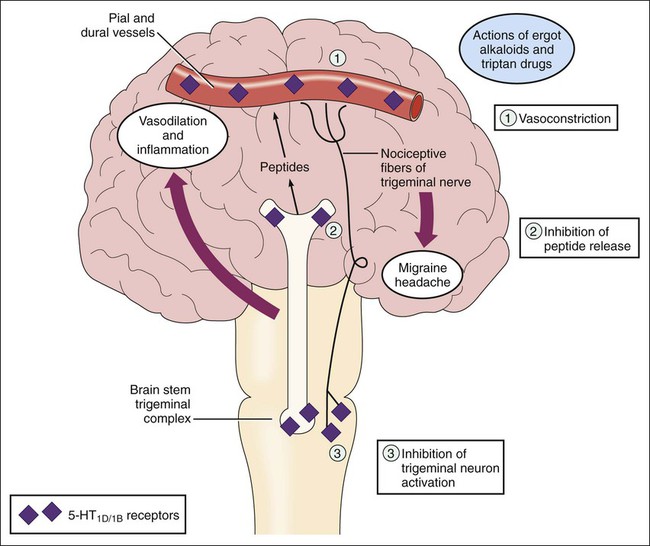
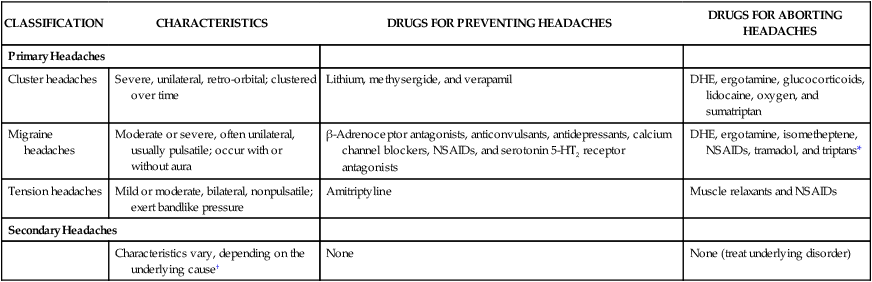
An occasional headache for most people is easily remedied by a couple of aspirin or ibuprofen pills and a glass of water. However, for many people, headaches are unremitting, severe, and recurring. The International Headache Society divides headache disorders into two large groups. The first group, primary headache disorders, includes cluster, migraine, and tension headaches. The characteristics and management of these three types of headaches, which together account for about 95% of all headaches, are compared in Table 29-1. The second group, secondary headache disorders, consists of headaches that arise from organic disorders (e.g., hemorrhage, infection, neuropathy, stroke, and tumor). In patients with secondary headaches, management focuses on treating the underlying disorder. TABLE 29-1 Classification and Pharmacologic Management of Headache Disorders DHE, Dihydroergotamine; NSAIDs, Nonsteroidal antiinflammatory drugs. *Triptans include naratriptan, rizatriptan, sumatriptan, and zolmitriptan. †Examples of causes are hemorrhage, infection, neuropathy, stroke, and tumor. In the United States, approximately 24 million people experience migraine headaches (Box 29-1). The pathophysiologic mechanisms of migraines are not completely understood, but migraine headaches appear to result from neurovascular dysfunction caused by an imbalance between excitatory and inhibitory neuronal activity at various levels in the central nervous system (CNS). This imbalance can be triggered by hormones, stress, fatigue, hunger, diet, or drugs. Each migraine attack has two phases. The first phase is characterized by cerebral vasoconstriction and ischemia. The release of serotonin from CNS neurons and circulating platelets contributes to this first phase. Hence, antiplatelet drugs and serotonin receptor antagonists are efficacious in the prevention of migraine headaches. The second phase, which is longer than the first one, is characterized by cerebral vasodilation and pain. The trigeminal neurovascular system appears to play a central role in the second phase. Neurons in the trigeminal complex release vasoactive peptides, including substance P and calcitonin gene-related peptide (CGRP). These peptides trigger vasodilation and inflammation of pial and dural vessels, which in turn stimulate nociceptive fibers of the trigeminal nerve and cause pain. Figure 29-1 depicts these events and the mechanisms of drugs that are used to terminate migraine headaches.
Drugs for Headache Disorders
Overview
CLASSIFICATION
CHARACTERISTICS
DRUGS FOR PREVENTING HEADACHES
DRUGS FOR ABORTING HEADACHES
Primary Headaches
Cluster headaches
Severe, unilateral, retro-orbital; clustered over time
Lithium, methysergide, and verapamil
DHE, ergotamine, glucocorticoids, lidocaine, oxygen, and sumatriptan
Migraine headaches
Moderate or severe, often unilateral, usually pulsatile; occur with or without aura
β-Adrenoceptor antagonists, anticonvulsants, antidepressants, calcium channel blockers, NSAIDs, and serotonin 5-HT2 receptor antagonists
DHE, ergotamine, isometheptene, NSAIDs, tramadol, and triptans*
Tension headaches
Mild or moderate, bilateral, nonpulsatile; exert bandlike pressure
Amitriptyline
Muscle relaxants and NSAIDs
Secondary Headaches
Characteristics vary, depending on the underlying cause†
None
None (treat underlying disorder)
Characteristics and Pathogenesis of Migraine Headaches
< div class='tao-gold-member'>
Drugs for Headache Disorders
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree