingers to the hand and then to the body. Auras are believed to result from the cerebral vasoconstriction and ischemia that precipitate migraine attacks. A migraine without an aura (previously known as a common migraine) is often accompanied by an attack of photophobia, phonophobia, nausea, or vomiting.
Each migraine attack has two phases. The first phase is characterized by cerebral vasoconstriction and ischemia. The release of serotonin from CNS neurons and circulating platelets contributes to this first phase. Hence, antiplatelet drugs and serotonin receptor antagonists are efficacious in the prevention of migraine headaches. The second phase, which is longer than the first one, is characterized by cerebral vasodilation and pain. The trigeminal neurovascular system appears to play a central role in the second phase. Neurons in the trigeminal complex release vasoactive peptides, including substance P and calcitonin gene-related peptide (CGRP). These peptides trigger vasodilation and inflammation of pial and dural vessels which, in turn, stimulate nociceptive fibers of the trigeminal nerve and cause pain. Figure 29–1 depicts these events and the mechanisms of drugs that are used to terminate migraine headaches.
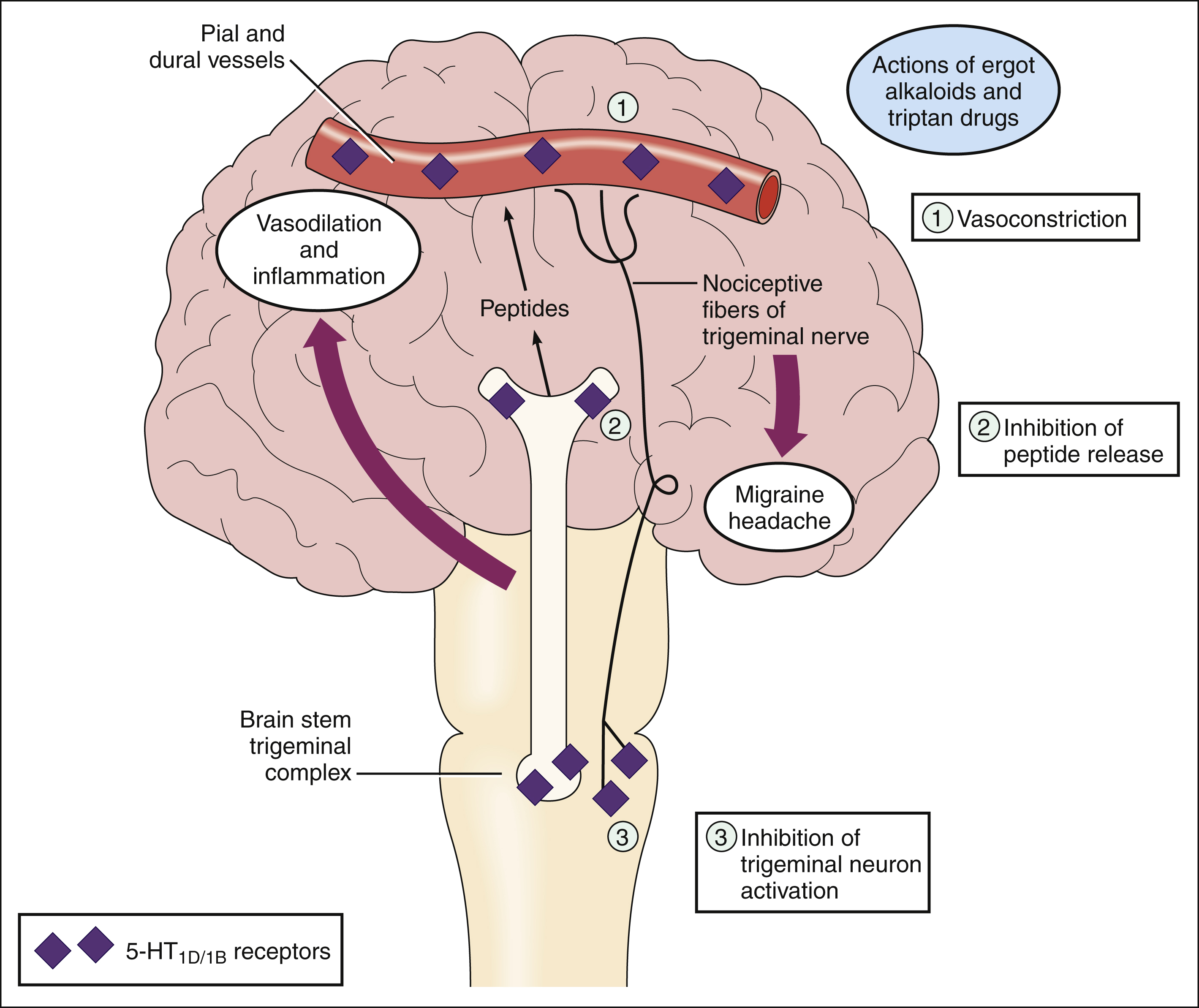
Figure 29–1 Mechanisms of ergot alkaloids and triptan drugs used in the treatment of migraine headache disorder. Migraine attacks are thought to result from trigeminal neurovascular dysfunction. When neurons in the trigeminal complex release peptides such as substance P and calcitonin gene-related peptide (CGRP), this causes vasodilation and inflammation of pial and dural vessels. These events activate nociceptive trigeminal fibers and cause the moderate to severe pain that is characteristic of migraine headaches. Ergot alkaloids and triptan drugs terminate the pain by activating serotonin 5-HT1B/1D receptors at several sites: (1) They activate receptors on pial and dural vessels and thereby cause vasoconstriction. (2) They activate presynaptic receptors to inhibit the release of peptides and other mediators from trigeminal neurons. (3) They activate receptors in the brain stem, which is believed to inhibit activation of trigeminal neurons responsible for migraine attacks.
DRUGS FOR MIGRAINE HEADACHES
The drugs used to manage patients with migraine headaches can be classified as prophylactic drugs and abortive (symptomatic) drugs. Many prophylactic drugs act by preventing the vasoconstrictive phase of the disorder, whereas abortive drugs reverse the vasodilative phase of migraine or relieve pain and inflammation.
Several drugs for migraine are antagonists or agonists at specific types of serotonin receptors. These receptors have been classified into four main types, 5-HT1 through 5-HT4.
The 5-HT2 receptors are widely distributed in the CNS, smooth muscle, and platelets, where they mediate vasoconstriction and platelet aggregation. Drugs that block 5-HT2 receptors, such as methysergide, can prevent the vasoconstrictive phase of migraine and are used as migraine prophylactics.
The 5-HT1 receptors are the predominant serotonin receptors in the CNS, and many of them function as presynaptic autoreceptors whose activation inhibits the release of serotonin and other neurotransmitters. The 5-HT1 receptors also mediate cerebral vasoconstriction. Drugs that activate these receptors, like sumatriptan, are used to terminate a migraine attack.
DRUGS FOR MIGRAINE PREVENTION
Numerous classes of drugs are used to prevent migraine headaches in persons who experience frequent attacks. These include anticonvulsants, antidepressants, anti-inflammatory drugs, β-adrenoceptor antagonists, calcium channel blockers, and serotonin-receptor antagonists. A trial of several different types of drugs may be useful to determine the most effective drug for a particular patient. Each drug requires several weeks of therapy before its effectiveness can be determined.
Anticonvulsants and Antidepressants
The properties of anticonvulsants and antidepressants are described in Chapters 20 and 22, respectively. Studies have shown that these two classes of drugs can prevent migraine in some patients, but the precise mechanisms underlying their effects are poorly understood.
Valproate (Divalproex) is the most widely used anticonvulsant for migraine prophylaxis. Its onset of efficacy (2–3 weeks) is somewhat shorter than that of other prophylactic drugs. Its common adverse effects include sedation, tremor, and weight gain.
Three types of antidepressants can be used to prevent migraine. The first consists of selective serotonin reuptake inhibitors (SSRIs), such as fluoxetine. The second consists of tricyclic antidepressants (TCAs). In this second group, tertiary amines such as amitriptyline are more potent inhibitors of serotonin reuptake and may be more effective in preventing migraine than are secondary amines such as desipramine. The third group consists of monoamine oxidase inhibitors (MAOIs), such as phenelzine. MAOIs can block serotonin degradation and are occasionally used in persons who fail to respond to other antidepressants.
Patients must take antidepressants for 3 to 4 weeks before the drugs become effective in preventing headaches, as is the case for alleviating the symptoms of depression. The inhibition of serotonin reuptake by the antidepressants leads to down-regulation of postsynaptic serotonin receptors and a compensatory increase in the firing rate of serotonin neurons. The relationship between these actions and migraine prophylaxis, however, is not clearly established.
Serotonin reuptake inhibitors sometimes cause anxiety, insomnia, tremor, anorexia, and sexual dysfunction. TCAs can cause drowsiness, tremor, and anticholinergic effects such as dry mouth, blurred vision, and urinary retention. MAOIs can cause a hypertensive crisis if they are taken with tyramine-containing foods or with sympathomimetic amine drugs (Chapter 22).
Nonsteroidal Anti-inflammatory Drugs
Nonsteroidal anti-inflammatory drugs (NSAIDs), including naproxen, can be used for the prevention and treatment of migraine. As discussed in Chapter 30, these drugs act by blocking thromboxane synthesis and platelet aggregation and thereby reducing the release of serotonin. NSAIDs can be used continuously or on an intermittent basis to prevent predictable headaches. For example, administration beginning 1 week before menses and continuing through menstruation may prevent migraine headaches associated with the menstrual cycle.
β-Adrenoceptor Antagonists
Of the various types of β-adrenoceptor antagonists that are available (see Chapter 9), only the β-blockers that lack intrinsic sympathomimetic activity are effective for the prevention of migraine headaches. One example of effective β-blockers is timolol. Another example, propranolol, is widely used for migraine prophylaxis but can cause more CNS side effects than timolol.
The mechanism of action of β-blockers in migraine prophylaxis is uncertain. These drugs may attenuate the second phase of migraine by blocking vasodilation mediated by β2-adrenoceptors. They may also reduce platelet aggregation and thereby decrease the release of serotonin from platelets.
Calcium Channel Blockers
Although verapamil and other calcium channel blockers are used for migraine prophylaxis, there is evidence that the calcium channel blockers are less effective in preventing migraine attacks than are other classes of drugs.
Calcium channel blockers may be effective in migraines by preventing the vasoconstrictive phase of migraine headaches. The properties of these drugs are described in Chapter 10.
5-HT2 Receptor Antagonists
Methysergide is a drug that blocks 5-HT2 receptors and thereby prevents the vasoconstrictive phase of migraine from occurring. Because of the potential toxicity of methysergide, however, other prophylactic drugs are usually chosen initially for migraine prophylaxis.
The drug is associated with a number of relatively mild adverse effects, including abdominal pain, weight gain, and hallucinations. It is also associated with a risk of life-threatening retroperitoneal, pleural, and cardiac valve fibrosis. For this reason, it should not be used longer than 6 months without a drug-free period of one month that begins with a 2-week period of decreasing dosage. Serum creatinine measurements should be monitored and a chest x-ray taken periodically to detect early signs of fibrosis in patients treated with methysergide.
Other Agents for Migraine Prevention
Gabapentin is an agent approved for the treatment of seizure disorders (see Chapter 20) and postherpetic neuralgia. It is moderately effective with little adverse effects in preventing occurrence of migraines. Although gabapentin is known to enhance γ-aminobutyric acid (GABA) action in the treatment of seizure disorder, its actions in migraine treatment are unclear.
The result of a double-blind, placebo-controlled study of patients with migraines showed that riboflavin (vitamin B2) can significantly reduce the frequency and duration of migraine attacks. This study found that a daily dose of riboflavin at 400 mg produced a significant decrease in the number of migraine attacks as well as the total days with headache pain. The effect was not evident until after 2 months of administration, however, and the mechanism of action is unknown.
Feverfew is an herbal remedy that has low to moderate efficacy in preventing migraines with little side effects. It is available without a prescription as a combination of the extracts of Pyrethrum parthenium (feverfew) and Zingiber officinale (ginger) in a rapidly dissolving formulation. The active ingredient in feverfew is parthenolide, which has anti-inflammatory activity. As with NSAIDs, parthenolide may prevent inflammation associated with migraine headaches.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


